ORIF with trochanteric flip osteotomy offers optimal exposure for precise reduction and fixation in complex femoral head fractures with early mobilization with delayed weight-bearing is essential in post-operative management to support healing and functional recovery.
Dr. Akshay D Punekar, Department of Orthopedics, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India. E-mail: drakshaypunekar@gmail.com
Introduction: Pipkin Type III femoral head fractures, characterized by dislocation and concurrent fractures of the femoral head-and-neck, present significant challenges due to the risk of avascular necrosis (AVN) and post-traumatic osteoarthritis. Open reduction and internal fixation (ORIF) using surgical hip dislocation with trochanteric flip osteotomy has been proposed as a viable option, enabling optimal exposure of the femoral head and acetabulum while potentially minimizing complications.
Case Report: We report a case of a 40-year-old male presenting with a right hip dislocation and a Pipkin Type III femoral head-and-neck fracture. ORIF was performed with a surgical hip dislocation and trochanteric flip osteotomy, followed by fixation using 3.5 mm Herbert screws. Post-operative rehabilitation involved immediate early range of motion exercises, with delayed weight-bearing initiated at 6–8 weeks. Radiographs at regular intervals of 6, 12, 18 and 24 months showed no signs of AVN or arthritis, with gradual onset osteoarthritic changes appearing from 2.5-years post-operative.
Conclusion: This case underscores the efficacy of ORIF with trochanteric flip osteotomy for Pipkin Type III fractures, offering functional outcomes comparable to other methods. This technique is associated with higher heterotopic ossification rates but may reduce the risk of AVN, early-onset arthritis relative to alternative methods and delay in requirement of hip replacement surgery. Despite a mild-to-moderate progression of osteoarthritis by the 3rd year of follow-up, the patient reported minimal hip pain until this time, highlighting the durability of this approach.
Keywords: Pipkin type III fracture, femoral head fracture, trochanteric flip osteotomy, avascular necrosis, hip dislocation, osteoarthritis.
Pipkin Type III femoral head fractures are rare, high-energy injuries, accounting for <1% of all hip fractures [1]. They involve concurrent fractures of the femoral head-and-neck, often accompanied by hip dislocation these injuries present unique challenges due to the risk of avascular necrosis (AVN) and post-traumatic osteoarthritis, especially in cases with delayed diagnosis or treatment [2]. The femoral head-and-neck fractures impede vascular supply, increasing susceptibility to AVN, which is reported in 25–50% of cases, even with early intervention [3]. Conventional management approaches, including closed reduction and conservative fixation, have shown limited success in these fractures, often resulting in suboptimal outcomes due to inadequate exposure of the femoral head, making reduction and stable fixation challenging [4]. Among various surgical techniques, open reduction and internal fixation (ORIF) with a surgical hip dislocation and trochanteric flip osteotomy has emerged as a viable option for managing these complex injuries. First popularized by Ganz et al., this approach allows for optimal visualization and access to the femoral head and acetabulum, improving the accuracy of reduction and fixation while preserving blood supply [5]. Despite these advantages, trochanteric flip osteotomy is associated with complications, particularly heterotopic ossification (HO), reported in 10–20% of cases, potentially impacting long-term hip mobility and function [6]. However, it may reduce the risk of AVN and delay the progression to hip replacement surgery, especially when managed with careful post-operative rehabilitation protocols. This case report details the successful application of ORIF with surgical hip dislocation and trochanteric flip osteotomy in a 40-year-old male with a Pipkin Type III femoral head-and-neck fracture. By highlighting the challenges and outcomes associated with this approach, this report aims to contribute to the limited literature on Pipkin Type III fractures and underscore the importance of a comprehensive surgical and rehabilitation strategy in optimizing patient outcomes.
