Prompt recognition of irreducible hip dislocation is critical to prevent iatrogenic femoral neck fractures and enables successful head-preserving management even in elderly patients.
Dr. Satyendra Kumar, Senior Resident, Department of Orthopaedics, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India. E-mail: satyendradagur4@gmail.com
Introduction: Iatrogenic femoral neck fractures following attempted closed reduction of irreducible posterior hip dislocations are extremely rare and underreported. This case highlights the importance of pre-reduction evaluation and presents the first known report of successful osteosynthesis in an elderly patient.
Case Report: A 55-year-old Indian female presented with a posterior hip dislocation and femoral head fracture (Pipkin type I) following a road traffic accident. During attempted closed reduction, an audible crack was noted. Imaging revealed an iatrogenic femoral neck fracture, converting the injury to a Pipkin type III configuration. The patient underwent open reduction and internal fixation using a modified Gibson approach and Ganz trochanteric osteotomy. Post-operative rehabilitation included staged weight-bearing and physical therapy. The patient achieved fracture union with an excellent Harris Hip Score of 96.8 at 18 months of follow-up.
Conclusion: This is the first reported case demonstrating successful osteosynthesis in a Pipkin type III fracture-dislocation due to an iatrogenic neck fracture in an elderly patient. The case emphasizes the role of thorough assessment before reduction and the feasibility of head preservation techniques even in elderly patients with good bone stock.
Keywords: Irreducible hip dislocation, iatrogenic femoral neck fracture, Pipkin type III, osteosynthesis, trochanteric flip osteotomy.
Hip dislocations are typically the result of high-velocity trauma, with posterior dislocations being the most common type. Approximately 5–15% of these cases are associated with fractures of the femoral head [1]. In cases of dislocations accompanied by femoral head fractures, urgent closed reduction has been the primary approach for management, which is then succeeded by definitive treatment (whether closed or open) focused on the anatomical restoration of both the fractures and any joint incongruities [2]. Irreducible injuries, often referred to as “locked or fixed” dislocations, have been discussed in several studies. In addition, iatrogenic femur fractures are infrequent but recognized complications associated with these types of dislocations [3,4,5]. Along with hip dislocation, a fracture involving both the femoral head and neck is categorized as a type III femoral head fracture-dislocation under the Pipkin classification [6]. This type of injury is a rare form of femoral head injury documented in the literature, and its prognosis has been noted to be unfavorable, with most cases needing total hip replacement (THR) [7]. In the present case, we report a rare instance of an iatrogenic femoral neck fracture that occurred during attempted closed reduction of an irreducible posterior hip fracture dislocation in an elderly patient. The fracture was successfully treated by osteosynthesis with three cancellous cannulated screws using the modified Gibson approach and Ganz trochanteric osteotomy, resulting in favorable functional outcomes at 18 months of follow-up. To the best of our knowledge and based on the available literature, this is the first reported case of its kind managed with this approach in an elderly patient, demonstrating excellent functional results. This underscores the importance of a patient-specific treatment strategy in the management of complex proximal femoral fractures, particularly in patients aged 45–59 years, where both fixation and arthroplasty remain viable depending on bone quality, activity level, and physiological age [8,9,10,11,12].
A 55-year-old female with no known comorbidities presented to the emergency department of our tertiary care center with complaints of pain in the right hip and inability to bear weight on the right lower limb following an alleged history of a road traffic accident. The patient was initially evaluated in the emergency, and her right hip was flexed, adducted, and internally rotated with no distal neurovascular deficit. There was no history of loss of consciousness, vomiting, or abdominal pain, suggesting any soft organ injury. Initial evaluations, including X-rays, revealed a posterior hip dislocation with a Pipkin type I femoral head fracture (Fig. 1). A closed reduction attempt under conscious sedation was taken, and during the reduction maneuver, while applying longitudinal traction, an audible crack was heard. Subsequently, a C-arm image was taken, and a computed tomography scan was performed, suggestive of an iatrogenic femoral neck fracture in a previously recognized femoral head fracture dislocation (Fig. 2 and 3).
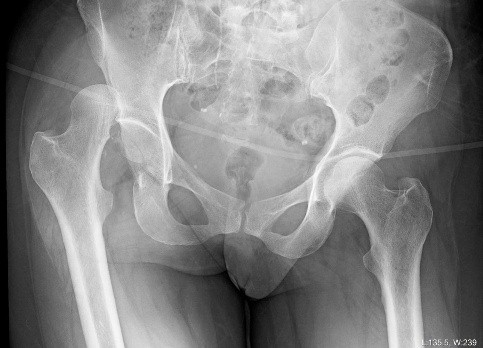
Figure 1: Anteroposterior view of pelvis with both hips showing posterior hip fracture dislocation on the right side.

