Combined fixation with a pre-contoured distal clavicle plate and tunneled EndoButton provides reliable union, restores coracoclavicular stability, and yields excellent functional outcomes with minimal complications in unstable lateral end clavicle fractures.
Dr. Sahil Maingi, Department of ENT, Dayanand Medical College and Hospital, Civil Lines, Tagore Nagar, Ludhiana, Punjab, India. E-mail: ssmaingi@gmail.com
Introduction: Unstable lateral end clavicle fractures (Neer type 2) are prone to non-union due to various deforming forces and present a challenge in management. While multiple fixation techniques exist, each has its own complications. Combining a pre-contoured locking distal clavicle plate with a tunneled suspensory device gives best clinical and biomechanical results.
Materials and Methods: This prospective interventional study included 50 patients with unilateral Neer type 2 fractures of clavicle, treated with combined fixation using a pre-contoured locking distal clavicle plate and tunneled EndoButton. Patients were followed up for 6 months postoperatively. Functional outcomes were assessed using Constant-Murley and modified University of Calofornia Los Angeles (UCLA) scores, and radiological outcomes included coracoclavicular distance measurements and fracture union rates.
Results: The mean Constant-Murley score improved from 79.2 at 6 weeks to 94.1 at 6 months, comparable to uninjured shoulder (P = 0.894). Similarly, the modified UCLA score improved from 28.9 to 33.8 over the same period (P = 0.256). All patients achieved radiological union. Coracoclavicular distance significantly reduced postoperatively and remained comparable to contralateral side at final follow-up (P = 0.107). Complications were minimal, with no cases of nonunion, hardware failure or EndoButton migration.
Conclusion: Combined fixation using a pre-contoured locking distal clavicle plate and tunneled suspensory EndoButton device offers excellent radiological union and functional outcomes with minimal complications making it a reliable option for treating unstable lateral end clavicle fractures.
Keywords: Clavicle fracture, distal clavicle plate, EndoButton, Neer type 2.
The clavicle known as the collar bone is the articulating link between the upper limb and the axial skeleton. Clavicular fractures are relatively common traumatic injuries around the shoulder girdle due to the subcutaneous position of clavicle and constitute about 2–4% of all adult fractures [1,2], whereas lateral end clavicle fractures account for 12–15% of all clavicle fractures [3]. The lateral end clavicle fracture account for about fifty percent of all clavicular non-union [4]. Neer divided the lateral end clavicle fractures into three types [5,6,7]. Type I with intact coracoclavicular ligaments, Type II with the coracoclavicular ligaments detached from the medial segment, and Type III lateral end clavicular fractures involve acromioclavicular (AC) joint alone. Type II fractures were subdivided into two subgroups Type IIA and Type IIB according to the disruption of coracoclavicular ligament. The functional results of minimally displaced Type I and III fractures when managed conservatively, are generally satisfactorily. On the other hand, non-union rates are as high as 30% in Type II fractures due to the deforming forces occurring at the fracture site. The weight of the upper extremity, pull of muscles such as pectoralis major, and scapular rotators lead to downward displacement of the lateral fragment. On the other hand, the trapezius muscle pulls the medial fragment upwards. These strong and multidirectional forces occurring at the fracture site may explain the high rate of nonunion of unstable lateral end clavicle fracture. The treatment of this Type 2 fracture thus is very challenging. The non-union may lead to persistent pain, loss of shoulder strength, and restriction of shoulder movements. Since it is difficult to manage such non-union cases, open reduction and internal fixation is often recommended as the primary treatment for such unstable fractures [8]. A lot of operative procedures for fixation of lateral third clavicle fractures have been described in literature such as Kirschner wiring, screw fixation, tension band wiring, plate fixation, and arthroscopic treatment for unstable lateral end clavicle fractures but unfortunately these operative procedures are associated with a lot of drawbacks [9,10,11,12,13]. With the continued evolution of internal fixation devices, locking T-plates have been used to increase the stability of the lateral clavicular fragment. Recently, there have been some cases treated with additional CC interval fixation using suture anchors or buttons to repair the CC ligaments [14,15,16]. All of these operative procedures have been associated with high intraoperative and post-operative complications and none of them have been found to be gold standard treatment modality. These complications often require re-surgery in 43% patients [17]. Anatomical locking plate fixation has emerged as a popular surgical method for unstable distal clavicle fractures [18]. The advantage of the anatomical locking plate is that the AC joint and the subacromial space are not violated and the AC joint is totally spared [19]. However, the vertical stability of the fracture with plate fixation alone might not be sufficient due to small lateral fragments. The stability can be achieved if coracoclavicular fixation is combined with the fracture fixation [20]. This is due to the fact that pre-contoured lateral end locking plates with coracoclavicular reconstruction negates both horizontal and vertical deforming forces occurring at the fracture site efficiently, thereby providing better functional outcomes and less chances of failure [21]. Taking into account the lacunae of studies involving the Indian population undergoing the proposed procedure, the authors aimed to evaluate a surgical technique of managing Neer Type II B lateral clavicle fracture consisting of anatomical reconstruction of lateral clavicle leaving the uninjured AC joint untouched. The purpose of this study was to assess the functional and radiological outcome of unstable lateral end clavicle fracture treated by our surgical technique and method of fixation.
Study design
The authors conducted a prospective interventional study over a duration of 18 months with a sample size of 50.
Study sample
Patients meeting the inclusion criteria were subjected to clinical examination and radiological evaluation with plain radiography of bilateral shoulder before surgery after written informed consent.
Sample size
The study of Tae Kang Lim et al. observed that union rate was 95.65% in coracoclavicular ligament suture augmentation with anatomical locking plate fixation procedure [15]. Taking this value as reference, the minimum required sample size with 6% margin of error and 5% level of significance is 45 patients. To reduce margin of error, total sample size taken is 50.
Inclusion criteria
- Patients with clinical and radiological findings suggestive of unilateral Neer Type II fractures.
- Age < 60 years.
- Patients with normal pre-injury shoulder function.
Exclusion criteria
- Patients with previous injury to the fractured clavicle or ipsilateral shoulder.
- Polytrauma patients.
- Patients with neurovascular compromise.
- Patients having pathological fracture
- Patients having open fracture
- Patients having AC joint dislocation.
