The subsidence rate of cementless femoral stems in patients who underwent hemiarthroplasty or total hip arthroplasty is potentially related to proximal femoral geometry, as reflected by the Dorr classification, and was lower in patients with a type A Dorr classification compared to types B and C.
Dr. Albagly Aviram, Department of Orthopedic Surgery, Bnai Zion Medical Center, Haifa, Israel. E-mail: aviram50@gmail.com
Introduction: Hip joint replacement surgeries, including total hip arthroplasty (THA) and hemiarthroplasty (HA), are highly successful for treating subcapital femoral neck fractures. However, femoral stem subsidence can negatively impact post-operative outcomes. This study investigates subsidence rates in relation to the geometry of the proximal femur.
Methods: A total of 255 patients who underwent cementless HA or THA were included, with follow-up data available for 74 patients who met the inclusion criteria. Pre- and post-operative variables included surgery type, age, sex, ASA score, and rehabilitation method. The cohort was divided into two groups based on femoral stem migration: a low subsidence group (0–4.99 mm) and a high subsidence group (>5 mm). Further subdivision was done according to the proximal femur morphology, which was classified by the Dorr Classification.
Results: 44 patients (or 59.5%) were classified as Dorr type A, 27 patients (or 36.5%) were type B, and only three patients (4.1%) were type C. Among patients with Dorr type A, 79.5% had low subsidence, while 20.5% had high subsidence. In Dorr type B, subsidence was nearly equal (51.9% low, 48.1% high). Two Dorr type C patients had low subsidence (66.6%), and one had high subsidence (33.3%). Results were statistically significant (P = 0.042). Multivariate analysis showed that type A patients were likelier to have low subsidence (OR 3.403, CI 1.221–9.486, P = 0.022).
Conclusion: The subsidence rate of cementless femoral stems was lower in patients with type A Dorr classification compared to types B and C. These findings suggest that structural geometric differences between the classifications may significantly affect susceptibility to subsidence.
Keywords: Total hip arthroplasty, hemiarthroplasty, femoral neck fracture, Dorr classification.
Femoral neck fractures represent a significant global health concern, especially among the elderly. They are associated with a substantial decline in quality of life and an elevated mortality risk. According to the Global Burden of Disease Study, which was conducted in 2019, it estimated that the prevalence of hip fractures globally was 14.2 million, with an incidence rate of 182/100,000 people [1]. Hip joint replacement surgeries, such as total hip arthroplasty (THA) and hemiarthroplasty (HA), are commonly indicated for displaced femoral neck fractures in the elderly population. These procedures generally exhibit high success rates and patient satisfaction [2,3]. However, comparative studies indicate that THA is associated with a higher risk of complications compared to HA [4,5]. One notable potential complication common to both THA and HA is the subsidence of the femoral stem, particularly concerning cementless stems that can sink into the femoral canal [6]. Subsidence is characterized by the distal migration of the femoral stem relative to the tip of the greater trochanter of the femur. In most cases, this phenomenon typically occurs within the first 6–8 weeks following the surgery [7,8,9]. Evidence in the literature suggests that subsidence occurs even several months and years after the initial procedure. Migliorini et al. reported a mean subsidence rate of 2.6 mm in THA patients after a follow-up period of 14.4 months [10]. In contrast, Rubio et al. observed a significant subsidence rate even after a follow-up of 10 years [11]. Subsidence of cementless femoral stems has been associated with several complications, including aseptic loosening of the implant, which increases the risk of femoral fracture [12], reduces soft tissue tension, raising the risk of dislocation [13], and contributes to leg-length discrepancy [14]. These factors frequently compromise the longevity of the hip arthroplasty, potentially leading to early failure. This study aimed to identify subsidence rates based on the Dorr classification for proximal femur morphology. We assume there is a possible connection between advanced types of Dorr classification (types B and C) and a higher subsidence rate.
