● Epidural steroid injections are effective in reducing pain and disability in lumbar disc herniation. ● The transforaminal route gives the best results by directly targeting the affected nerve root. ● Route selection should be based on patient factors and safety considerations, with fluoroscopy improving accuracy.
Dr. Rahul Yadav, Department of Orthopaedics, SGT Medical College and Research Institute, Gurugram, Haryana, India. E-mail: rahulyadav.medical@gmail.com
Introduction: Lumbar prolapsed intervertebral disc (PIVD) is a prevalent cause of radicular pain and functional impairment. Epidural steroid injections are an established non-surgical treatment option. This study compares the efficacy of caudal, transforaminal, and interlaminar routes for methylprednisolone delivery.
Objectives: To evaluate and compare the analgesic and functional outcomes of different ESI routes in managing lumbar PIVD.
Materials and Methods: In this prospective, randomized study, 75 patients aged 25–75 years with magnetic resonance imaging -confirmed single-level PIVD and refractory symptoms were allocated to one of three intervention groups: Caudal, transforaminal, or interlaminar ESI (n = 25 each). All patients received methylprednisolone acetate injections under fluoroscopic guidance. Pain and function were assessed using the Visual Analog Scale (VAS) and Oswestry Disability Index (ODI) at baseline, 1, 2, and 4 weeks, and at 3 months post-intervention.
Results: All groups showed significant reductions in VAS and ODI scores over time (P < 0.001). At 3 months, the transforaminal group had the greatest improvement (VAS: 0.72 ± 1.1; ODI: 2.92 ± 4.61), followed by caudal and interlaminar routes. Analysis of variance and post hoc analysis confirmed the superiority of the transforaminal approach (P < 0.001).
Conclusion: Transforaminal ESI with methylprednisolone provides superior pain relief and functional recovery compared to caudal and interlaminar routes. Route selection should consider anatomical precision and patient-specific factors.
Keywords: Lumbar disc prolapse, epidural steroid injection, methylprednisolone, caudal, transforaminal, interlaminar, radiculopathy, Visual Analog Scale, Oswestry Disability Index, fluoroscopy.
Low back pain (LBP) remains a leading cause of disability worldwide and is particularly prevalent in India due to sedentary lifestyles and limited access to early interventions [1]. Lumbar disc herniation is a common etiology of LBP, where the nucleus pulposus protrudes through the annulus fibrosus, compressing spinal nerve roots and resulting in radiculopathy, pain, and neurological deficits [2,3].
Non-surgical interventions, including non-steroidal anti-inflammatory drugs, physiotherapy, and muscle relaxants, are often used but can be inadequate for persistent cases [4,5,6]. Epidural steroid injections (ESIs) offer targeted anti-inflammatory action to reduce pain and disability. Methylprednisolone is commonly used due to its efficacy and safety profile [7,8,9]. The route of administration – caudal, transforaminal, or interlaminar – plays a crucial role in clinical outcomes. Caudal ESI is technically simple with fewer risks but provides diffuse medication spread [10,11]. Transforaminal injections target the affected nerve root directly, leading to faster relief but with a higher risk profile [12,13]. Interlaminar ESI allows posterior epidural access near the affected disc level, balancing safety and efficacy [14]. This study compares these three approaches in patients with single-level lumbar prolapsed intervertebral disc (PIVD) who failed conservative therapy, with outcomes assessed using the Visual Analog Scale (VAS) and Oswestry Disability Index (ODI).
This prospective, randomized clinical study was conducted in the Department of Orthopaedics at SGT Medical College and Hospital, Budhera, Gurgaon. Institutional Ethical Committee approval was obtained (IEC/FMHS/MD/MS/2023–31), and informed consent was secured from all participants.
Study design and participants
A total of 75 patients, aged 25–75 years, diagnosed with magnetic resonance imaging (MRI)-confirmed single-level lumbar PIVD, and refractory to at least 6 weeks of conservative treatment, were enrolled. Using IBM Statistical Package for the Social Sciences (SPSS) v23, participants were randomized equally into three intervention groups of 25 each.
Inclusion criteria
- Patients aged 18–75 years old
- Diagnosis of single disc herniation(protrusion and extrusion) through MRI
- Failure of at least 6 weeks of conservative treatment
- Previously diagnosed as PIVD
- No past history of lumbar surgery.
Exclusion criteria
- Migrated or sequestrated herniation on imaging
- Diagnosis of multiple-level disc herniation through MRI
- Motor deficit
- Cauda Equina Syndrome
- Segmental instability
- Spinal canal stenosis
- Medical problems that contraindicate the procedure
- History of allergic reaction to local anesthetics or corticosteroids
- Psychogenic disorders, tumors, malformation deformities, post-traumatic root compression, or infectious etiologies.
The injection procedure was tailored based on the route of administration: Caudal, interlaminar, or transforaminal. Each technique was performed under sterile conditions with fluoroscopic guidance to ensure accurate needle placement and delivery of the medication.
Caudal epidural injection
For the caudal route, patients were positioned prone on the procedure table with a pillow placed under their abdomen to reduce lumbar lordosis. The sacral cornua were identified through palpation, and the skin overlying the sacral hiatus was cleaned thoroughly with povidone-iodine and alcohol-based solutions. Sterile draping was applied. A 1 mL injection of 2% lignocaine was administered for local anesthesia at the puncture site. Using an 18G lumbar puncture needle with a stylet, the needle was inserted at an angle of approximately 30° into the sacral hiatus. The needle was carefully advanced into the sacral canal under continuous fluoroscopic guidance, ensuring its tip was correctly positioned without penetrating the dura mater. Once the position was confirmed with anteroposterior (AP) and lateral fluoroscopic views, a test injection of contrast dye (1–2 mL) was administered to confirm epidural spread and rule out intravascular or intrathecal placement. The therapeutic injection comprised a mixture of 6 mL of normal saline, 2 mL of 2% xylocaine, and 80 mg (2 mL) of methylprednisolone acetate (Fig. 1).