Figure 2: C-arm image of the right hip showing an iatrogenic femoral neck fracture after attempted closed reduction.
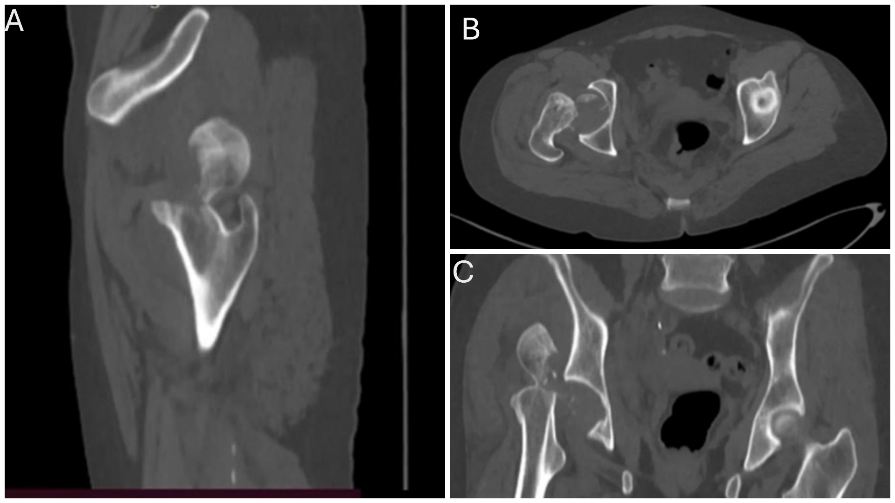
Figure 3: Computed tomography of the pelvis showing femoral neck fracture in sagittal (a) and coronal view (b) showing fractured femur head fragment, (c) and axial view .
On the same day, considering the patient’s borderline age of 45–59 years, bone quality, and following a thorough discussion with the patient, a decision was made to proceed with osteosynthesis, and the patient was taken to the operating room. Under general anesthesia, the patient was positioned in the lateral decubitus position, and a modified Gibson approach was taken [13]. A trochanteric flip osteotomy was performed as described by Ganz et al. [14] to enhance visualization. A Z-shaped capsulotomy was then made to expose the femoral neck and proximal femur. The posterosuperior capsule, which was obstructing the reduction of the proximal femur, was incised under direct vision. The femoral neck fracture was then anatomically reduced and stabilized using cancellous cannulated screws inserted percutaneously under fluoroscopic guidance. Particular attention was paid to screw trajectory and placement to avoid compromising the femoral head fracture fragment. Following this, an anterior dislocation of the hip was performed, and the fractured segment of the femoral head was carefully retrieved from the acetabulum. Intraoperatively, the fractured segment of the femoral head was found to be infrafoveal, comminuted, and non-reconstructable. Therefore, excision of the fragment was performed. The hip’s range of motion was assessed and found to be stable. The anterior capsule was repaired, and the trochanteric osteotomy was fixed using two cancellous screws (Fig. 4). The wound was closed in layers. The patient withstood the surgery well, and the post-operative period was uneventful. The patient was mobilized with non-weight-bearing ambulation using a walker from post-operative day 1.
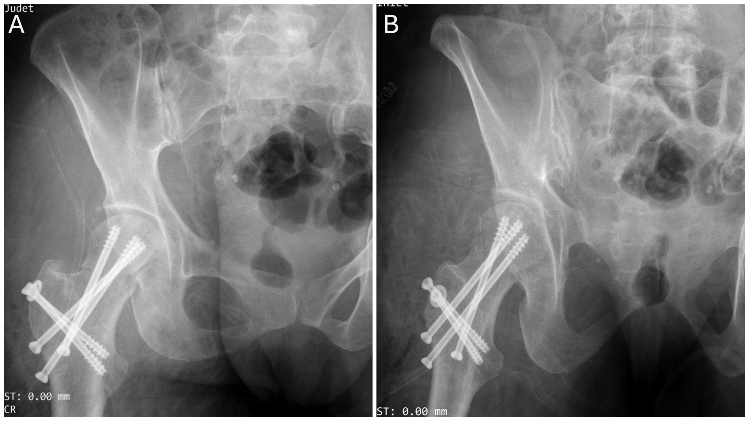
Figure 4: Image showing immediate post-operative X-ray (a) anteroposterior and (b) lateral view of right hip.