This is a retrospective case–control study in which we analyzed the subsidence rate in 74 patients diagnosed with subcapital femur fractures who underwent HA or THA in our department between 2020 and 2023. Inclusion criteria consisted of patients with fully displaced subcapital femoral neck fractures classified as Garden stages 3 or 4, aged above 60, who received a cementless stem and participated in weight-bearing activities during the post-operative period, either through home or institutional rehabilitation (Fig. 1).
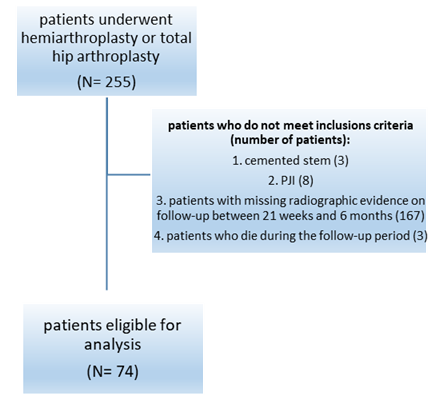
Figure 1: Flow chart of patient’s selection process.
All patients underwent surgery utilizing either the Corail or H-MAX collarless fully porous coated hydroxyapatite stem from the Johnson and Johnson DePuy (25 patients) or Lima Corporate (49 patients), which features a similar design and general concept. None of the patients required revision of the femoral and/or acetabular component during the follow-up time period. The bipolar head features a two-piece design, allowing motion between the components. This standardization of implant types was essential for maintaining consistency in our evaluation of subsidence rates.
Patients who underwent cemented hip replacement, those treated with non-weight-bearing protocols, those lost to follow-up, and those who experienced post-operative prosthetic joint infections or died during the follow-up period were excluded from this study. The minimum follow-up duration was 21 days, while the maximum was extended to 6 months. Preoperative variables included age, gender, and ASA score. The primary objective was to divide the cohort into two groups based on femoral stem subsidence: One group with a low rate of subsidence (0–4.99 mm) and another with a high rate of subsidence (>5 mm). Each group was further subdivided according to the proximal femur morphology as classified by the Dorr classification. The Dorr classification assesses the quality of the proximal femur based on radiographic, biochemical, and histological characteristics. Thick and well-defined cortices characterize type A, while Type B indicates bone loss from the medial and posterior cortices, leading to a broader diaphyseal canal, and Type C reflects significant loss of the medial and posterior cortices, resulting in decreased bony definition of the cortices [15]. In this study, we assessed the Dorr classification through quantitative measurements by calculating the canal diameter 10 cm distal to the lesser trochanter and dividing it by the inner canal diameter at the mid-portion of the lesser trochanter [15] (Fig. 2). A ratio of <0.5 mm was classified as Dorr type A, a ratio between 0.5 and 0.75 mm as type B, and a ratio >0.75 mm as type C.

Figure 2: Anteroposterior radiograph of the left hip illustrates the Dorr criteria calculation (a/b = ratio for Dorr criteria).
Stem subsidence was evaluated by measuring the difference in distance from the greater trochanter’s highest point to the stem shoulder perpendicular to the axis of the femur stem. This was performed using an anteroposterior (AP) radiograph of the hip or pelvis, taken between 3 weeks and 6 months postoperatively, and compared to the initial post-operative AP radiograph (Fig. 3).