Transforaminal epidural injection
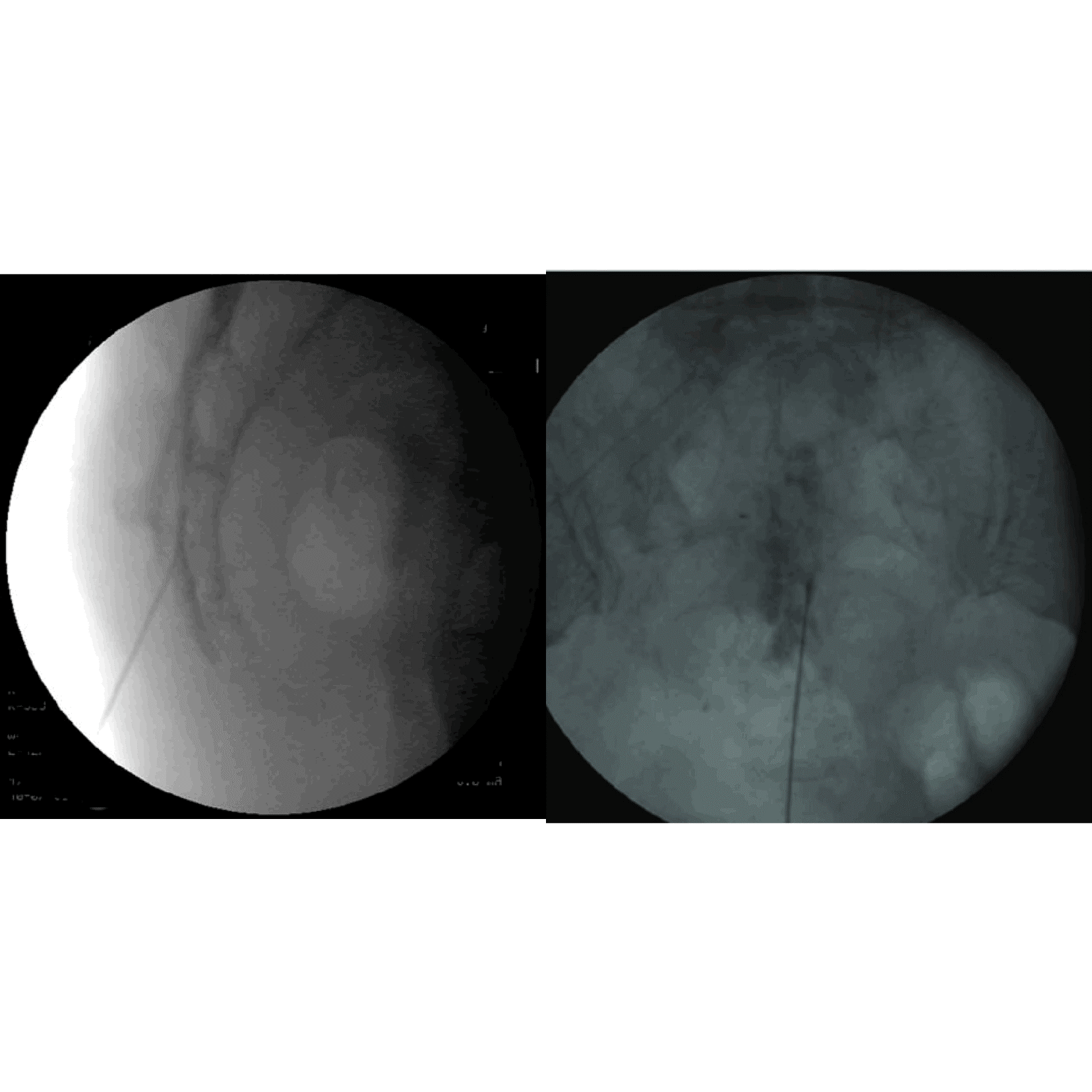
For the transforaminal route, patients were positioned prone on a radiolucent table, and the area was cleaned with povidone-iodine and alcohol, followed by sterile draping. The affected nerve root level was identified using fluoroscopy. Under oblique fluoroscopic guidance, the needle insertion site was marked at the eye of the “Scotty dog,” corresponding to the target neural foramen. After administering 1 mL of 2% lignocaine for local anesthesia, a 22G spinal needle was inserted at a 30–45° angle toward the foramen. The needle was advanced under continuous fluoroscopic guidance, with adjustments made using both oblique and lateral views. Once the needle tip reached the posterior aspect of the foramen, a test injection of 0.5–1 mL of contrast dye was administered to confirm proper epidural spread and avoid intravascular placement. The therapeutic injection consisted of 1 mL of 2% xylocaine and 1 mL (40 mg) of methylprednisolone acetate (Fig. 2).
The rationale for using 40 mg of methylprednisolone acetate instead of 80 mg, as administered in caudal or interlaminar epidural injections, is based on the precision and localized nature of the transforaminal technique. Since transforaminal injections target the nerve root directly within the neural foramen, a lower dose is sufficient to achieve therapeutic effects at the site of inflammation while minimizing systemic exposure. In addition, the lower dose reduces the risk of complications, such as chemical irritation or vascular compromise, which are more significant in this route due to its proximity to segmental arteries. This dose adjustment is further supported by evidence demonstrating that 40 mg is effective for localized radicular pain without added benefit from higher doses in the transforaminal approach.