Sutures were removed after 2 weeks, and the wound had healed well. The patient was followed up monthly for the first 6 months, and then every 3 months up to 1 year. Partial weight-bearing was initiated at 8 weeks, progressing to full weight-bearing by 12 weeks, at which point complete fracture union was achieved (Fig. 5).
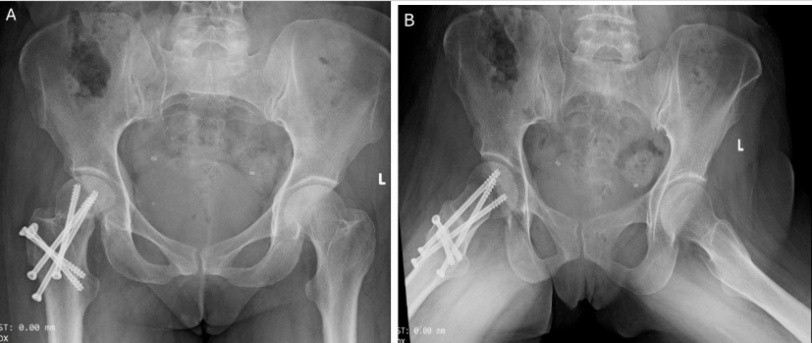
Figure 5: Post-operative X-ray at 3 months showing union at femoral neck fracture (a) anteroposterior and (b) lateral views.
At the 18-month follow-up, there were no signs of avascular necrosis of the femoral head, and the patient was able to walk comfortably with a good range of motion, and the patient’s Harris Hip Score was 96.80, signifying an excellent functional outcome (Figs. 6 and 7).
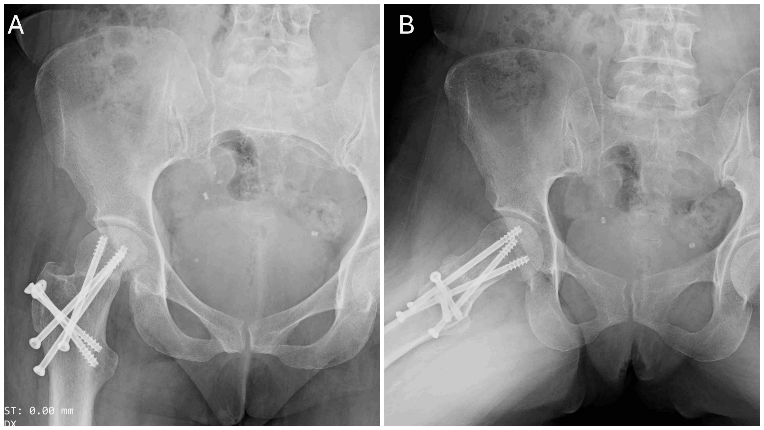
Figure 6: Post-operative X-ray at 18 months showing no sign of avascular necrosis of the femoral head in (a) anteroposterior and (b) lateral views of the right hip.

Figure 7: (A-D) Clinical images of the patient.