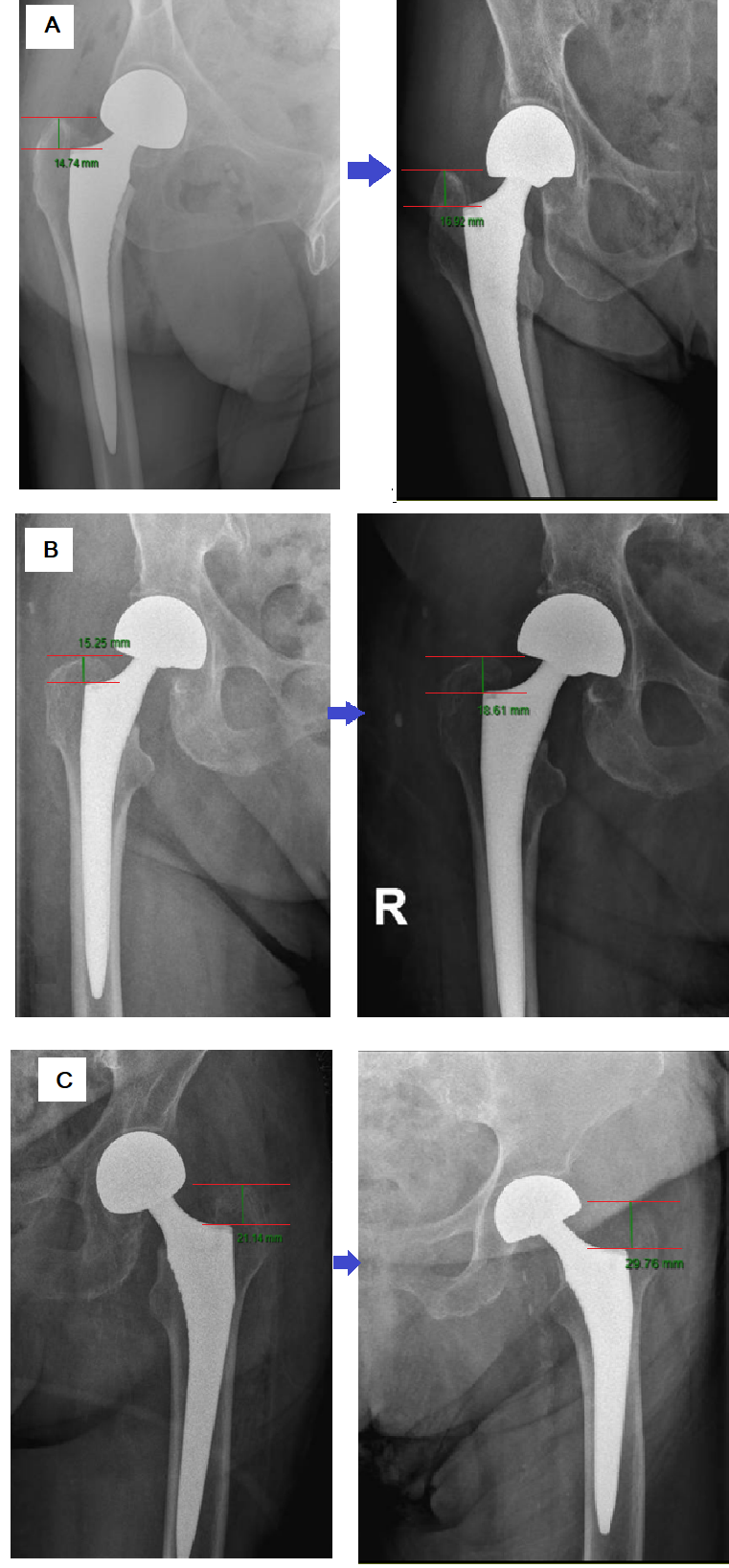
Figure 3: Anteroposterior radiograph of the hip shows the determination of femoral stem subsidence by calculating the difference in distance from the greater trochanter’s highest point to the stem shoulder perpendicular to the axis of the femur stem. All the implants in this figure are Lima Corporate implants. (a) Dorr type A patient, one day after hemiarthroplasty (HA) surgery (left) and 53 days after the surgery (right), showcases a subsidence rate of 2.18 mm. (b) Dorr type B patient, one day after HA surgery (left) and 44 days after the surgery (right), showcases a subsidence rate of 3.36 mm. (c) Dorr type C patient, one day after HA surgery (left) and 37 days after the surgery (right), showcases a subsidence rate of 8.62 mm.
All statistical analyses were conducted using SPSS statistical analysis software (IBM, version 29.0). A P < 0.05 was considered statistically significant for all the tests. The odds ratio (OR) and its corresponding 95% confidence interval (CI) were used for multivariant analysis.