Interlaminar epidural injection
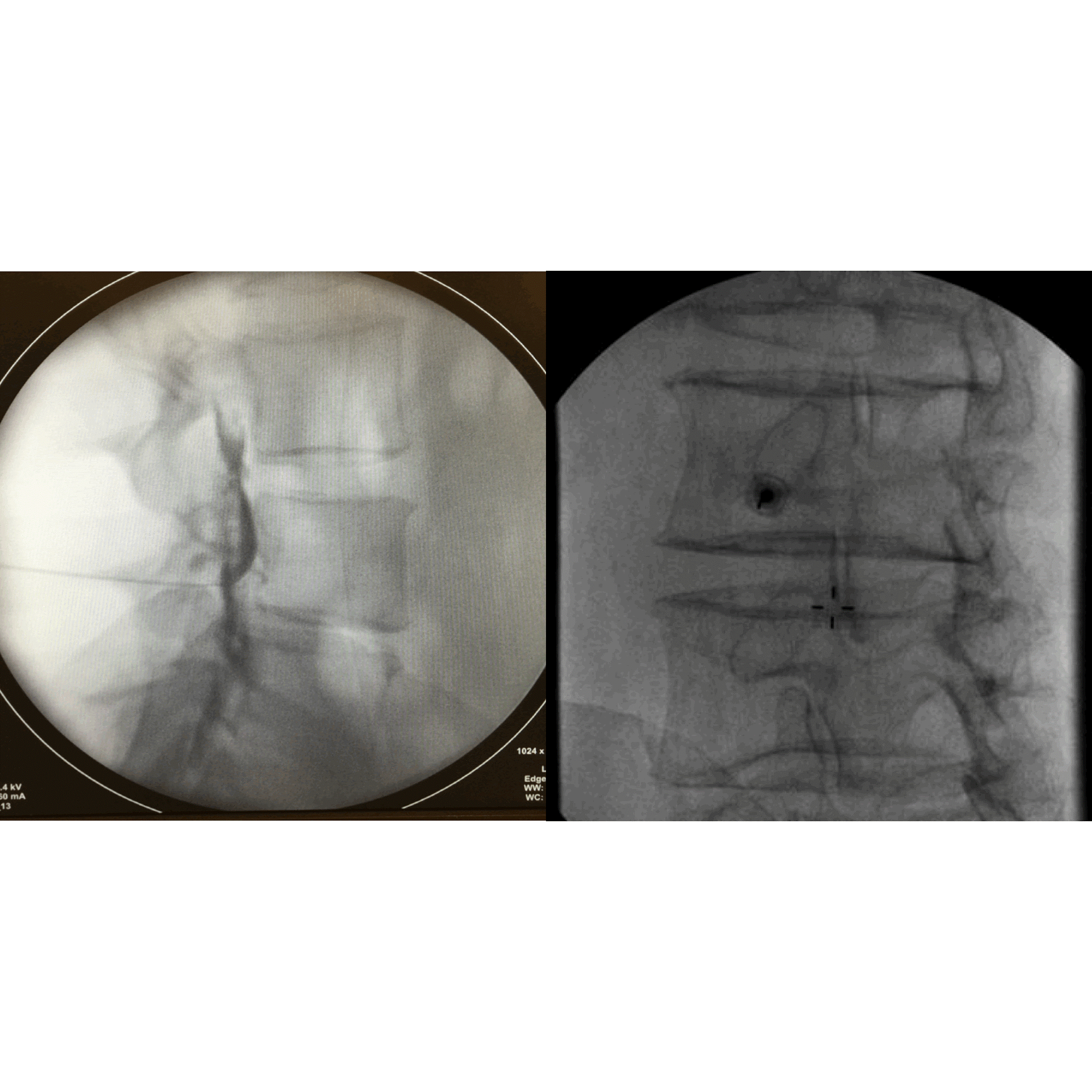
For the interlaminar route, patients were positioned prone on the procedure table with a pillow under the abdomen. The spinous processes of the lumbar vertebrae were palpated, and the specific interlaminar space for the injection was identified. After the area was cleaned and draped, 2% lignocaine (1 mL) was injected locally for anesthesia. Using an 18G or 20G spinal needle, the needle was inserted into the midline of the selected interlaminar space at a slight upward angle. The needle was advanced through the skin, subcutaneous tissue, supraspinous ligament, interspinous ligament, and ligamentum flavum until a loss of resistance was felt, indicating entry into the epidural space. Fluoroscopic guidance in AP and lateral views confirmed correct needle placement. A test dose of contrast dye was injected to ensure epidural placement and rule out intravascular or subarachnoid injection. The injection contained 4 mL of 2% xylocaine and 2 mL (80 mg) of methylprednisolone acetate (Fig. 3).
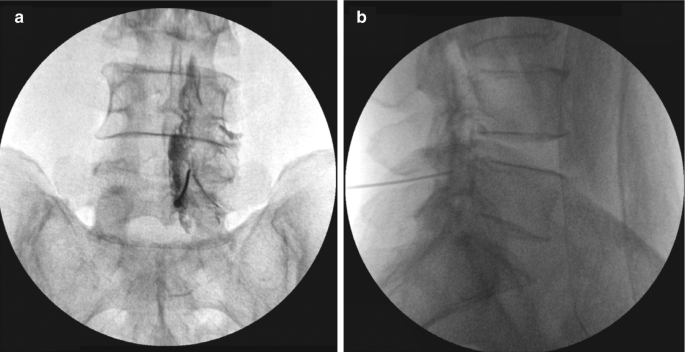
Figure 3: Needle positioning of interlaminar injection in anteroposterior view and lateral view.
Post-procedure assessment and monitoring
Following each procedure, patients were monitored in the day care ward for at least 4–6 h post-procedure. Vital signs were checked regularly, and patients were observed for any immediate complications, such as nausea, dizziness, vasovagal reactions, and headache. Post-procedure follow-up was scheduled at 1, 2, and 4 weeks, as well as 3 months, to assess the efficacy of the intervention using validated tools, such as the ODI, and VAS.
Statistical analysis
Data were compiled in Microsoft Excel and analyzed using SPSS v23.
- Analysis of variance (ANOVA) was used to compare group means
- Tukey’s HSD post hoc test identified intergroup significance
- P < 0.05 was considered statistically significant.
This prospective randomized study included 75 patients diagnosed with single-level lumbar disc herniation who did not respond to conservative treatment for at least 6 weeks. The patients were randomized into three groups of 25 individuals each, receiving a single 80 mg dose of methylprednisolone acetate through one of the three common epidural routes – caudal, transforaminal, or interlaminar. The groups were compared with respect to pain relief and functional recovery, as assessed by the VAS and ODI at baseline and during follow-up at 1 week, 2 weeks, 4 weeks, and 3 months. The demographic distribution across the three groups was comparable. Of the 75 patients, 42 were females (56%) and 33 were males (44%). Gender distribution was relatively balanced across groups, with 15 females and 10 males in the caudal group, 16 females and 9 males in the transforaminal group, and 11 females and 14 males in the interlaminar group. Chi-square analysis showed no statistically significant difference in gender distribution among the groups (P = 0.321). Similarly, age distribution was statistically equivalent. The overall mean age was 49.3 ± 14.4 years, with age ranges spanning from 25 to 75 years. The mean ages of the caudal, transforaminal, and interlaminar groups were 47.7, 47.1, and 53.1 years, respectively. ANOVA yielded no statistically significant difference in age between the groups (P = 0.312), thus confirming demographic comparability (Fig. 4).