Ethical clearance
- Ethical clearance from the Institutional Ethical Committee was taken.
- IEC number-10/252 (Dated: October 30, 2019).
- Informed consent from all the patients was taken.
Procedure
Pre-operative assessment
Pre-operative evaluation of the normal shoulder was done using modified University of Calofornia Los Angeles (UCLA) shoulder rating score and the Constant and Murley score. Pre-operative neurovascular status was assessed and recorded for each patient. Radiological assessment of fracture clavicle was done using antero-posterior roentgenogram of bilateral shoulder. Pre-operative all blood investigations, electrocardiography, urine routine, and microscopic examination and chest X-ray were done as part of pre-anesthetic evaluation.
Surgical procedure
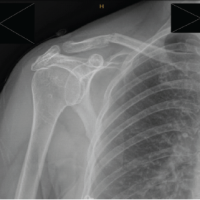
Under general anesthesia in beach chair position, a 5–7 cm vertical (“bra-strap”) incision was made from the tip of the coracoid process to anterosuperior aspect of the lateral third of the clavicle. Medial and lateral flaps were developed. The deltotrapezial fascia was then incised perpendicular to the skin incision and released from the clavicle. The fracture ends and coracoid was exposed. Dissection medial to the coracoid was avoided to prevent inadvertent damage to neurovascular structures. A tunnel was made at the coracoid base centrally about 1.5 cm from its tip using a 2.5 mm drill bit. Another bony tunnel was made in the clavicle just above the coracoid slightly anterior to the midline. Then, an EndoButton loaded with ethibond suture no. 5 was passed under the coracoid and the clavicle tunnel in a retrograde fashion so that the EndoButton flipped on the undersurface of the coracoid and two ends of the suture come out of the clavicle which were later tied to the distal clavicle plate. The fracture ends were then reduced and fixed with anatomically pre-contoured locking distal clavicle plate, as shown in Fig. 1.

Figure 1: Clavicular fracture fixation done with anatomically pre-contoured plate and ligamentous reconstruction done with tunneled suspensory device (EndoButton).

Figure 2: Immediate post-operative radiograph of the unstable lateral end clavicle fixed with our surgical technique.
Proper hemostasis was achieved and wound was closed in layers. No drain was applied. The arm was immobilized in an arm pouch. Immediate post-operative radiograph was done (Fig. 2).
Post-operative period
Postoperatively, intravenous antibiotics were given and the patients were discharged on the 3rd day. Gentle pendular exercises were started on the 3rd day and passive shoulder range of motion (ROM) exercises on the 7th day with restriction of shoulder abduction to 90 degrees. Assisted active motion was started at 2 weeks after suture removal. Patients were allowed both active and passive full range of movements after 4 weeks. Arm pouch was removed after 6 weeks. Clinical evaluation was performed at 6 weeks, 3 months, and 6 months using modified UCLA score and Constant-Murley score and compared with the pre-operative score of the normal shoulder. Radiographic assessment included coracoclavicular distance and fracture union
Fifty consecutive patients with unstable Neer Type II fractures of the lateral end of clavicle were treated surgically using a pre-contoured locking distal clavicle plate along with coracoclavicular reconstruction with one EndoButton.