A total of 255 patients who underwent HA or total arthroplasty at our institution between 2020 and 2023 were identified and included in the primary cohort. Among this initial group, 74 patients met the inclusion criteria. The exclusion of 167 patients was primarily due to the loss of follow-up and non-radiological evidence available during the follow-up period. Additional exclusion criteria are outlined above (Fig. 1). The mean follow-up period was 70.77 days. Table 1 demonstrates the demographic characteristics of the patients in detail. Among the cohort, 75.7% underwent HA, while the remaining 24.3% underwent THA. More than two-thirds (63.5%) of the cohort were female, and the mean age was 80.75 years, with nearly 80% of the patients being over 75 years old.
Table 1: Demographic characteristics of the cohort
Approximately equal numbers of patients were assigned to either home rehabilitation (35 patients) or institutional rehabilitation (39 patients). Most patients (66.2%) were classified as having an ASA score of 2 before surgery.
When further subdivided the cohort into DORR classification, 44 patients (or 59.5%) were classified as DORR type A, 27 patients (or 36.5%) were type B, and only 3 patients (4.1%) were type C. The second stage of the analysis involved dividing the cohort into two groups based on subsidence rate (Table 2). Upon analyzing the results, we found no statistically significant differences between the two groups regarding variables such as age, sex, rehabilitation status, or ASA score.
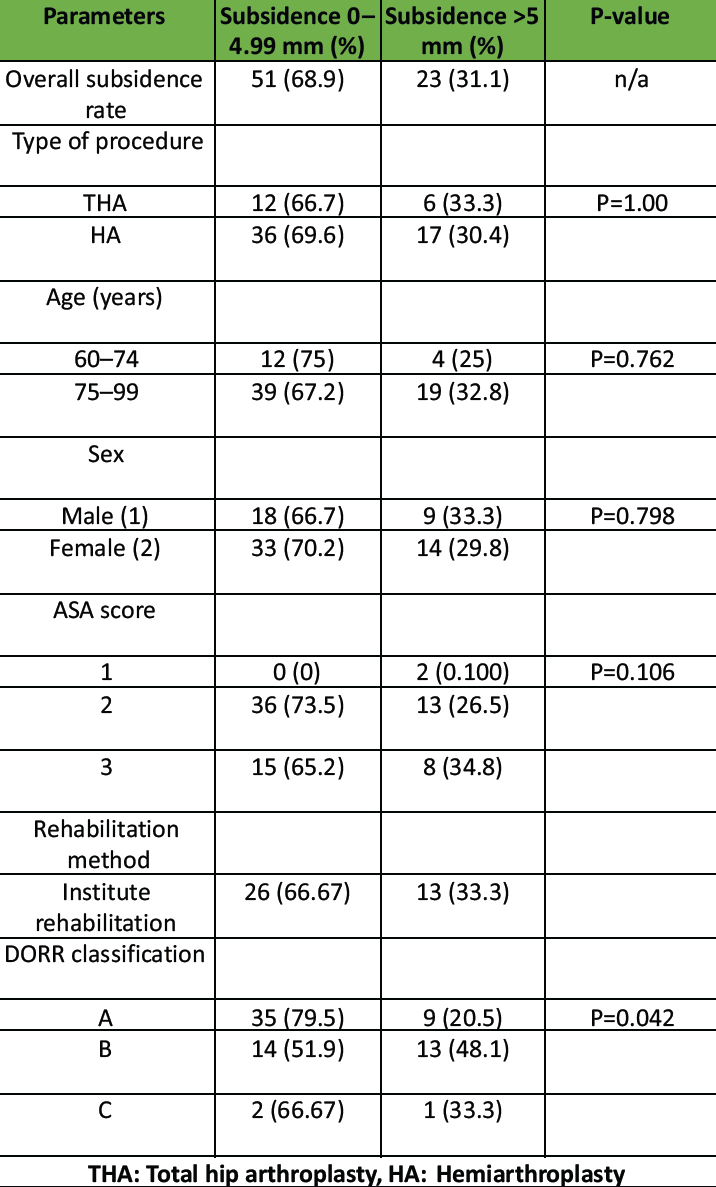
Table 2: Overview of subsidence rates in relation to patients’ characteristics
When examining the Dorr classification and its correlation to subsidence rate, we observed that among patients classified as Dorr type A, 79.5% experienced a low subsidence rate of 0–4.99 mm, while only 20.5% had a high subsidence rate of more than 5 mm. In contrast, patients classified as Dorr type B showed nearly equal distribution between low (51.9%) and high (48.1%) subsidence rates. For Dorr type C patients, there were only three individuals, of whom two had low subsidence rates, and one had a high subsidence rate exceeding 5 mm. These results were statistically significant, with a P = 0.042.