Figure 4: Demographic summary.
<H2>Visual analog scale (VAS) scores
The mean pre-injection visual analog scale (VAS) scores for all three injection routes indicate severe pain levels: Caudal (8.04 ± 1.136), Transforaminal (8.52 ± 1.194), and Interlaminar (8.4 ± 1.155). These values suggest that all patients had significant baseline pain before intervention.
Table 1 presents the visual analog scale (VAS) pain scores at different time points for three injection techniques: Caudal, Transforaminal, and Interlaminar (Table 1 and Fig. 5).
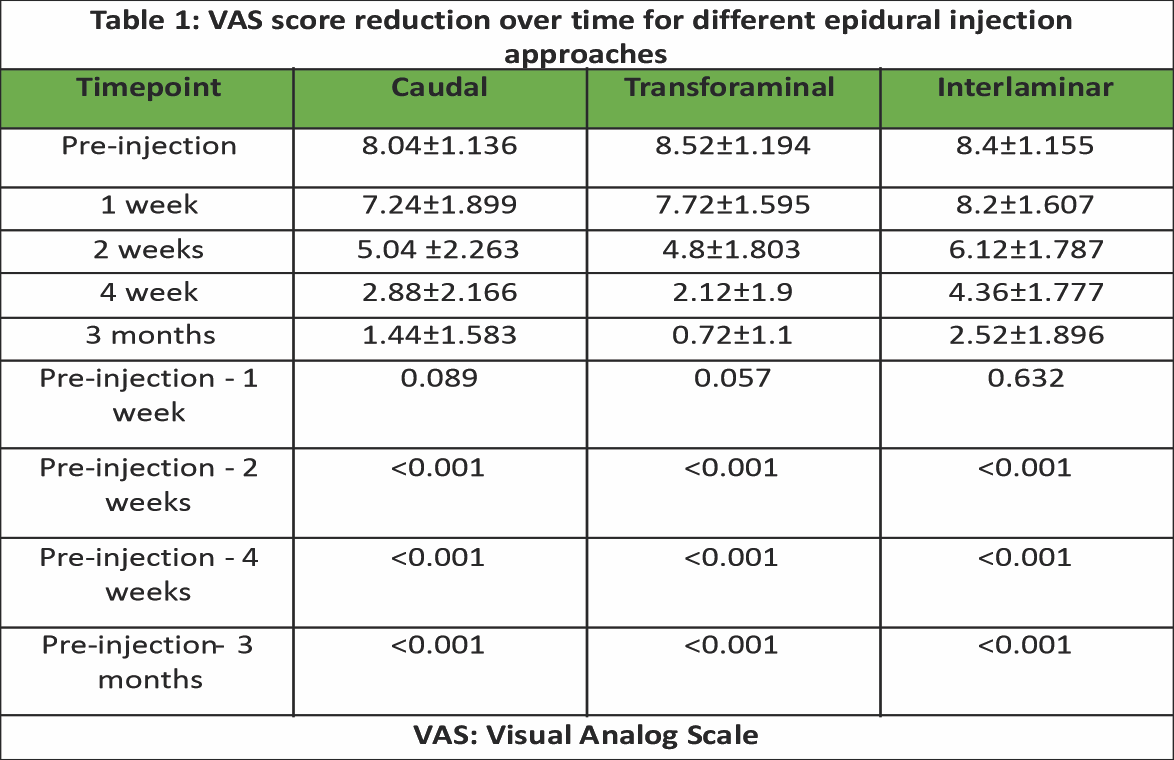
- Pre-injection VAS scores were 8.04 ± 1.136 , 8.52 ± 1.194, and 8.4 ± 1.155
- In 1 week, the scores were 7.24 ± 1.899, 7.72 ± 1.595, and 8.2 ± 1.607
- For 2 weeks, the scores were 5.04 ± 2.263, 4.8 ± 1.803, and 6.12 ± 1.787
- In 4 weeks, the VAS scores were 2.88 ± 2.166, 2.12 ± 1.9, and 4.36 ± 1.777
- For 3 months, the scores were 1.44 ± 1.583, 0.72 ± 1.1, and 2.52 ± 1.896.
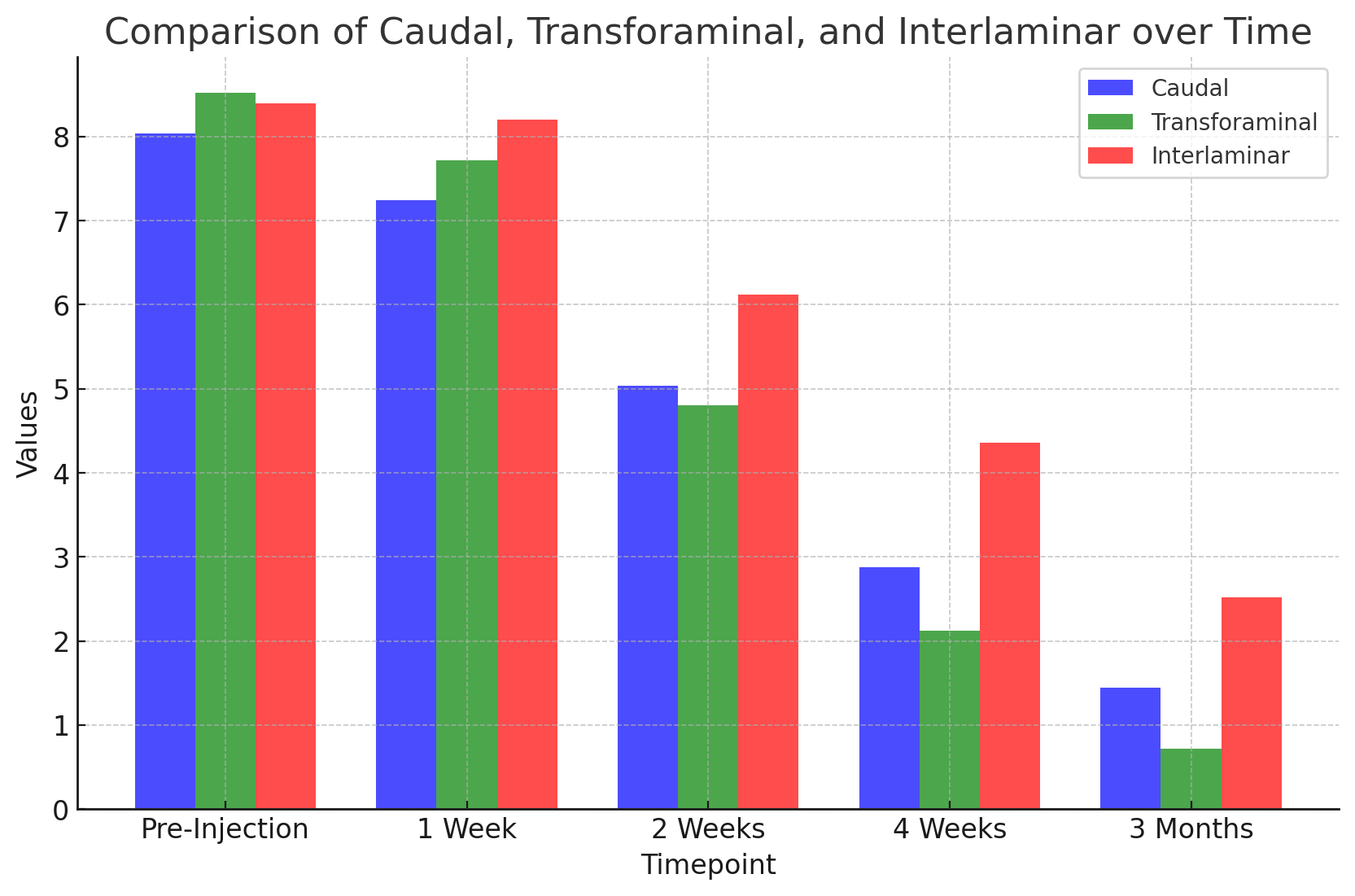