The mean age of the patients was 33.2 (±7.3) years, ranged between 20 and 49 years. Out of 50 patients, 34 (68%) patients were male while 16 (32%) were female. While observing the distribution of site and cause of injury in study subjects, it was noted that the right side was involved in 32 (64%) cases as compared to the left side with 18 (36%) cases. The dominant side was affected in 76% of cases. The most common mechanism of injury was fall followed by road traffic accidents. The mean interval between injury and surgery was 5 days. The mean time of surgery was 75.6 min. The given Table 1 describes the modified UCLA score of injured side during pre-operative phase and follow-up intervals at 6 weeks, 3 months, and 6 months along with score of the normal side.
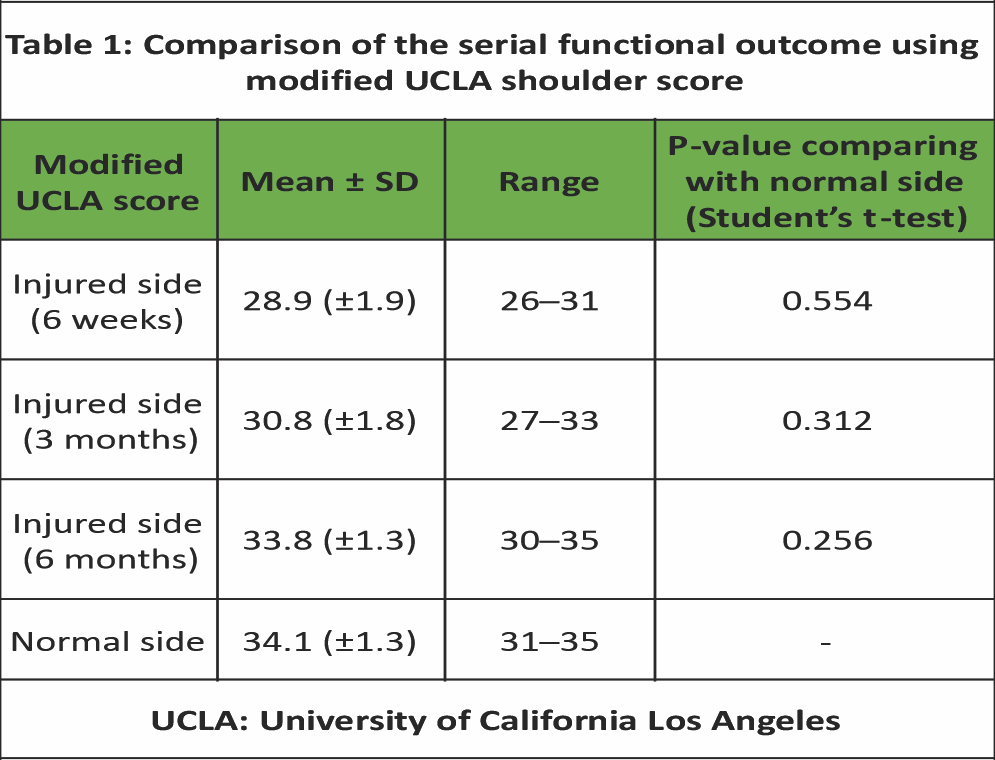 The modified UCLA score during pre-operative phase was 6.6 (±1.5) with range 4–12. After the surgical procedure, 6 weeks later, the score was 28.9 (±1.9) with range of 26–31. During the 3rd month follow-up, the score was 30.8 (±1.8) with range 27–33 and latest follow-up at 6th month was 33.8 (±1.3) with range 30–35. The score of normal side was 34.1 (±1.3) with range 31–35. When the mean scores of the normal side was compared to all the follow-up scores of the injured side, no statistical difference was observed. Similarly, when the mean score of the injured side pre-operation was compared to all the follow-up scores, a statistical difference was observed (P < 0.001). As seen in Fig. 3,
The modified UCLA score during pre-operative phase was 6.6 (±1.5) with range 4–12. After the surgical procedure, 6 weeks later, the score was 28.9 (±1.9) with range of 26–31. During the 3rd month follow-up, the score was 30.8 (±1.8) with range 27–33 and latest follow-up at 6th month was 33.8 (±1.3) with range 30–35. The score of normal side was 34.1 (±1.3) with range 31–35. When the mean scores of the normal side was compared to all the follow-up scores of the injured side, no statistical difference was observed. Similarly, when the mean score of the injured side pre-operation was compared to all the follow-up scores, a statistical difference was observed (P < 0.001). As seen in Fig. 3,
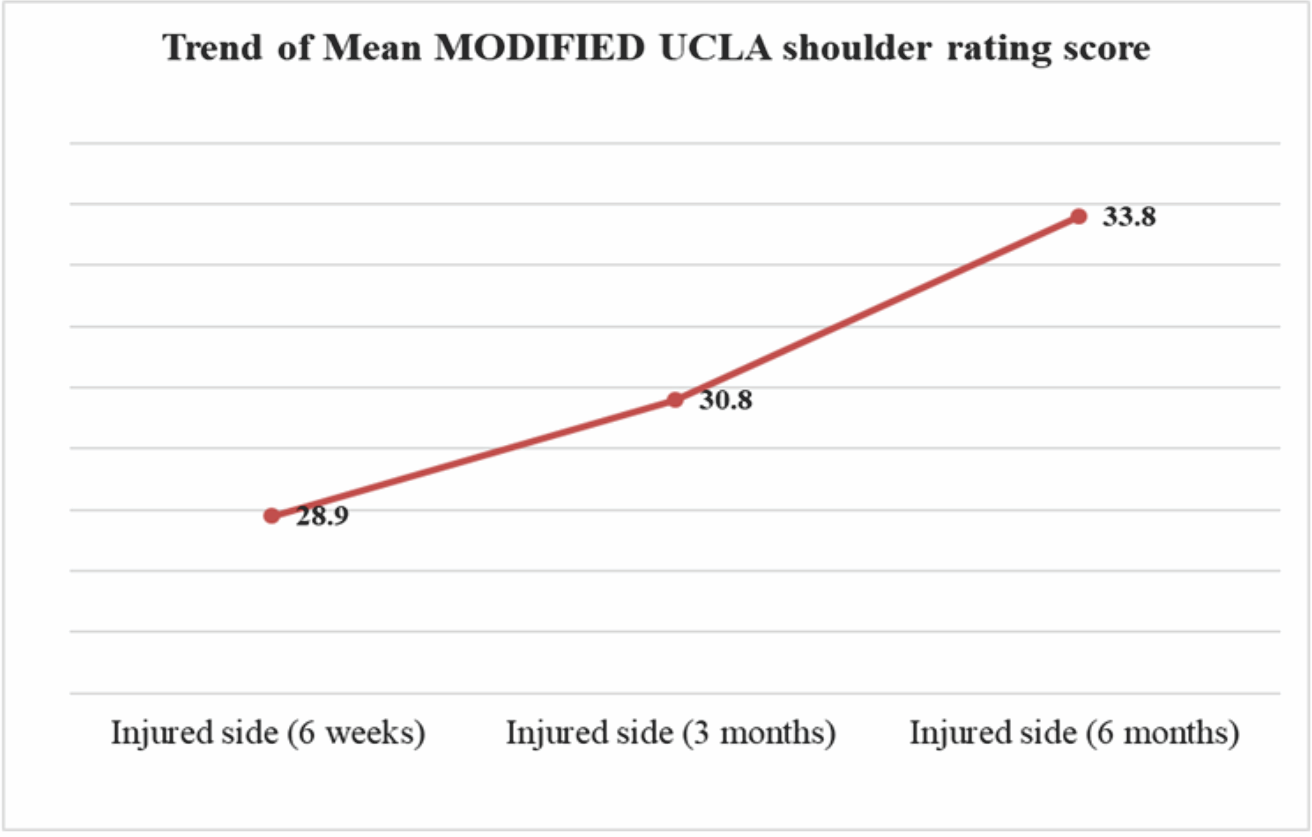
Figure 3: Trend of mean modified University of California Los Angeles shoulder rating score at injured side during post-operative period-6 weeks, 3 months, and 6 months.
the modified UCLA score displayed an upward trend on the injured side post-surgery. The given Table 2 describes the Constant-Murley score of injured side during follow-up intervals at 6 weeks, 3 months, and 6 months and along with the normal side.
 After the surgical procedure, 6 weeks later, the score observed was 79.2 (±3.4) with range of 73–88. During the 3rd month follow-up, the score was 87.2 (±2.9) with range 82–95 and latest follow-up at 6th month was 94.1 (±3.2) with range 86–98. The score of normal side was 97.1 (±1.8) with range 92–100. When the mean scores of the normal side was compared to all the follow-up scores of the injured side, no statistical difference was observed.
After the surgical procedure, 6 weeks later, the score observed was 79.2 (±3.4) with range of 73–88. During the 3rd month follow-up, the score was 87.2 (±2.9) with range 82–95 and latest follow-up at 6th month was 94.1 (±3.2) with range 86–98. The score of normal side was 97.1 (±1.8) with range 92–100. When the mean scores of the normal side was compared to all the follow-up scores of the injured side, no statistical difference was observed.