A 40-year-old male patient presented to the emergency department with acute right hip pain and inability to bear weight following a high-energy motor vehicle accident. Physical examination revealed a shortened, externally rotated right lower limb with marked tenderness over the hip region. Neurovascular examination of the limb was intact, with no distal deficits. The patient had no significant medical history, no known allergies, and no prior surgeries or fractures. Initial radiographs and CT imaging confirmed a posterior hip dislocation with a Pipkin Type III femoral head-and-neck fracture (Fig. 1). The severity of the fracture, coupled with the dislocation, placed him at a high risk for AVN and post-traumatic osteoarthritis. Given the complexity of the injury and high risk of AVN, the patient was scheduled for surgery and underwent ORIF with surgical hip dislocation and trochanteric flip osteotomy within 48 h of trauma (Fig. 2).
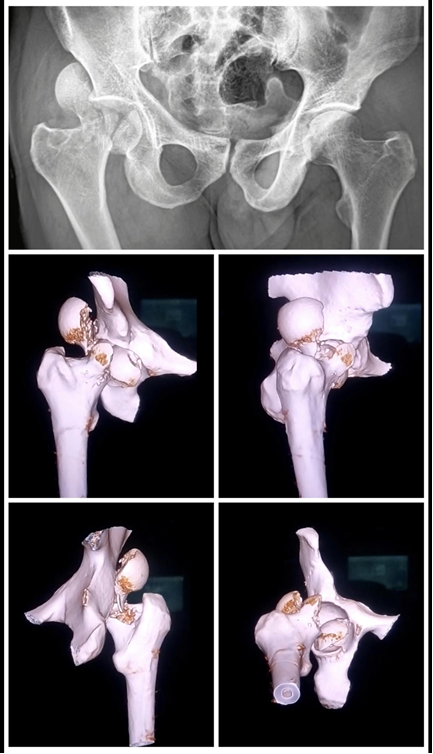
Figure 1: Pre-operative imaging of the affected hip showing anteroposterior radiograph and 3D computed tomography reconstruction delineating the femoral head pathology and acetabular involvement.
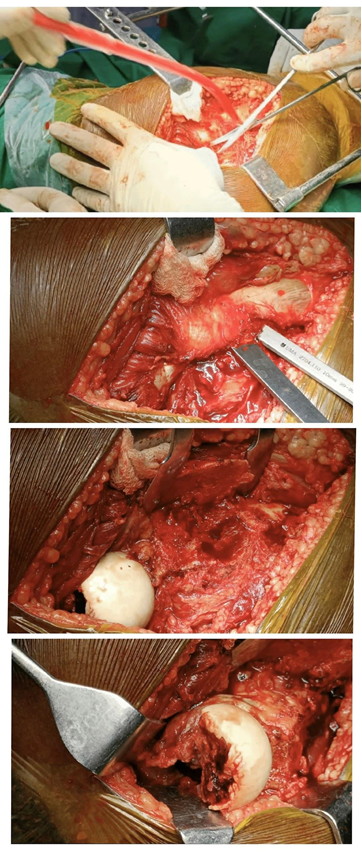
Figure 2: Intraoperative illustration demonstrating the surgical exposure of the femoral head through a trochanteric flip osteotomy, performed through the Gibson interval.
Operative procedure
The technique allowed adequate exposure of the femoral head and acetabulum, enabling a precise reduction and stable fixation. Intraoperatively, a periacetabular capsulotomy was performed to preserve the blood supply to the femoral head and minimize AVN risk. The fracture was stabilized using six 3.5 mm Herbert screws – two directed through the femoral head fragments and four across the femoral head into the femur neck. Despite careful screw placement, one screw head was noted to be marginally protruding into the joint space on post-operative imaging. The positioning was not deemed to compromise joint articulation significantly at the time; however, the patient was advised on close monitoring for mechanical symptoms or degenerative progression.