Figure 5: Graphic representation of Visual Analog Scale score over time.
ODI scores
The mean ODI scores before injection were comparable across all three groups, with Caudal (42 ± 5.276), Transforaminal (42.64 ± 5.114), and Interlaminar (41.96 ± 4.886), indicating a similar baseline level of disability due to pain.
Table 2 presents the scores at different time points for three injection techniques: Caudal, Transforaminal, and Interlaminar (Table 2 and Fig. 6).

- The pre-injection scores were 42 ± 5.276, 42.64 ± 5.114, and 41.96 ± 4.886
- At 1 week, the scores were 38.36 ± 9.278, 33.4 ± 8.822, and 38.32 ± 9.873
- At 2 weeks, the scores were 30.4 ± 9.937, 21.12 ± 9.563, and 30.64 ± 10.02
- At 4 weeks, the values were 23.04 ± 9.347, 9.4 ± 8.884, and 23.24 ± 10.101
- At 3 months, the scores were 15.56 ± 9.496, 2.92 ± 4.609, and 15.88 ± 10.199.
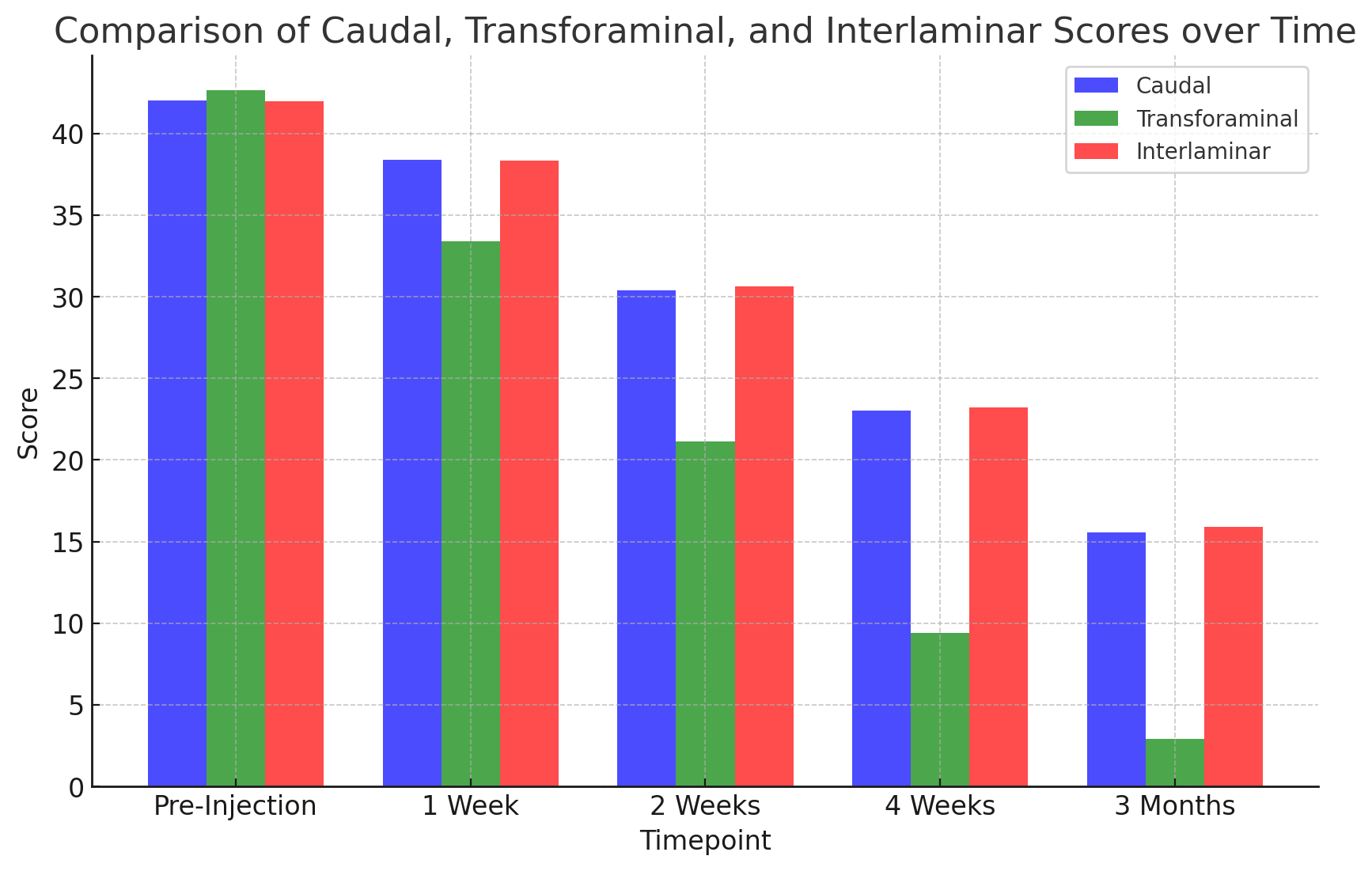
Figure 6: Graphic representation of Oswestry Disability Index score over time.