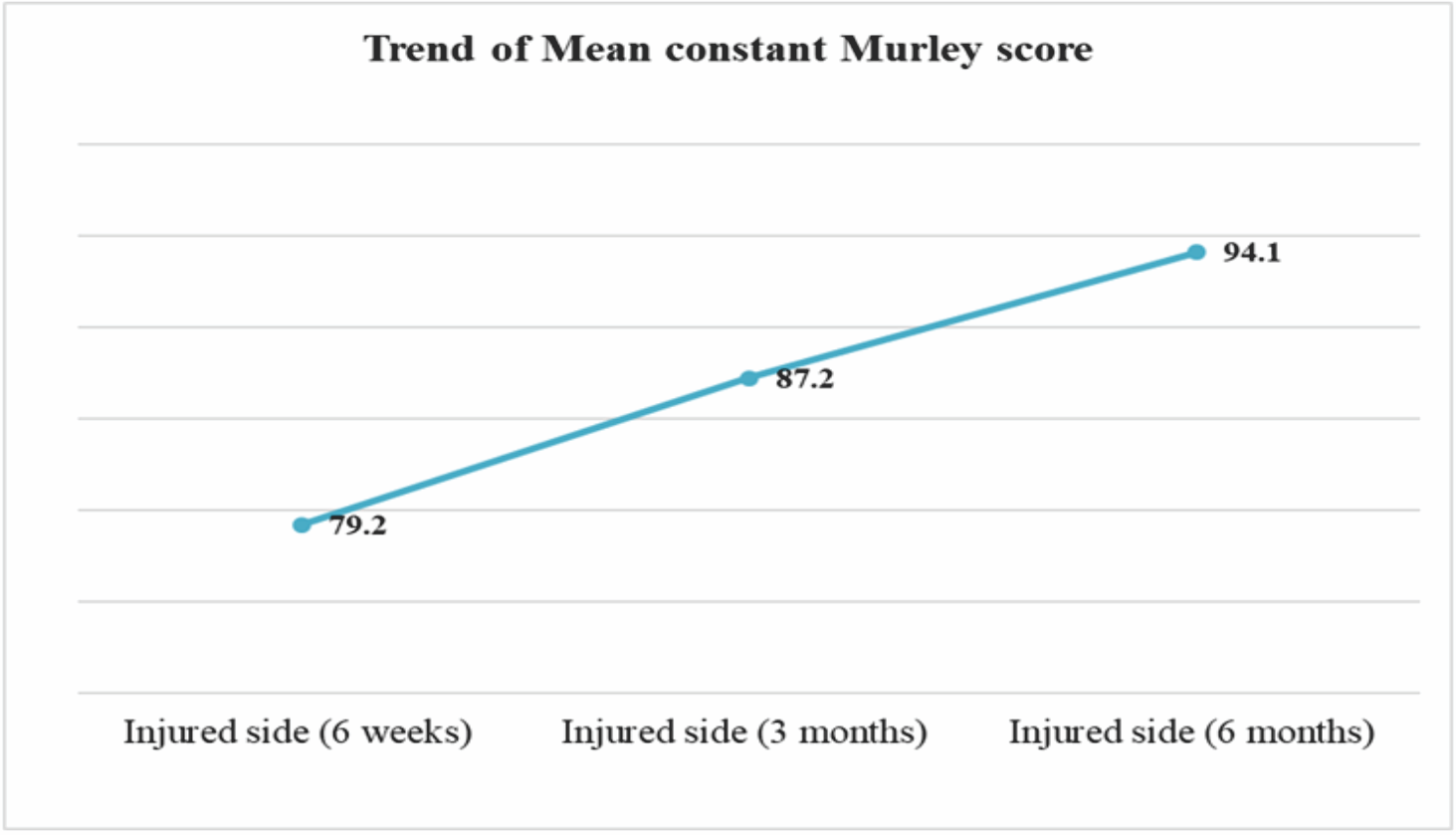
Figure 4: Trend of mean Constant-Murley score at injured side during post-operative period-6 weeks, 3 months, and 6 months.
Fig. 4 showcases the upward trend of the mean Constant-Murley score on the injured side.
In Table 3, it is described the coracoclavicular distance at injured side during pre-operative phase, post-operative phase, and follow-up intervals at 6 weeks, 3 months, and 6 months along with the distance at the normal side.
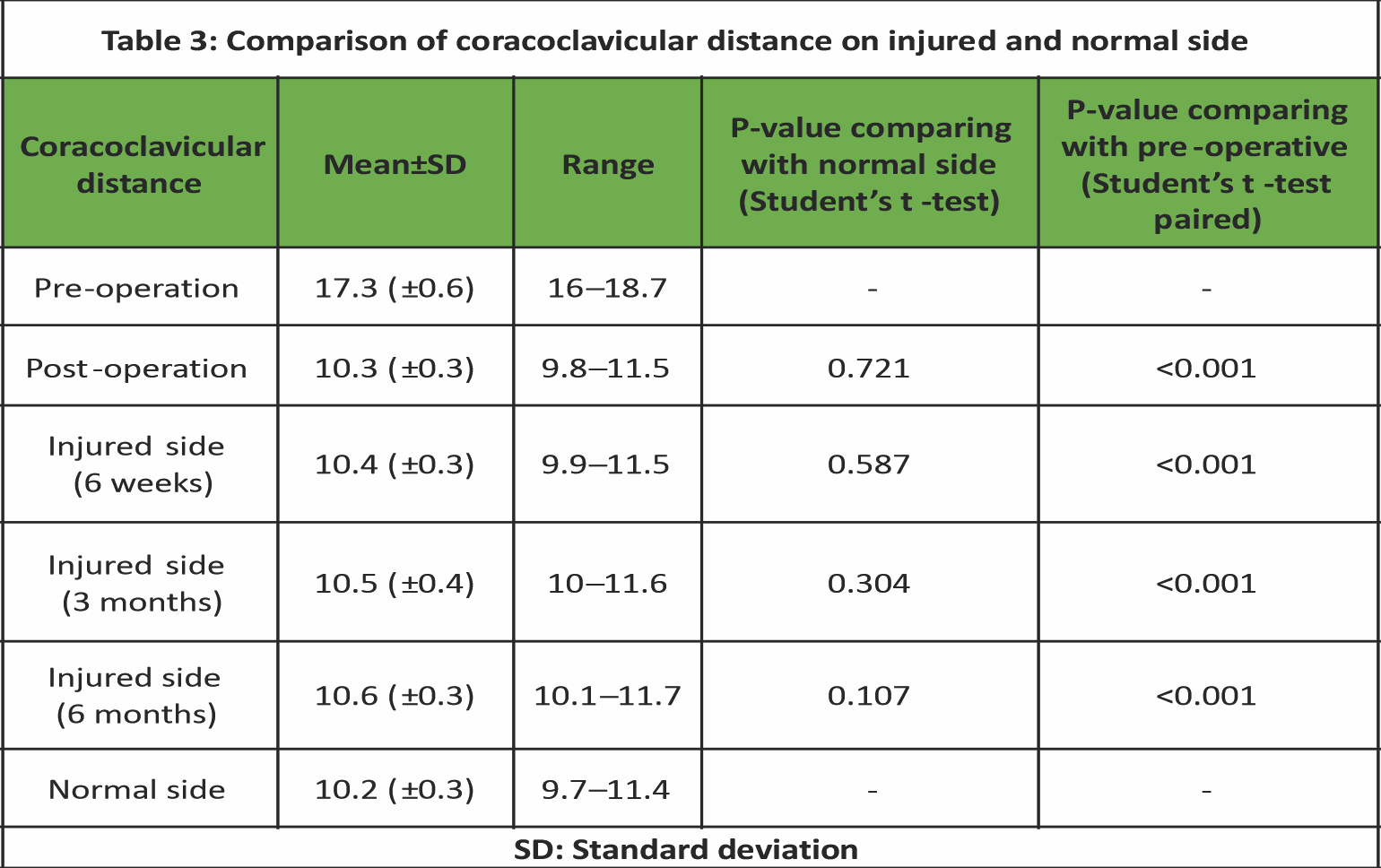 The mean coracoclavicular distance during pre-operative phase was 17.3 (±0.6) mm with range 16–18.7 mm. After the surgical procedure, the mean coracoclavicular distance during post-operative phase was 10.3 (±0.3) mm with range of 9.8–11.5 mm, 6 weeks later, the same mean distance was at 10.4 (±0.3) mm with range of 9.9–11.5 mm. During the 3rd month follow-up, the mean coracoclavicular distance was at 10.5 (±0.4) mm with range 10–11.6 mm and during the latest follow-up at 6th month, the same mean distance was at 10.6 (±0.3) mm with range 10.1–11.7 mm. The mean coracoclavicular distance of normal side was 10.2 (±0.3) mm with range 9.7–11.4 mm. When the mean distance of the injured side was compared to the normal side, no statistical difference was observed between the normal side and all follow-up scores including post-operation. Similarly, when mean distance of the injured side during pre-operation was compared to all the follow-up scores including post-operation, a statistical difference was observed (P < 0.001), with Fig. 5 showcasing the trend of the coracoclavicular distance on the injured side.
