Clinical examination plays a critical role in sciatica-related pathologies, which got misdiagnosed in this case. Discrepancy between MRI and clinical signs should prompt reconsideration in the diagnosis.
Dr. Neel Shah, Department of Orthopaedics, Ashirwad Hospital, Vadodara, Gujarat, India. E-mail: Shahneel89@gmail.com
Introduction: Nerve tumors are rare entities with variable presentation from pain, numbness, burning, to variable motor deficits. The most common nerve tumors are Schwannoma and Neurofibroma, which arise from the nerve sheath. Rarely tumor arises from the epineural tissue of the nerve, such as hemangioma, engiometosis, paraganglioma, lipoma, and glomus tumor.
Case Report: We are reporting an extremely rare case of Glomus tumor in a 48-year-old female from the most proximal part of the sciatic nerve extending from the L4-5 region in the retroperitoneal space inside the pelvis to the extra-pelvic region up to inferior gluteal fold. Surgery was performed and a partial excision and decompression were performed. The patient had good pain relief after surgery.
Conclusion: The case highlights the importance of clinical findings, early detection, and multidisciplinary management of Nerve tumor to optimize patient outcomes. To our knowledge, this is the only case of glomus tumor involving the proximal part of the sciatic nerve with intrapelvic and extrapelvic extension reported in the literature.
Keywords: Glomus tumor, sciatic nerve, sciatica, nerve, spine, endoscopy.
Glomus tumor is a rare benign vascular tumor usually found in sites rich in glomus bodies, such as the subungual region of digits and the skin of palm, forearm, and leg [1,2]. Involvement of nerve is very rare. Only 12 cases of glomus tumor have been reported till February 2017, and out of which only 3 cases that are sciatic nerve glomus tumor [3]. However, no case with involvement of the proximal sciatic nerve with intra- and extra-pelvic extension described so far. Sciatic nerve involvement can mimic sciatica or nerve entrapment syndromes [4,5]. This report discusses the diagnosis, misdiagnosis, surgical treatment, and outcomes of a sciatic nerve glomus tumor.
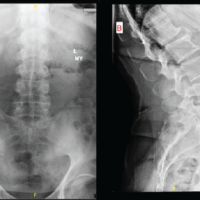
A 48-years-old female presented to us with complains of radiating pain in the left lower limb, burning, weakness, and foot drop since 3 years. Pain was continuous throughout the day with no specific aggravating factor. Pain was not responding to analgesics and other medicines for neuropathic pain. Before 1 year, the patient presented to a spine surgeon with the same complains and magnetic resonance imaging (MRI) of the spine revealed L4-5 disc prolapse for which she underwent endoscopic L4-5 discectomy (MRI photo). No mention of the sciatic nerve tumour was made. However, the patient did not get any relief but gradually complain worsened. Patient was not able to stand/walk for more than 5 min.
Examination
The patient was walking with high-stepping gait on the left lower limb. On examination of the lumbar spine, mild tenderness was present at L4-5 midline and left paraspinal region. A small operative scar was present (2 × 1 cm) in the left paraspinal region at L4-5 level. Straight leg raise (SLR) was 90° and pain-free on the right side, while the left side SLR was 40° and very painful. The hip joint was normal. No swelling in the distal leg or foot was present. Distal pulsations were normal. Neurological examination revealed Medical Research Council grade S2 sensory changes (superficial sensation) at L5–S1 dermatome. L2-3-4 dermatome was normal. Motor examination of the left lower limb revealed tibialis anterior and extensor hallucis longus grade 1, extensor digitorum longus grade 3, tibialis posterior grade 1, Quadriceps was grade 5, hamstring and gastrosoleus were grade 4. Hip muscles were grade 5. Knee reflex was present while ankle reflexes were absent on the left side.
Investigations
Since the examination findings were not in concurrence with the previous MRI showing mild L4-L5 disc prolapse, we decided to go for a thorough evaluation.
X-ray lumbosacral Spine – Normal
Nerve conduction velocity study – showed left sciatic nerve neuropathy
MRI – Hyperintense lesion in the sciatic nerve along the L4, L5, and S1 fibers, starting in the retroperitoneum and extending beyond the greater sciatic foramen. Approximate length was 20 cm (Figs. 1 and 2).

Figure 1: Magnetic resonance imaging scan T1 image OD sciatic nerve showing thickened with a fusiform appearance. The green arrow marled (L) in image shows the tumour while the marke (R) shows normal sciatic nerve.

Figure 2: Magnetic resonance imaging scan T1 image showing hyperintensity along the course of sciatic nerve.
Ultrasonography – Large, elongated hypoechoic lesion involving the sciatic nerve in the retroperitoneum, proximal and distal to the greater sciatic foramen (Fig. 3).
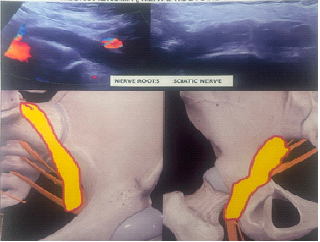
Figure 3: Ultrasonography image and demonstration of sciatic nerve tumor in the pelvis.