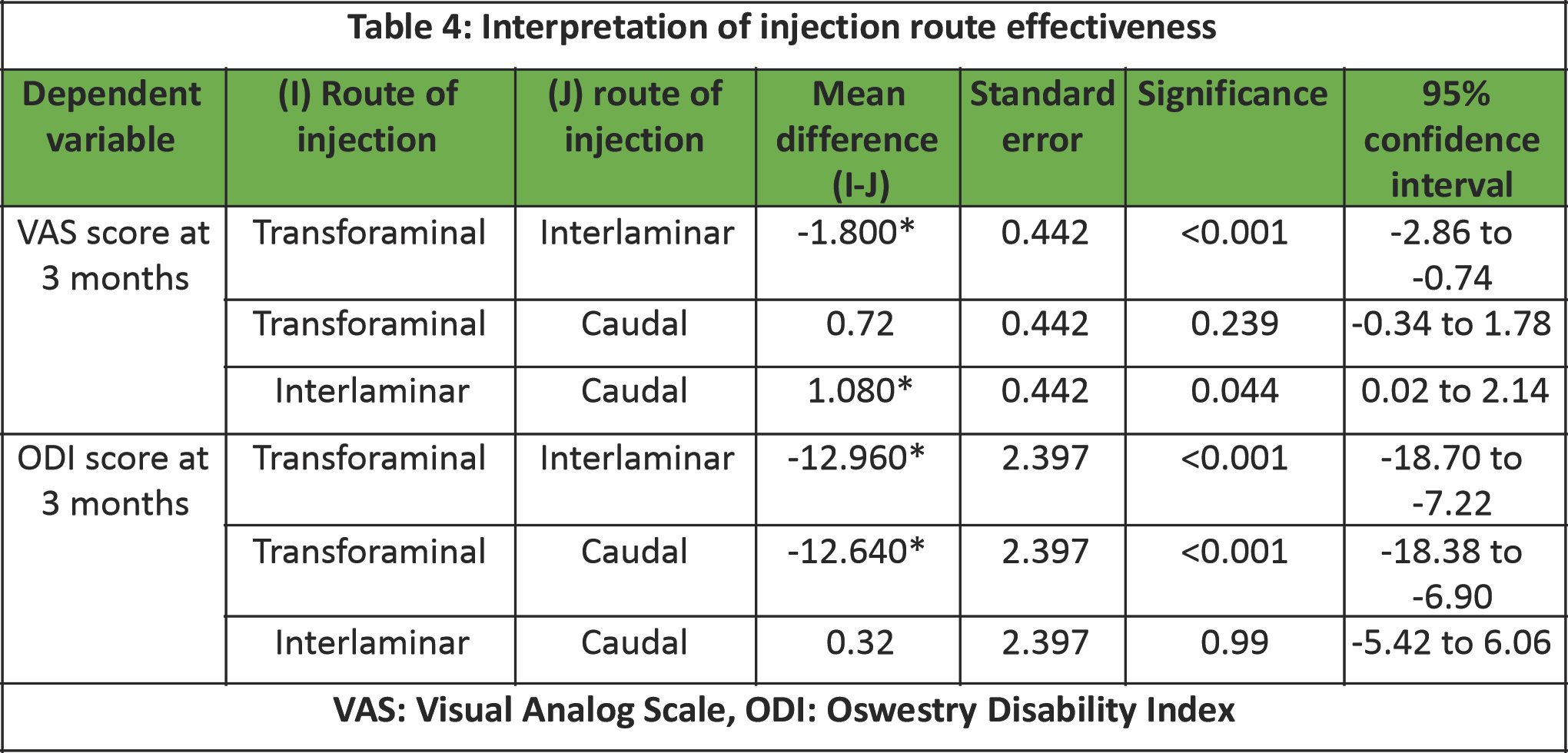
At the 3-month follow-up, pain relief peaked across all groups. Mean VAS scores were 1.44 ± 1.58 for the caudal group, 0.72 ± 1.10 for the transforaminal group, and 2.52 ± 1.89 for the interlaminar group. ANOVA analysis yielded an F value of 8.42 with P < 0.001, confirming a statistically significant difference among groups. Post hoc Tukey’s test showed that the transforaminal route was significantly more effective than the interlaminar route (P < 0.001). The difference between transforaminal and caudal routes, though numerically favoring the transforaminal route, was not statistically significant (P = 0.239). However, the interlaminar group had significantly worse outcomes than the caudal group (P = 0.044). Final ODI scores at 3 months reflected consistent patterns of improvement. The caudal group achieved a mean ODI of 15.56 ± 9.50, while the transforaminal group demonstrated near-complete functional recovery with an ODI of 2.92 ± 4.61. The interlaminar group remained behind, with a final mean ODI of 15.88 ± 10.19. ANOVA analysis showed significant differences (F = 19.02, P < 0.001). Post hoc comparisons revealed that the transforaminal group differed significantly from both the caudal (P < 0.001) and interlaminar groups (P < 0.001), while the difference between caudal and interlaminar routes was not statistically significant (P = 0.990) (Tables 3 and 4).

The present study investigated the comparative efficacy of epidural methylprednisolone injection through three commonly used routes – caudal, transforaminal, and interlaminar – in patients with lumbar PIVD. Our findings demonstrate that the transforaminal route yields superior pain relief and functional improvement, as measured by VAS and ODI scores at 3 months post-injection. While all three techniques were effective in reducing symptoms, the transforaminal group consistently outperformed the others, showing statistically significant improvements. These outcomes align with a growing body of literature supporting the transforaminal approach for its targeted drug delivery and clinical efficacy [12,15,16].