The mean coracoclavicular distance during pre-operative phase was 17.3 (±0.6) mm with range 16–18.7 mm. After the surgical procedure, the mean coracoclavicular distance during post-operative phase was 10.3 (±0.3) mm with range of 9.8–11.5 mm, 6 weeks later, the same mean distance was at 10.4 (±0.3) mm with range of 9.9–11.5 mm. During the 3rd month follow-up, the mean coracoclavicular distance was at 10.5 (±0.4) mm with range 10–11.6 mm and during the latest follow-up at 6th month, the same mean distance was at 10.6 (±0.3) mm with range 10.1–11.7 mm. The mean coracoclavicular distance of normal side was 10.2 (±0.3) mm with range 9.7–11.4 mm. When the mean distance of the injured side was compared to the normal side, no statistical difference was observed between the normal side and all follow-up scores including post-operation. Similarly, when mean distance of the injured side during pre-operation was compared to all the follow-up scores including post-operation, a statistical difference was observed (P < 0.001), with Fig. 5 showcasing the trend of the coracoclavicular distance on the injured side.
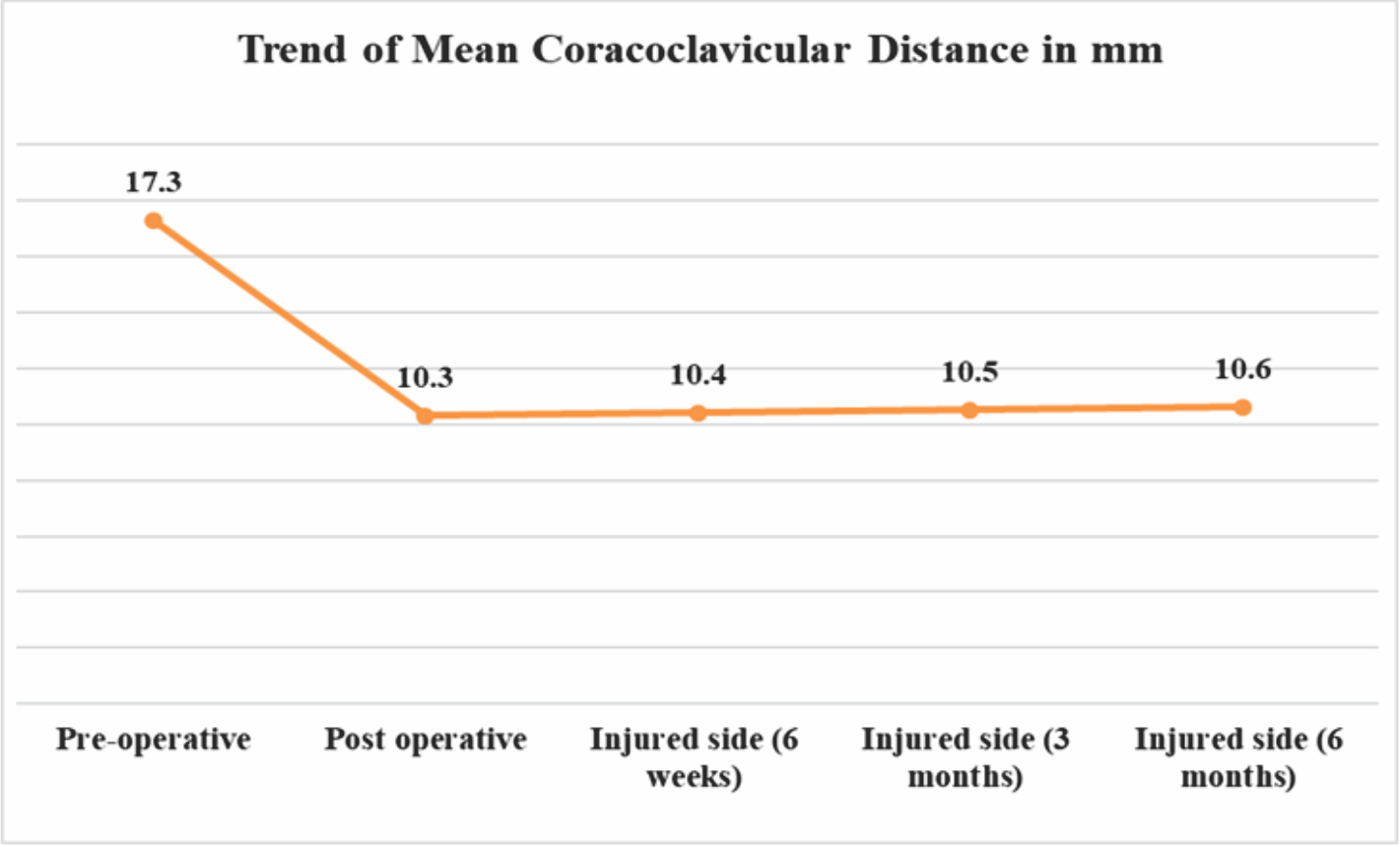
Figure 5: Trend of mean coracoclavicular distance in mm at injured side during post-operative period-6 weeks, 3 months, and 6 months.