Post-operative rehabilitation
The patient was enrolled in a structured rehabilitation program. Immediate post-operative management included early mobilization with assisted range-of-motion exercises to prevent stiffness and promote healing. Full weight-bearing on the affected limb was strictly avoided to protect the fixation. Hip rotation (both internal and external) was restricted to avoid stressing the repair site. Weight-bearing on the affected limb was delayed for 6–8 weeks to ensure adequate healing of the fracture and minimize stress on the fixation. Gradual strengthening exercises, focusing on the quadriceps and hip abductors, were introduced as tolerated to optimize recovery and support functional outcomes. The patient was instructed to avoid high-impact activities, such as running or jumping, to prevent joint stress. Movements involving high rotational forces on the hip were still restricted to reduce the risk of hardware loosening or soft tissue strain.
Follow-up
Routine radiographic follow-ups at 6, 12, 18, and 24 months showed satisfactory alignment and healing of the fracture, with no signs of AVN or early arthritis during this period. The patient was pain-free and functional, with gradual osteoarthritic changes only observed starting 2.5 years post-operatively (Fig. 3). Harris hip score (HHS) at intervals of 6, 12, 18, and 24 months, and again at 2.5 years post-operatively were 85, 90, 90, 88, 80 suggesting pain-free movement and “excellent” range of motion by 1-year follow-up and a gradual decrease to “good” functionality with mild hip pain related to progressive osteoarthritis, but without significant impairment in daily activities [7]. Since his HHS has decreased to 80, though still allowing him to manage daily tasks independently. Imaging reveals mild-to-moderate osteoarthritic changes in the hip joint, signifying the early stages of arthritis setting in. Although his range of motion remains largely unaffected, there is a slight decrease in hip flexion and abduction strength, likely due to the degenerative changes. The patient has been advised to avoid high-impact activities and continue with low-impact strengthening exercises to help manage symptoms and slow arthritis progression.
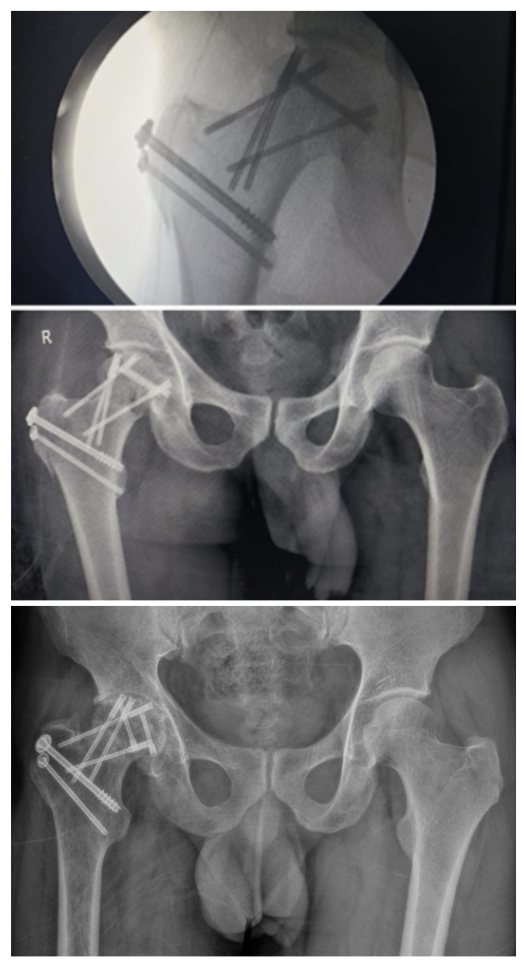
Figure 3: Serial radiographs of the hip: Intraoperative fluoroscopy, 6-month follow-up, and 2.5-year follow-up images illustrating progressive mild–to-moderate osteoarthritic changes in the hip joint.
Ethical considerations
Informed consent was obtained from the patient for the publication of this case report, including the use of anonymized clinical data and images. The patient was informed about the purpose of this report and agreed to share his medical information to contribute to the medical literature on Pipkin Type III femoral head fractures.