Lumbar disc herniation frequently compresses adjacent nerve roots, leading to an inflammatory cascade that sensitizes nerve fibers and results in radiculopathy. Methylprednisolone, as a potent glucocorticoid, reduces inflammation by suppressing pro-inflammatory cytokines and immune cell activity [6,7]. The choice of injection route influences both drug concentration at the site of inflammation and risk of complications.
The transforaminal route delivers corticosteroids directly to the anterior epidural space near the affected nerve root. This route enables maximum drug concentration at the site of pathology with minimal systemic exposure [9,12,13]. In our study, patients receiving transforaminal injections showed the most rapid and sustained pain reduction. The VAS score dropped from 8.52 ± 1.19 pre-injection to 0.72 ± 1.1 at 3 months. Similarly, ODI improved markedly to 2.92 ± 4.61.
These results are in agreement with those of Vad et al. [15], who demonstrated that transforaminal injections provide better outcomes compared to caudal and interlaminar routes. Karppinen et al. [16] also reported improved function and reduced surgical requirement following transforaminal ESI. Furthermore, Riew et al. [13] found that transforaminal ESI reduced the need for surgical intervention by up to 40% in patients with radiculopathy.
The advantages of this route, however, come with procedural challenges. Precise needle placement is critical, as intravascular injection, nerve root injury, or inadvertent dural puncture are potential complications [17]. In our study, no major complications were observed, likely due to the use of fluoroscopic guidance and adherence to strict procedural protocols.
Caudal ESI involves injection through the sacral hiatus, resulting in more diffuse drug distribution. While this route is considered the safest, particularly in patients with altered anatomy or prior spinal surgeries, it is less efficient in achieving high local drug concentrations at the affected nerve root [10,11]. In our study, the caudal group showed significant improvement in VAS and ODI scores, but to a lesser degree than the transforaminal group (VAS: 1.44 ± 1.58; ODI: 15.56 ± 9.49 at 3 months).
These findings are consistent with the literature. Buenaventura et al. [9] reported pooled success rates of 64% for caudal injections compared to 78% for transforaminal. Cousins et al. [18] emphasized its ease of administration and low complication rate, but acknowledged that caudal ESI may require repeated injections for optimal results.
The interlaminar route permits access to the posterior epidural space at or near the level of the herniated disc. It provides a balance between safety and targeted delivery [14]. In our study, the interlaminar group had better outcomes than caudal but was significantly less effective than transforaminal ESI in both VAS and ODI scores at 3 months (VAS: 2.52 ± 1.89; ODI: 15.88 ± 10.19).
This trend mirrors the findings of Manchikanti et al. [17] and Kennedy and Plastaras [19], who reported moderate efficacy of interlaminar ESI, particularly in non-foraminal pathology. Nelson and King [14] suggested that interlaminar ESI is less effective in cases of far lateral or foraminal disc herniation due to limited anterior epidural spread.
Analyzing pain relief over time, our study noted that significant improvement occurred after the 2nd week across all groups, with maximum benefit achieved by 3 months. This is supported by Helm et al. [20], who reported sustained pain relief with transforaminal ESI up to 1 year in discogenic pain. Early pain relief (within 1 week) was modest across groups, possibly due to the time required for corticosteroids to suppress local inflammatory mediators.
In this study, the transforaminal group received 40 mg methylprednisolone versus 80 mg in the other groups. This dose reduction is justified due to the precision of drug placement in transforaminal ESI. Studies by Botwin et al. [21] and Lee et al. [22] support the effectiveness of lower steroid doses when delivered with anatomical accuracy. This minimizes systemic exposure and reduces adverse effects.
In India, surgical treatment for lumbar disc herniation is often inaccessible to a large proportion of the population. Thus, safe and effective interventional pain management techniques are crucial. Indian studies, such as Rajkumari et al. [23], Pandey et al. [24], and Patel et al. [25], have confirmed the efficacy of ESI in local populations. In our study, the results echo global trends and reinforce the role of transforaminal ESI in routine practice.
Our study has several strengths, including a robust design with well-defined methodology, standardized assessment tools for evaluating pain relief and functional improvement, and a diverse patient population, enhancing the generalizability of our findings. It also provides valuable comparative data on different epidural injection techniques, supporting evidence-based clinical decision-making. However, the relatively small sample size may limit the broader applicability of the results, and the short, 3-month follow-up restricts assessment of long-term outcomes and recurrence rates. In addition, factors, such as quality of life, psychological impact, and long-term recurrence were not evaluated, highlighting areas for further research to provide a more comprehensive understanding of the overall effectiveness of epidural injection techniques.
The present study evaluated 75 patients with lumbar disc herniation treated with ESIs through three different approaches: Caudal, interlaminar, and transforaminal. Patients were evenly divided among the three groups, each receiving a standard combination of methylprednisolone and 2% lignocaine. While 80 mg of methylprednisolone was administered for caudal and interlaminar routes, a reduced 40 mg dose was used in the transforaminal group due to its highly targeted drug delivery, minimizing systemic side effects. At the 3-month follow-up, the transforaminal approach demonstrated the most significant improvement in pain (VAS reduction from 7.8 to 2.63, 66.3%) and disability (ODI reduction from 42.64 to 16.4, 61.5%) compared to caudal (VAS 51.9%, ODI 48.4%) and interlaminar (VAS 46.3%, ODI 43.7%) routes. This superior outcome is likely due to precise corticosteroid deposition at the inflamed nerve root, enhancing therapeutic efficacy and reducing complications. Importantly, no major adverse effects were reported in any group throughout the follow-up period. The transforaminal route, with its focused drug delivery, minimized the risk of complications typically associated with more diffuse epidural techniques, reinforcing it as a safe and effective non-surgical treatment option for patients with lumbar disc herniation.