The movement of the injured shoulder was measured using forward flexion, abduction, and internal rotation during 6th-month follow-up. As shown in Table 4, the mean forward flexion movement of the injured side was 174.9 (± 3.5) degrees with a range of 170–180 degrees. Similarly, the mean abduction movement of the injured shoulder was 173.3(±5.5) degrees with a range of 165–180 degrees. The mean internal rotation was 85.2 (±3.6) degrees with a range of 80–90 degrees. It was observed that all the patients returned to the pre-injury levels of motion.

No occurrence major complications were seen in any of the cases. Bony union was achieved in all cases. However, two of our patients (4 %) developed superficial infection which was managed with debridement and intravenous antibiotics. No patient complained of pain in their shoulder at 6-month follow-up. None of our the developed non-union, AC joint subluxation, plate pull out or EndoButton migration, and removal of implant due to hardware prominence was not required in any patient. Although 3 patients (6%) did complain of slight screw prominence, the discomfort was not to an extent that required implant removal. No patient showed signs of rotator cuff weakness, impingement, or glenohumeral instability.
Conservative management for lateral end clavicle fracture results in high numbers of non- union, .Therefore, operative management is now increasingly being accepted as the treatment modality of these unstable lateral end clavicle fractures. Many implants and surgical methods can be used for fixing such fractures such as Kirschner wires, Knowles pin, coracoclavicular screws, coracoclavicular slings, flexible coracoclavicular fixation, hook plate fixation, and locking plate fixation. However, all of these methods have disadvantages. Any internal fixation that consists of rigid fixation between the clavicle and coracoid or the clavicle and acromion will have to be removed before full mobilization is initiated. Transacromial Kirschner wires when used have been associated with high infection rate which may lead to sepsis, K-wire migration, and reduced stability requiring increased immobilization which leads to stiffness of the shoulder region postoperatively. Wire migration can sometimes disastrously cause tetraplegia. Even though the complications with the use of K wires are exceptionally rare, a treatment method using K wire as a means of fixation of clavicle fracture is not justifiable. Knowles pin can directly penetrate AC joint and cause arthrodesis or fibrosis and osteoarthritis of the AC joint. Patients when treated with coracoclavicular screws may need implant removal due to impingement and the complications such as screw back out, malunion of fracture are not uncommon. Coracoclavicular slings when used a treatment modality are commonly associated with fracture of the coracoid process. Closed-loop double EndoButton fixation when used as the treatment modality lead to non-union and frozen shoulder [22,23,24]. .Hook plates when used as the treatment modality for unstable distal clavicle fractures lead to shoulder stiffness, rotator cuff pathology, impingement of shoulder, bony erosion, and osteolysis of acromion. No incidence of axial pull out of screws was observed in the study as opposed to cases involving fracture fixation modality using plate alone without coracoclavicular reconstruction used by Brouwer et al. [25], leading to high incidence of fracture fixation failure. The study, also, did not observe any AC joint subluxation as opposed to the fracture fixation modality used by Sajid et al. [26] which led to high incidences of AC joint disruption. Suggesting, the proposed surgical technique holds potential to avoid such disastrous complications. In a study performed by Zhang et al. [27], the functional outcome as represented by Constant-Murley score of the anatomically pre-contoured clavicle locking plate is better than the clavicle hook plate. The results of the present study are in accordance with the study of Zhang et al. as the functional outcome of the fractured extremity was comparable to the unaffected side. Study performed by Xu et al. [28] revealed that the clinical outcomes of the distal clavicular locking plate and coracoclavicular suture anchor combination group were better than the locking plate alone group for treatment of unstable lateral end clavicle fracture, with far less complications in the combination group as compared to the plate alone group. Another study performed by Vikas et al. [29] using pre-contoured locking plate and coracoclavicular reconstruction with EndoButton and fiber wire showed promising results. Other studies like the ones performed by Largo et al. [30] using T-plate and a polydioxanone cord (PDS) on unstable lateral end clavicle fracture and study performed by Schleiman et al. using combination of locked plate fixation and minimal-invasive coracoclavicular ligament reconstruction with a flip button showed satisfactory trends of the Constant and Murley score among other clinical and radiological improvements. In another study performed by Morsy et al. [31], osteosynthesis of unstable distal clavicular fractures with and without coracoclavicular ligament reconstruction was compared. Fixation of the fracture was done with T-shaped locking plates and coracoclavicular reconstruction was done with suture anchors and the results revealed that the group which had undergone coracoclavicular reconstruction with suture anchors had better post-operative ROM in the group. In our present study for fixation of unstable lateral end clavicle fracture using anatomically pre-contoured lateral clavicle