Pipkin Type III fractures are rare, complex injuries that pose significant treatment challenges due to the risk of AVN and post-traumatic osteoarthritis, especially when there is hip dislocation and disruption of blood supply to the femoral head [8]. ORIF using a surgical hip dislocation and trochanteric flip osteotomy was selected for this patient due to its ability to achieve optimal exposure, precise reduction, and stable fixation. The Ganz surgical hip dislocation approach, first popularized by Ganz et al., allows full visualization of the femoral head, neck, and acetabulum while preserving the femoral head’s blood supply, thereby reducing AVN risk. This approach is particularly suited to younger, active patients, as it minimizes damage to the surrounding soft tissue, preserves hip stability, and avoids immediate arthroplasty. In this case, fixation was favored over arthroplasty due to the patient’s age and activity level. Hip replacement is typically reserved for older patients or those with advanced joint degeneration, as it introduces risks of early wear and revision surgery in younger patients. Surface arthroplasty, although an option, may not provide the same stability in complex fractures involving both the femoral head-and-neck. ORIF with screw fixation offers the advantage of preserving the patient’s natural anatomy and delaying the need for hip replacement, which is especially valuable in younger patients who would benefit from retaining native joint function as long as possible. Literature suggests that fixation in such cases can effectively postpone or reduce the risk of early-onset osteoarthritis and total hip arthroplasty [9]. Ideally, serial magnetic resonance imaging (MRI) would be used post-operatively to assess early AVN through T1-weighted signal loss, double-line signs on T2/short-tau inversion recovery sequences, and absence of contrast enhancement in the femoral head [10]. However, in this case, post-operative MRI could not be reliably performed due to significant magnetic susceptibility artefacts caused by the multiple metallic Herbert screws [11]. In the absence of MRI, serial radiographs were used to monitor femoral head integrity. Up to 2.5-years post-operatively, there was no radiographic evidence of femoral head collapse, sclerosis, or subchondral crescent sign. Clinically, the patient remained pain-free for over 2 years, with a gradual decline in HHS to 80, correlating with the emergence of mild-to-moderate osteoarthritic changes. Reliance on serial radiographs may have missed subtle or early-stage ischemic changes, reducing the sensitivity of AVN assessment. In addition, the presence of a marginally protruding intra-articular screw, although not symptomatic initially, may have contributed to early cartilage wear and degenerative changes. This confounds the interpretation of whether degeneration was implant-related or due to natural disease progression. Although the patient has started to experience some mild arthritis-related symptoms, this outcome compares favorably with studies showing that ORIF using trochanteric flip osteotomy can delay the need for hip replacement and minimize joint deterioration in the early years post-surgery. Literature supports ORIF with trochanteric flip osteotomy as a viable option for managing Pipkin Type III fractures, particularly in younger patients where joint preservation is preferred. Studies indicate that this approach, while associated with certain complications, such as HO, results in improved functional outcomes and delays in the progression of arthritis. However, the trochanteric flip osteotomy approach has shown efficacy in preserving blood flow to the femoral head, reducing AVN rates relative to other methods. Despite the advantages of ORIF with surgical hip dislocation, this approach carries certain risks, such as AVN, HO, arthritis, hardware complications and joint stiffness [12]. Adhering to a structured rehabilitation protocol, as in this case, is essential for preserving range of motion and functional outcomes. While ORIF with trochanteric flip osteotomy provides a promising option for Pipkin Type III fractures, it is a technically demanding procedure requiring specialized surgical expertise. This approach is also associated with specific risks, as mentioned, and requires diligent follow-up to monitor for complications, such as HO and arthritis. In addition, while fixation can postpone the need for arthroplasty, it may not eliminate the long-term risk of joint degeneration, especially in cases where mild arthritis has already begun to set in. We are limited by assessment of early and mid-term outcomes with the patient follow-up of 2.5–3 years, the long-term risk of advanced osteoarthritis or eventual conversion to arthroplasty beyond 5–10 years remains unknown. Another limitation is the absence of a comparative arm to conclude the superiority of ORIF with trochanteric flip osteotomy over other approaches, particularly in older or lower-demand patients. Further longer duration follow-up comparative studies are necessary to confirm the reproducibility of these outcomes since the present report is limited by its single-case design.