Epidural steroid injections (ESIs) are an effective treatment for lumbar prolapsed intervertebral disc (PIVD) with significant pain and disability reduction. Among the three common routes—caudal, transforaminal, and interlaminar—the transforaminal route provides superior pain relief and functional recovery. This technique is the most targeted, delivering corticosteroids directly to the affected nerve root, making it the most effective in achieving rapid and sustained symptom improvement. It is critical, however, to select the injection route based on the patient’s anatomy and specific clinical conditions, as well as to use fluoroscopy for precise needle placement to minimize risks.
References
- 1. GBD 2021 Disease and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2022;400:2237-77. [Google Scholar] [PubMed]
- 2. Leveille SG, Buchanan JL, Cooney LM Jr., Wallace RB. Self-reported functional difficulty in old age: A comparison of probing techniques. J Am Geriatr Soc 1999;47:1042-9. [Google Scholar] [PubMed]
- 3. Daniell JR, Osti OL. Failed back surgery syndrome: A review article. Asian Spine J 2018;12:372-9. [Google Scholar] [PubMed]
- 4. Yang S, Liu Y, Li H, Wang J, Peng Y, Zhao W. Efficacy of transforaminal, interlaminar, and caudal epidural injections in managing lumbar disc herniation: A systematic review and network meta-analysis. Spine J 2010;10:207-14. [Google Scholar] [PubMed]
- 5. Stout A. Epidural steroid injections for low back pain. Phys Med Rehabil Clin N Am 2010;21:825-34. [Google Scholar] [PubMed]
- 6. Liu J, Zhou H, Lu L, Li X, Jia J, Shi Z, et al. The effectiveness of transforaminal versus caudal routes for epidural steroid injections in managing lumbosacral radicular pain: A systematic review and meta-analysis. Medicine (Baltimore) 2016;95:e3373. [Google Scholar] [PubMed]
- 7. Yun Z, Wang C, Yu T, Yuan T, Nie X, He T, et al. Comparative effects of different epidural injection approaches on lumbosacral radicular pain: A systematic review and network meta-analysis. Pain Physician 2020;25:531-42. [Google Scholar] [PubMed]
- 8. Goel A, Singh S, Shukla NK, Yadav A. Efficacy of caudal epidural steroid injections in chronic low backache patients. J Pharm Bioallied Sci 2023;15(Suppl 1):S669-72. [Google Scholar] [PubMed]
- 9. Buenaventura RM, Datta S, Abdi S, Smith HS. Systematic review of therapeutic lumbar transforaminal epidural steroid injections. Pain Physician 2009;12:233-51. [Google Scholar] [PubMed]
- 10. Lee JH, Shin KH, Bahk SJ, Lee GJ, Kim DH, Lee CH, et al. Comparison of clinical efficacy of transforaminal and caudal epidural steroid injection in lumbar and lumbosacral disc herniation: A systematic review and meta-analysis. Spine J 2018;18:2343-53. [Google Scholar] [PubMed]
- 11. Rekatsina M, Peng PW. The importance of image guidance in common spine interventional procedures for pain management: A comprehensive narrative review. Pain Ther 2025;14:841-63. [Google Scholar] [PubMed]
- 12. Lutz GE, Vad VB, Wisneski RJ. Fluoroscopic transforaminal lumbar epidural steroids: An outcome study. Spine 1998;23:442-8. [Google Scholar] [PubMed]
- 13. Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C. The effect of nerve-root steroid injection on the need for operative treatment of lumbar radicular pain: A prospective, randomized, controlled, double-blind study. Spine 2000;25:737-43. [Google Scholar] [PubMed]
- 14. Kroenke K. Pain measurement in research and practice. J Gen Intern Med 2018;33(Suppl 1):7-8. [Google Scholar] [PubMed]
- 15. Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: A prospective randomized study. Spine (Phila Pa 1976) 2002;27:11-6. [Google Scholar] [PubMed]
- 16. Karppinen J, Ohinmaa A, Malmivaara A, Kurunlahti M, Kyllönen E, Pienimäki T, et al. Periradicular infiltration for sciatica: A randomized controlled trial. Spine (Phila Pa 1976) 2001;26:1059-67. [Google Scholar] [PubMed]
- 17. Manchikanti L, Singh V, Cash KA, Pampati V, Falco FJ. A comparative effectiveness evaluation of epidural injections with or without steroids for lumbar disc herniation: A systematic review and meta-analysis. Pain Physician 2012;15:E199-244. [Google Scholar] [PubMed]
- 18. Cousins MJ, Bridenbaugh PO, Carr DB. Neural blockade in clinical anesthesia and management of pain. Anesth Analg 1992;74:412-6. [Google Scholar] [PubMed]
- 19. Kennedy DJ, Plastaras CT. A systematic review of the effectiveness of lumbar interlaminar epidural injections. Pain Physician 2015;18:E191-223. [Google Scholar] [PubMed]
- 20. Helm S, Harmon D, Noe C, Deer T, Falco FJ, Manchikanti L. A systematic review of the effectiveness of lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain. Pain Physician 2021;24:S13-44. [Google Scholar] [PubMed]
- 21. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Sanelli JT, Freeman ED, et al. Fluoroscopically guided lumbar transformational epidural steroid injections in degenerative lumbar stenosis: An outcome study. Am J Phys Med Rehabil 2002;81:898-905. [Google Scholar] [PubMed]
- 22. Lee JW, Kim SH, Choi JY, Yeom JS, Kim KJ, Chung SK, et al. Transforaminal epidural steroid injection versus interlaminar epidural steroid injection for the treatment of radicular pain: A randomized, blinded, prospective study. Pain Physician 2018;21:547-56. [Google Scholar] [PubMed]
- 23. Rajkumari N, Devi BI, Ramesh VG. Transforaminal versus interlaminar epidural steroid injection in the management of lumbar disc herniation: A randomized controlled trial. J Spine Surg 2021;7:157-63. [Google Scholar] [PubMed]
- 24. Pandey RK, Sethi A, Aggarwal S, Jindal R. Comparison of caudal versus transforaminal epidural steroid injections in managing lumbar disc herniation. J Clin Diagn Res 2016;10:RC01-3. [Google Scholar] [PubMed]
- 25. Patel AK, Kulkarni D, Dave B, Parikh T. Role of interlaminar epidural steroid injection in management of lumbar radiculopathy: An Indian experience. Indian J Orthop 2023;57:32-8. [Google Scholar] [PubMed]