Treatment
Patient and relatives were explained that while pain relief after surgery is achievable, restoration of motor function and muscle power may be limited, depending on the extent of nerve involvement and pre-operative deficits.
The patient was planned for surgical excision under general anesthesia.
Multidisciplinary team of Orthopedic Surgeon, Plastic Surgeon, and Oncosurgeon was involved.
Under general anesthesia, the pararectus approach was used to explore the tumor. After dissecting the common, internal, and external iliac arteries and vein, tumor was identified near the sciatic foramen (Fig. 4); however, proximally, the tumor was right behind the common iliac vein, which looked flattened and thrombosed. The sciatic nerve sheath was incised longitudinally along the length, which exposed the tumor tissue. The tumor was grayish in color and fragmented nerve fibers were coming out along with the tumor tissue. Intraoperative morphology was different from the pre-operative diagnosis of schwannoma or neurofibroma. There was no delineation between tumor and nerves; to avoid further neurological damage, only decompression was performed.
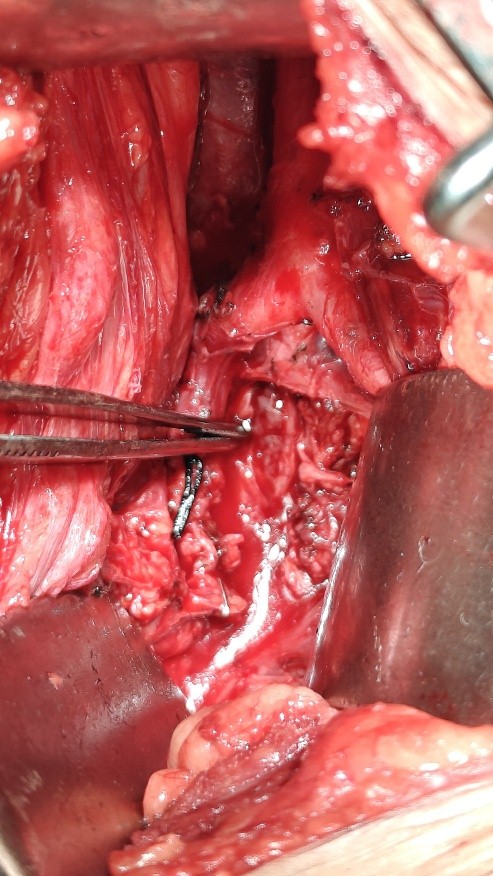
Figure 4: Showing sciatic nerve, behind the bifurcation of common iliac artery, through pararectus approach.
The patient was turned laterally, and tumor was exposed posteriorly from the Kocher-Langenbeck approach of the hip. The nerve, as shown in the figure, was thickened and firm. The nerve sheath was incised, but no tumor delineation was possible (Fig. 5). A small finger-like extension coming out from the sciatic nerve was present over the surface of about 1.5 cm, which was excised (glomangiomatosis) and sent for histopathological examination. A biopsy was also taken after decompression of the nerve and the wound was closed.
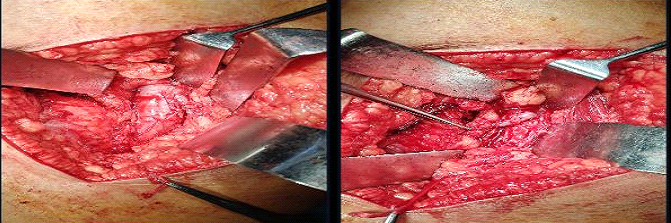
Figure 5: Showing the sciatic nerve through the Kocher-Langenback approach, the first image shows the sciatic nerve after dissection, and the second after longitudinal incision over the nerve.
Histopathology
Expanded nerve fascicles with a low-grade neoplasm composed of uniform plump spindle to oval with increased vascularity; features are not of a nerve sheath tumor. Histopathology was inconclusive so Immunohistochemistry was advised.
Immunohistochemistry
Smooth muscle actin – positive, calponin – positive, and S-100, epithelial membrane antigen and CD 34 negative, confirmed the diagnosis of glomus tumor of the sciatic nerve [6,2] (Fig. 6).
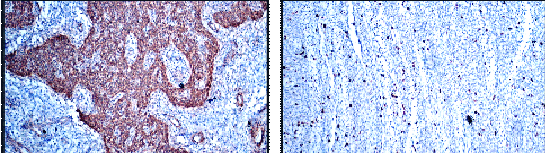
Figure 6: Immunohistochemistry showing positive for Calponin and K67 markers.
Outcome and follow-up
Post-operatively, both anterior and posterior wounds healed well. The patient had developed deep vein thrombosis (DVT) of the common femoral vein post-operatively. The patient had no relief for initially 10 days. DVT was treated conservatively with enoxaparin and resolved in 8 weeks. At 3 months, the patient had near complete resolution of pain; however, foot drop persisted. Patient was able to walk with a foot drop splint and stick. Pain relief was unexpected as the tumor was not removed completely. The patient was explained about the prognosis, chances of recurrence of pain and/or increase in the size of the tumor requiring further surgery. Any future surgery would again require reexploration of the tumour and possible vascular intervention as risk of vascular injury is high. The patient was advised MRI evaluation of the sciatic nerve every 6 months.