locking plate and tunneled suspensory device fixation, the mean Constant-Murley [32] score at the final follow-up was 94.1 range (86–98). The mean modified UCLA [33] score at the final follow-up was 33.8. The mean Constant-Murley score and the modified UCLA score of the injured shoulder at the 6 month follow-up were comparable to the normal shoulder and not statistically significant with P-value of 0.894 and 0.256, respectively. There was a continuous increase in the coracoclavicular distance at all follow-ups due to possible loosening of EndoButton fixation with time; however, it was not significant when compared to the normal side at the latest follow-up with P = 0.107. The mean post-operative coracoclavicular distance on the injured side was decreased by 38 % as compared to the pre-operative status. Bony union was achieved clinically and radiologically in all the cases and there were no major complications in any patient. Hence, these studies suggest coracoclavicular reconstruction using coracoclavicular screws, EndoButton fixation or suture anchors along with osteosynthesis using anatomically pre-contoured lateral clavicle locking plate is very important for the stabilization of vertically unstable lateral end clavicle fracture . Various studies can be taken into consideration regarding discussions surrounding use of screws, sutures, or EndoButton in management of unstable lateral end clavicle fractures. Motamedi et al. [34] reported that placement of coracoclavicular screws is technically very challenging and the use of these result in pull-out of the screw, breakage, screw head impingement and are therefore inferior to the use of EndoButton for coracoclavicular fixation. Moreover, these screws need to be removed before full ROM can be initiated. In a study conducted by Friedman et al. [35], only suture anchors were used for the fixation of unstable distal clavicle fracture and AC joint dislocation which led to failure of fixation due to suture anchor pull out and revision surgery was required. Robinson et al. [36] used EndoButton fixation alone without the plate for unstable lateral end clavicle fracture fractures and the construct was found to be unstable. Hence, in the study exploring the proposed surgical technique, EndoButton was used as the means of coracoclavicular reconstruction along osteosynthesis using anatomically pre-contoured lateral clavicle locking plate. In the study, all cases achieved union and no patient developed shoulder stiffness. This can be attributed to the fact that a locking plate provides stable and rigid fixation and if supported by coracoclavicular reconstruction, early ROM exercise can be started without the fear of implant pull out thereby minimizing the chances of shoulder stiffness. There was no case of EndoButton pullout or migration and none of the cases required a revision surgery for non-union, implant failure or hardware-related problems. There are studies which show that distal locking plates when used with coracoclavicular reconstruction gives excellent functional outcome. However, most of the studies have used suture anchors in combination with distal locking plate. These studies have reported suture anchor pull out and in some cases revision surgery was required. The use of EndoButton for coracoclavicular reconstruction along with distal locking plates has not been studied much. Our study shows that the functional outcome of distal locking plate with coracoclavicular reconstruction using tunneled suspensory device (EndoButton) is comparable to suture anchors when they are used along with the locking plates. However, complications were far less in our study as compared to suture anchors as there was no case of EndoButton migration and revision surgery.
Limitation of study
This study has certain limitations that should be acknowledged. First, the follow-up period was limited to 6 months, which, while sufficient to assess union and short-term function, may not capture long-term complications such as implant fatigue, hardware-related irritation, degenerative changes around the AC joint, or late implant migration. Second, the study was conducted at a single center with a modest sample size of 50 patients, which may restrict the generalizability of the findings to broader populations with varied demographics, surgical expertise, and rehabilitation protocols. Third, the absence of a comparative control group treated with alternative methods, such as plate fixation alone, suture anchors, or hook plates, limits the ability to establish the true superiority of the combined technique. In addition, functional outcomes were evaluated primarily using Constant-Murley and modified UCLA scores, without incorporation of other validated patient-reported measures such as DASH or PROMIS, potentially underrepresenting the impact on quality of life and daily activities.
This study aimed at evaluation of functional and radiological outcome of combined use of pre-contoured locking distal clavicle plate and tunneled suspensory device using EndoButton for the fixation for unstable lateral end clavicle fracture. As per the observation and results, this method of surgical fixation provides improvement in the functional and radiological parameters as compared to the other techniques described in literature.
For orthopedic surgeons, combined fixation using a pre-contoured locking distal clavicle plate and tunneled suspensory EndoButton device offers excellent radiological union and functional outcomes with minimal complications making it a reliable option for treating unstable lateral end clavicle fractures as compared to other surgical techniques.