A subsequent multivariable analysis was conducted to identify predictors of low subsidence rates in patients with Dorr types A and combined types B and C (Table 3). We united Dorr types B and C due to the very low number of type C patients. The analysis revealed that patients classified as Dorr type A were more likely to have a low subsidence rate of 0–4.99 mm compared to those with Dorr types B or C, with an OR of 3.403 (CI of 1.221–9.486, P = 0.022.
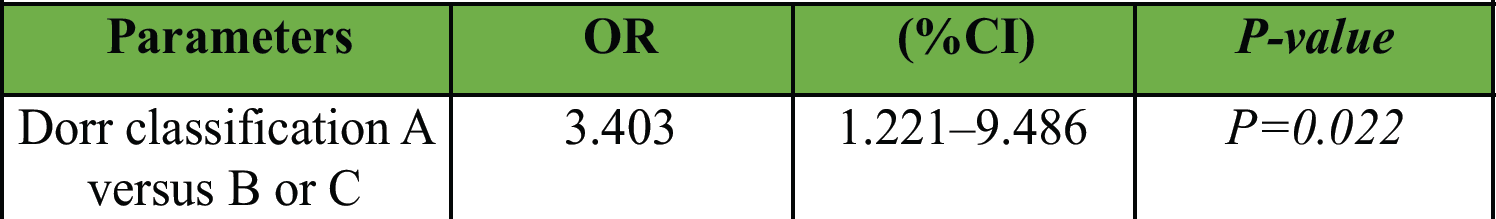
Table 3: Multivariant analysis – odds ratio for low subsidence rate in correlation with Dorr classification A versus B or C
In this study, we measured the subsidence rate for 74 patients who underwent either THA or HA. By analyzing the results, we found that most patients had a low subsidence rate of 0–4.99 mm (68.9%), and the mean subsidence rate was 4.53 mm (SD 3.62). The reasons for femoral stem subsidence are varied and well-documented in the literature. Contributing factors include stem design [7], the weight-bearing protocol following surgery (whether full weight-bearing or partial weight-bearing) [16], increasing age [17], and a high body mass index (BMI) [17]. In this article, we subdivided the cohort based on proximal femur morphology using the Dorr classification. Our analysis revealed that 59.5% of the patients were classified as Dorr type A, 36.5% were type B, and only three patients (4.1%) were classified as type C. This ratio of types A to B and C is consistent with the overall prevalence ratios of the Dorr classification reported in the literature. Gema et al. found that 83% of their patients were type A, approximately 16% were type B, and none were type C [18]. In contrast, Goldberg et al. reported that the prevalence of Dorr type A was 45.8%, type B was 38.9%, and type C was 15.3% [19]. The progression of osteoporotic changes in the proximal femur is closely linked to the bone’s ability to ingrown into the stem and achieve long-term incorporation between the stem and bone surfaces. Inadequate incorporation can lead to subsidence, along with subsequent complications such as loosening, fracture, and dislocation, which can adversely affect the overall outcome of the surgery. Therefore, understanding the proximal femoral anatomy is crucial for selecting the appropriate implant or fixation method. The Dorr classification provides a simple and efficient tool for understanding the morphology and matching it with the most suitable implant. Our results showed a positive correlation between advanced proximal femur morphology (Dorr classification type B and C) and high subsidence rates. The correlation between femoral stem subsidence and Dorr classification is poorly established in the literature. In their article, Gema et al. attempted to identify several factors contributing to femoral stem subsidence after HA, including Dorr classification, but found no statistically significant results [18]. Similarly, Bornes et al. [17] analyzed subsidence rates of femoral stems in THA concerning various associated factors and reported no significant association between subsidence of more than 5 mm and Dorr classification. The effect of anatomy and morphology of the proximal femur and femoral stem subsidence in patients undergoing arthroplasty can be attributed to several factors. Sah et al. [20] found that type A femurs exhibit greater bone density, while subjects with type C had lower T-scores compared to those with type B, who in turn had lower T-scores than type A. The severity of osteoporosis and bone quality in patients undergoing HA or THA is a critical factor influencing osseointegration, durability, and