Glomus tumors typically occur in the digits, palm, or nail beds but rarely involve deep structures, such as peripheral nerves [1,7]. Sciatic nerve glomus tumors are extremely uncommon and can mimic sciatica, piriformis syndrome, or lumbar radiculopathy, which are common presentations in the middle-aged group. We could find only 3 reported cases till date [3,4,8]. Clinical examination remains a cornerstone in diagnosing nerve tumors, guiding further investigations and treatment decisions. A thorough assessment helps differentiate between neuropathic and musculoskeletal causes of symptoms, ensuring timely intervention. Key findings, such as localized tenderness, Tinel’s sign, and motor deficits, provide crucial clues for accurate diagnosis and surgical planning. The patient even underwent an endoscopic discectomy, which was not required. Diagnosis is usually delayed in such cases [9]. In our case, the diagnosis was reached at 3 years. MRI is essential for diagnosis, but glomus tumors may be mistaken for schwannomas or neurofibromas. [10] Any surgical intervention is challenging to explore the proximal sciatic nerve and sacral plexus. Both anterior and posterior approaches are described for intra-pelvic exploration of the sciatic nerve, but we selected ant pararectus approach. Presence of the large tumor in the region of L5 and S1 is also likely to compress iliac artery and vein, and we found the same in our case, where the common iliac vein was completely flattened and adherent to the tumor, and it was not possible to dissect it. The chances of Venus complications after the operation are likely. DVT of the proximal femoral vein occurred in our case post-operatively. Surgery of the tumor in this part needs a multidisciplinary team and, in this case, along with an orthopedic surgeon, a plastic surgeon having experience of nerve tumors, and an oncosurgeon having experience of pelvic tumors, where part of our surgical team. Complete surgical excision in a sciatic nerve tumor is not possible, so limited decompression/excision should be undertaken by an experienced surgeon. Histopathology and immunochemistry are very helpful for the accurate diagnosis of a glomus tumor. To our knowledge, this is the first case of a glomus tumor of the most proximal part of the sciatic nerve and so there is no comparison for management and prognosis of this tumor.
This is the first case of glomus tumor of the proximal part of the sciatic nerve with intra- and extra-pelvic extension reported in the literature. This case highlights the importance of considering a glomus tumor in patients with atypical sciatic pain. A thorough clinical and radiological evaluation is crucial for timely diagnosis and surgical intervention.
When a patient comes with prolonged radicular pain in the lower limb, a Sciatic nerve tumor should also be considered as a differential diagnosis.
References
- 1. Shinohara T, Hirata H. Glomus tumor originating from a digital nerve. Plast Reconstr Surg Glob Open 2019;7:e2053. [Google Scholar] [PubMed]
- 2. Donato G, Iofrida G, Amorosi A. Images in pathology. Glomangioma of the sural nerve. Int J Surg Pathol 2006;14:332-3. [Google Scholar] [PubMed]
- 3. Frimpong D, Naz S, Kadhum M, Rogut M, Farooque T, O’Neill J, Fleming A. A Rare Case of Cutaneous Intraneural Glomus Tumour. J Cutan Pathol. 2025 Feb 8. doi: 10.1111/cup.14793. Epub ahead of print. PMID: 39921470 [Google Scholar] [PubMed] [CrossRef]
- 4. Nwankwo BO, Henshaw RM, Kumar D. Glomus tumor of the sciatic nerve: An extraspinal cause of sciatica. Orthopedics 2018;41:e151-3. [Google Scholar] [PubMed]
- 5. Scheithauer BW, Rodriguez FJ, Spinner RJ, Dyck PJ, Salem A, Edelman FL, et al. Glomus tumor and glomangioma of the nerve. Report of two cases. J Neurosurg 2008;108:348-56. [Google Scholar] [PubMed]
- 6. Gombos Z, Zhang PJ. Glomus tumor. Arch Pathol Lab Med 2008;132:1448-52. [Google Scholar] [PubMed]
- 7. Mitchell A, Spinner RJ, Ribeiro A, Mafra M, Mouzinho MM, Scheithauer BW. Glomus tumor of digital nerve: Case report. J Hand Surg Am 2012;37:1180-3. [Google Scholar] [PubMed]
- 8. Tropet Y, Menez D, Billerey C, Vichard P. Tumeur glomique du nerf sciatique [Glomus tumor of the sciatic nerve]. Ann Chir Plast Esthet 1991;36:204-8. [Google Scholar] [PubMed]
- 9. Nebreda CL, Urban BJ, Taylor AE. Upper extremity pain of 10 years duration caused by a glomus tumor. Reg Anesth Pain Med 2000;25:69-71.</p> [Google Scholar] [PubMed]
- 10. <p>10. Kim SW, Jung SN. Glomus tumour within digital nerve: A case report. J Plast Reconstr Aesthet Surg 2011;64:958–60. [Google Scholar] [PubMed]