References
- 1. Moseley HF. The clavicle: Its anatomy and function. Clin Orthop Relat Res 1968;58:17-27. [Google Scholar] [PubMed]
- 2. Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg 2002;11:452-6. [Google Scholar] [PubMed]
- 3. Koppe D, Reilmann H. Fractures of the lateral clavicle. Unfallchirurg 2010;113:45-52; quiz 53. [Google Scholar] [PubMed]
- 4. Neer CS 2nd. Nonunion of the clavicle. J Am Med Assoc 1960;172:1006-11. [Google Scholar] [PubMed]
- 5. Neer CS. Fractures about the shoulder. In: Ca R, Dp G, editors. Fracture, Dislocation. 2nd ed. Philadelphia PA: JB Lippincott; 1984. [Google Scholar] [PubMed]
- 6. Neer CS 2nd. Fractures of the distal third of the clavicle. Clin Orthop Relat Res 1968;58:43-50. [Google Scholar] [PubMed]
- 7. Craig EV. Fractures of the clavicle. In: Ca R, Fa M, editors. 2nd ed. Philadelphia PA: WB Saunders; 1998. [Google Scholar] [PubMed]
- 8. Edwards DJ, Kavanagh TG, Flannery MC. Fractures of the distal clavicle: A case for fixation. Injury 1992;23:44-6. [Google Scholar] [PubMed]
- 9. Ballmer FT, Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle. A report of five cases. J Bone Joint Surg Br 1991;73:291-4. [Google Scholar] [PubMed]
- 10. Fann CY, Chiu FY, Chuang TY, Chen CM, Chen TH. Transacromial Knowles pin in the treatment of Neer type 2 distal clavicle fracturesA prospective evaluation of 32 cases. J Trauma 2004;56:1102-5; discussion 1105-6. [Google Scholar] [PubMed]
- 11. Mall JW, Jacobi CA, Philipp AW, Peter FJ. Surgical treatment of fractures of the distal clavicle with polydioxanone suture tension band wiring: An alternative osteosynthesis. J Orthop Sci 2002;7:535-7. [Google Scholar] [PubMed]
- 12. Badhe SP, Lawrence TM, Clark DI. Tension band suturing for the treatment of displaced type 2 lateral end clavicle fractures. Arch Orthop Trauma Surg 2007;127:25-8. [Google Scholar] [PubMed]
- 13. Goldberg JA, Bruce WJ, Sonnabend DH, Walsh WR. Type 2 fractures of the distal clavicle: A new surgical technique. J Shoulder Elbow Surg 1997;6:380-2. [Google Scholar] [PubMed]
- 14. Herrmann S, Schmidmaier G, Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury 2009;40:236-9. [Google Scholar] [PubMed]
- 15. Johnston PS, Sears BW, Lazarus MR, Frieman BG. Fixation of unstable type II clavicle fractures with distal clavicle plate and suture button. J Orthop Trauma 2014;28:e269-72. [Google Scholar] [PubMed]
- 16. Seppel G, Lenich A, Imhoff AB. Distal clavicle fracture. Oper Orthop Traumatol 2014;26:254-62. [Google Scholar] [PubMed]
- 17. Bostman O, Manninen M, Pihlajamaki H. Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma 1997;43:778-83. [Google Scholar] [PubMed]
- 18. Shin SJ, KO YW, Lee J, Park MG. Use of plate fixation without coracoclavicular ligament augmentation for unstable distal clavicle fractures. J Shoulder Elbow Surg 2016;25:942-8. [Google Scholar] [PubMed]
- 19. Klein SM, Badman BL, Keating CJ, Devinney DS, Frankle MA, Mighell MA. Results of surgical treatment for unstable distal clavicular fractures. J Shoulder Elbow Surg 2010;19:1049-55. [Google Scholar] [PubMed]
- 20. Rieser GR, Edwards K, Gould GC, Markert RJ, Goswami T, Rubino LJ. Distal-third clavicle fracture fixation: A biomechanical evaluation of fixation. J Shoulder Elbow Surg 2013;22:848-55. [Google Scholar] [PubMed]
- 21. Schliemann B, Roßlenbroich SB, Schneider KN, Petersen W, Raschke MJ, Weimann A. Surgical treatment of vertically unstable lateral clavicle fractures (Neer 2b) with locked plate fixation and coracoclavicular ligament reconstruction. Arch Orthop Trauma Surg 2013;133:935-9. [Google Scholar] [PubMed]
- 22. Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res 1968;58:29-42. [Google Scholar] [PubMed]
- 23. Esenyel CZ, Ceylan HH, Ayanoglu S, Kebudi A, Adanir O, Bülbül M. Treatment of Neer type 2 fractures of the distal clavicle with coracoclavicular screw. Acta Orthop Traumatol Turc 2011;45:291-6. [Google Scholar] [PubMed]
- 24. Li Y, Shi S, Ou-Yang YP, Liu TL. Minimally invasive treatment for Neer IIb distal clavicle fractures with titanium cable. J Trauma 2014;5:73. [Google Scholar] [PubMed]
- 25. Brouwer KM, Wright TC, Ring DC. Failure of superior locking clavicle plate by axial pull-out of the lateral screws: A report of four cases. J Shoulder Elbow Surg 2009;18:e22-5. [Google Scholar] [PubMed]
- 26. Sajid S, Fawdington R, Sinha M. Locking plates for displaced fractures of the lateral end of clavicle: Potential pitfalls. Int J Shoulder Surg 2012;6:126-9. [Google Scholar] [PubMed]
- 27. Zhang C, Huang J, Luo Y, Sun H. Comparison of the efficacy of a distal clavicular locking plate versus a clavicular hook plate in the treatment of unstable distal clavicle fractures and a systematic literature review. Int Orthop 2014;38:1461-8. [Google Scholar] [PubMed]
- 28. Xu H, Chen WJ, Zhi XC, Chen SC. Comparison of the efficacy of a distal clavicular locking plate with and without a suture anchor in the treatment of Neer IIb distal clavicle fractures. BMC Musculoskelet Disord 2019;20:503. [Google Scholar] [PubMed]
- 29. Vikas V, Bhatia N, Jalan D, Prakash J, Singh J, Khare S. Clinical outcome of Neer type II lateral end clavicle fractures with coracoclavicular ligament disruption treated with pre-contoured locking plate and endobutton. Cureus 2021;13:e12585. [Google Scholar] [PubMed]
- 30. Largo RD, Rudin MA, Hotz TK, Valderrabano V, Käch KK. Anatomic reconstruction of unstable lateral clavicular fractures. J Trauma 2011;71:1348-51. [Google Scholar] [PubMed]
- 31. Morsy M, Hammad A. Osteosynthesis of unstable distal clavicular fractures with and without coracoclavicular ligament reconstruction. Egypt Orthop J 2017;52:202-7. [Google Scholar] [PubMed]
- 32. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987;214:160-4. [Google Scholar] [PubMed]
- 33. Amstutz HC, Sew Hoy AL, Clarke IC. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res 1981;155:7-20. [Google Scholar] [PubMed]
- 34. Motamedi AR, Blevins FT, Willis MC, McNally TP, Shahinpoor M. Biomechanics of the coracoclavicular ligament complex and augmentations used in its repair and reconstruction. Am J Sports Med 2000;28:380-4. [Google Scholar] [PubMed]
- 35. Friedman DJ, Barron OA, Catalano L, Donahue JP, Zambetti G. Coracoclavicular stabilization using a suture anchor technique. Am J Orthop (Belle Mead NJ) 2008;37:294-300. [Google Scholar] [PubMed]
- 36. Robinson CM, Akhtar MA, Jenkins PJ, Sharpe T, Ray A, Olabi B. Open reduction and endobutton fixation of displaced fractures of the lateral end of the clavicle in younger patients. J Bone Joint Surg Br 2010;92:811-6. [Google Scholar] [PubMed]