This case underscores the potential efficacy of ORIF with surgical hip dislocation and trochanteric flip osteotomy for managing Pipkin Type III femoral head fractures, especially in younger patients, where preserving hip function is essential. By enabling optimal exposure, precise reduction, and stable fixation, this technique offers a reliable alternative to early arthroplasty. Despite mild osteoarthritic progression, the patient remained pain-free and functional for over 2 years, highlighting the durability of this approach. The case is significant as it supports the use of ORIF with trochanteric flip osteotomy in the management of high-risk femoral head fractures. This approach offers a promising balance between preserving hip function and minimizing complications, such as AVN and early-onset osteoarthritis, making it a valuable contribution to orthopedic management in trauma cases where hip preservation is preferred. Long-term follow-up is essential in such cases to monitor for progressive arthritis, AVN, and other complications, as early detection and intervention can help manage symptoms and potentially delay the need for hip replacement.
This case demonstrates that ORIF with surgical hip dislocation and trochanteric flip osteotomy is an effective option for managing complex Pipkin Type III femoral head fractures. The approach provides reliable access and fixation while minimizing the risk of avascular necrosis and delaying the need for hip arthroplasty, making it a valuable alternative for preserving joint function in younger, active patients.
References
- 1. Giannoudis PV, Kontakis G, Christoforakis Z, Akula M, Tosounidis T, Koutras C. Management, complications and clinical results of femoral head fractures. Injury 2009;40:1245-51. [Google Scholar] [PubMed]
- 2. Matthews AH, Davis DD, Fish MJ, Stitson D. Avascular Necrosis. Treasure Island, FL: StatPearls Publishing; 2020. [Google Scholar] [PubMed]
- 3. Barney J, Piuzzi NS, Akhondi H. Femoral Head Avascular Necrosis. Treasure Island, FL: StatPearls Publishing; 2019. [Google Scholar] [PubMed]
- 4. Peng SH, Wu CC, Yu YH, Lee PC, Chou YC, Yeh WL. Surgical treatment of femoral head fractures. Biomed J 2020;43:451-7. [Google Scholar] [PubMed]
- 5. Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. The Journal of Bone and Joint Surgery British Volume 2001 Nov 1;83(8):1119–24. [Google Scholar] [PubMed]
- 6. Gupta S, Singh J, Virk JS. The role of trochanteric flip osteotomy in fixation of certain acetabular fractures. Chin J Traumatol 2017;20:161-5. [Google Scholar] [PubMed]
- 7. Nilsdotter A, Bremander A. Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (A. Arthritis Care & Research. 2011 Nov;63(S11):S200–7. [Google Scholar] [PubMed]
- 8. Keong MW, Razak HR, Koon WM, Ping CC. Case report of a rare pipkin type III femoral head fracture. J Orthop Case Rep 2019;9:11-5. [Google Scholar] [PubMed]
- 9. Stibolt RD Jr., Patel HA, Huntley SR, Lehtonen EJ, Shah AB, Naranje SM. Total hip arthroplasty for posttraumatic osteoarthritis following acetabular fracture: A systematic review of characteristics, outcomes, and complications. Chin J Traumatol 2018;21:176-81. [Google Scholar] [PubMed]
- 10. Karantanas AH, Drakonaki EE. The role of MR imaging in avascular necrosis of the femoral head. Semin Musculoskelet Radiol 2011;15:281-300. [Google Scholar] [PubMed]
- 11. Farshad-Amacker NA, Koff MF, Dyke JP, Lazaro LE, Shah P, Lorich DG, et al. Assessment of osteonecrosis in the presence of instrumentation for femoral neck fracture using contrast-enhanced MAVRIC sequence. HSS J 2016;12:51-8. [Google Scholar] [PubMed]
- 12. Punzi L, Galozzi P, Luisetto R, Favero M, Ramonda R, Oliviero F, et al. Post-traumatic arthritis: Overview on pathogenic mechanisms and role of inflammation. RMD Open 2016;2:e000279. [Google Scholar] [PubMed]