complications of the implanted prosthesis, including subsidence [21]. Furthermore, bone architecture and geometry have been recognized as key determinants of overall bone strength [22], which can significantly impact the subsidence rate following arthroplasty procedures. These geometric changes in the proximal femoral canal, influenced by Dorr classification, may occur with advancing age [23]. This indicates a positive correlation between Dorr classification and age-related changes in bone quality, which may, in turn, affect the rate of subsidence. This article has several limitations. While our hypothesis posits that Dorr classification may influence the subsidence rate of the femoral stem following arthroplasty, we did not account for other comorbidities that could affect this outcome. Specifically, although we operated under the assumption that all patients had osteoporosis or osteopenia, we could not calculate the T-score for each patient to accurately assess the level of these conditions. Furthermore, this analysis did not include factors such as BMI and alignment, which may impact subsidence rates. Moreover, preoperative variables such as age, gender, and home rehabilitation were deemed statistically insignificant, preventing us from considering them in our OR calculations for low subsidence rates. In addition, we acknowledge that our patient pool is relatively small. This limitation arises from the fact that many patients were lost to follow-up and did not provide radiological evidence during the post-operative period between 3 weeks and 6 months.
The subsidence of cementless femoral stems in patients with type A Dorr classification was lower than in patients with types B and C. These findings suggest that structural and geometric differences in the proximal femur between these classifications may significantly influence susceptibility to subsidence, potentially reducing the risk of complications. The authors recommend further investigation into these factors to enhance surgical techniques and implant designs, with the goal of minimizing subsidence risk and improving outcomes in orthopedic applications.
Preoperative assessment of femoral geometry in patients with subcapital femoral neck fractures may help reduce stem subsidence, guide implant selection, and lower the risk for post-operative complications
References
- 1. Dong Y, Zhang Y, Song K, Kang H, Ye D, Li F. What was the epidemiology and global burden of disease of hip fractures from 1990 to 2019? Results from and additional analysis of the global burden of disease study 2019. Clin Orthop Relat Res 2023;481:1209-20. [Google Scholar] [PubMed]
- 2. Learmonth ID, Young C, Rorabeck C. The operation of the century: Total hip replacement. Lancet 2007;370:1508-19. [Google Scholar] [PubMed]
- 3. Wang Z, Bhattacharyya T. Outcomes of hemiarthroplasty and total hip arthroplasty for femoral neck fracture: A Medicare cohort study. J Orthop Trauma 2017;31:260-3. [Google Scholar] [PubMed]
- 4. Avery PP, Baker RP, Walton MJ, Rooker JC, Squires B, Gargan MF, et al. Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: A seven- to ten-year follow-up report of a prospective randomised controlled trial. J Bone Joint Surg Br 2011;93:1045-8. [Google Scholar] [PubMed]
- 5. Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am 2006;88:2583-9. [Google Scholar] [PubMed]
- 6. Campbell D, Mercer G, Nilsson KG, Wells V, Field JR, Callary SA. Early migration characteristics of a hydroxyapatite-coated femoral stem: An RSA study. Int Orthop 2011;35:483-8. [Google Scholar] [PubMed]
- 7. Al-Najjim M, Khattak U, Sim J, Chambers I. Differences in subsidence rate between alternative designs of a commonly used uncemented femoral stem. J Orthop 2016;13:322-6. [Google Scholar] [PubMed]
- 8. Selvaratnam V, Shetty V, Sahni V. Subsidence in collarless corail hip replacement. Open Orthop J 2015;9:194-7. [Google Scholar] [PubMed]
- 9. Mukherjee K, Ghorai TK, Kumar A. High grade femoral stem subsidence in uncemented hip hemiarthroplasty – A radiographic analysis and an early prediction while treating femoral neck fractures. Int Orthop 2023;47:1591-9. [Google Scholar] [PubMed]
- 10. Migliorini F, Maffulli N, Pilone M, Velaj E, Hofmann UK, Bell A. Demographic characteristics influencing the stem subsidence in total hip arthroplasty: An imaging study. Arch Orthop Trauma Surg 2023;144:887-94. [Google Scholar] [PubMed]
- 11. Rubio I, Bellostas L, García-Rey E. Radiological subsidence and acetabular erosion after tapered uncemented hemiarthroplasty in femoral neck fractures a 10- to 13- year follow-up study. Injury 2020;51 Suppl 1:S37-41. [Google Scholar] [PubMed]
- 12. Streit MR, Haeussler D, Bruckner T, Proctor T, Innmann MM, Merle C, et al. Early migration predicts aseptic loosening of cementless femoral stems: A long-term study. Clin Orthop Relat Res 2016;474:1697-706. [Google Scholar] [PubMed]
- 13. Pentlow AK, Heal JS. Subsidence of collarless uncemented femoral stems in total hips replacements performed for trauma. Injury 2012;43:882-5. [Google Scholar] [PubMed]
- 14. Sculco PK, Cottino U, Abdel MP, Sierra RJ. Avoiding hip instability and limb length discrepancy after total hip arthroplasty. Orthop Clin North Am 2016;47:327-34. [Google Scholar] [PubMed]
- 15. Wilkerson J, Fernando ND. Classifications in brief: The Dorr classification of femoral bone. Clin Orthop Relat Res 2020;478:1939-44. [Google Scholar] [PubMed]
- 16. Leiss F, Götz JS, Meyer M, Maderbacher G, Reinhard J, Parik L, et al. Differences in femoral component subsidence rate after THA using an uncemented collarless femoral stem: Full weight-bearing with an enhanced recovery rehabilitation versus partial weight-bearing. Arch Orthop Trauma Surg 2022;142:673-80. [Google Scholar] [PubMed]
- 17. Bornes TD, Radomski LR, Bonello JP, Mortensen-Truscott L, Safir OA, Gross AE, et al. Subsidence of a single-taper femoral stem in primary total hip arthroplasty: Characterization, associated factors, and sequelae. J Arthroplasty 2023;38:S174-8. [Google Scholar] [PubMed]
- 18. Gema A, Irianto KA, Setiawati R. Femoral stem subsidence and its associated factors after cementless bipolar hemiarthroplasty in geriatric patients. Malays Orthop J 2021;15:63-71. [Google Scholar] [PubMed]
- 19. Goldberg T, Torres A, Bush JW, Mahometa MJ. Quantification of the Dorr classification system. Orthop Proc 2019;101-B(Suppl 4):67. [Google Scholar] [PubMed]
- 20. Sah AP, Thornhill TS, LeBoff MS, Glowacki J. Correlation of plain radiographic indices of the hip with quantitative bone mineral density. Osteoporos Int 2007;18:1119-26. [Google Scholar] [PubMed]
- 21. Delsmann MM, Strahl A, Mühlenfeld M, Jandl NM, Beil FT, Ries C, et al. High prevalence and undertreatment of osteoporosis in elderly patients undergoing total hip arthroplasty. Osteoporos Int 2021;32:1661-8. [Google Scholar] [PubMed]
- 22. Pulkkinen P, Partanen J, Jalovaara P, Jämsä T. Combination of bone mineral density and upper femur geometry improves the prediction of hip fracture. Osteoporos Int 2004;15:274-80. [Google Scholar] [PubMed]
- 23. Veldman HD, Boymans TA, Van Steenbergen LN, Heyligers IC. Age-associated changes in proximal femur morphology affect femoral component sizing in cementless hip arthroplasty. Geriatr Orthop Surg Rehabil 2022;13:21514593221144615. [Google Scholar] [PubMed]