Hip dislocations are usually due to high-energy trauma. It can compromise the vascular supply to the femoral head. A prolonged dislocation significantly increases the risk of avascular necrosis (AVN). Therefore, urgent closed reduction is critical to minimize the risk of poor outcomes [15]. Irreducible femoral head fracture-dislocation is a rare variant of posterior hip dislocation, accounting for approximately 9% of all cases, and poses significant therapeutic challenges [4]. The irreducibility of the hip is often unrecognized, which may lead to iatrogenic femoral neck fractures during attempted reduction [3]. Mehta et al. [4] emphasized the importance of thorough clinical and radiological evaluation in cases of posterior hip dislocation associated with Pipkin type I or II femoral head fractures, to identify irreducible dislocations. Clinically, an irreducible hip dislocation typically presents with the affected lower limb in a fixed position of slight flexion, with immobility in neutral or mild internal rotation, and apparent shortening of the limb. In contrast, a routine posterior hip dislocation usually shows the limb in adduction and flexion, but remains flexible and mobile. Therefore, the immobility of the hip joint should be carefully noted during the clinical examination as a key indicator of an irreducible dislocation. On the plain radiograph, a characteristic feature of irreducible dislocation is the abnormal apposition of the dislocated proximal femoral head fragment against the lateral aspect of the ilium in the supraacetabular region – a finding not typically seen in reducible hip dislocation. The radiographic findings described above were also present in the current case but were initially missed by the primary treating surgeon. This oversight led to an iatrogenic femoral neck fracture during the attempted reduction maneuver, converting the fracture pattern from type I to type III according to Pipkin classification. AVN of the femoral head is one of the most serious complications following femoral head and neck fractures, with an incidence of approximately 11.8% [2]. Park et al. [3] reported five cases of iatrogenic femoral neck fractures in patients with irreducible hip fracture-dislocations, all of whom ultimately required THR. Similarly, Scolaro et al. [7] managed 13 patients with Pipkin type III fractures initially treated with osteosynthesis, all of whom eventually required THR. Wang et al. [16], in their retrospective study of 12 patients, concluded that achieving good functional outcomes with open reduction and internal fixation (ORIF) for Pipkin type III femoral head fractures is challenging. Therefore, primary total hip arthroplasty may be considered an alternative. However, in younger patients, due to concerns about the long-term survivorship of prosthetic implants, ORIF may be recommended. There is no clearly defined age in the literature at which primary arthroplasty is recommended for Pipkin type III fractures. While many authors advocate for arthroplasty over fixation in femoral neck fractures in patients over 60 years of age, the optimal approach remains controversial in the 45–59 age group, particularly for displaced fractures [8,17,18,19]. In the present case, the patient’s age was at the borderline for considering arthroplasty. However, given her good bone quality and active mobility before injury, both treatment options—osteosynthesis and arthroplasty—were discussed in detail, outlining the advantages and disadvantages of each. The patient expressed a preference for attempting fracture fixation to preserve the native femoral head. Accordingly, the decision was made to proceed with open reduction and internal fixation. We recommend considering biological age rather than chronological age for the surgical management of fractures around the hip [9]. Due to the rarity of Pipkin type III fracture-dislocations, only a few surgical approaches have been documented, including the Kocher–Langenbeck, Smith–Petersen, and modified Gibson approaches [4,5,13]. In this case, we utilized a modified Gibson approach combined with a Ganz et al. trochanteric osteotomy to achieve better visualization of the femoral head and neck while preserving the femoral head’s blood supply [14]. Only two studies [5,20] have reported good functional outcomes with osteosynthesis in cases of femoral head fracture-dislocation complicated by iatrogenic femoral neck fractures, though these were limited to younger patients. To the best of our knowledge, we are the first to report a good functional outcome following osteosynthesis in an elderly patient with femoral head fracture-dislocation and an iatrogenic femoral neck fracture. However, this is a single case, and larger studies are needed to clearly establish age-related criteria for choosing between osteosynthesis and primary arthroplasty in such cases. In summary, irreducible femoral head fracture-dislocations, while uncommon, pose considerable diagnostic and treatment difficulties. Prompt identification is vital to prevent iatrogenic issues such as femoral neck fractures, which can significantly change the fracture configuration and treatment approach. Although existing literature suggests a shift toward arthroplasty for older individuals, our case illustrates the necessity of personalized treatment strategies, considering not only chronological age but also biological factors such as bone condition, functional status before injury, and patient preferences [10]. The favorable result in this instance, despite the complexities of a Pipkin type III fracture-dislocation complicated by an iatrogenic femoral neck fracture, implies that open reduction and internal fixation could still be a feasible option for carefully selected older patients. Nevertheless, due to the limited available data and the distinct characteristics of each case, more extensive multicentric research is required to formulate clearer management guidelines for these intricate injuries, especially concerning the comparison between primary arthroplasty and osteosynthesis across various age groups [11,12].
This case illustrates that head-preserving osteosynthesis is a viable and effective option in elderly patients with Pipkin type III fracture-dislocation, even when complicated by an iatrogenic femoral neck fracture. Early recognition of irreducible dislocations is crucial to avoid iatrogenic injury. While arthroplasty is often considered standard in older adults, this case supports personalized treatment decisions based on biological rather than chronological age. With appropriate surgical technique and careful patient selection, excellent functional outcomes can be achieved. Larger, multicenter studies are needed to refine treatment algorithms for this rare and complex injury pattern.
First, being a single case, the findings cannot be generalized to all elderly patients with Pipkin type III fracture-dislocations complicated by iatrogenic femoral neck fractures. Second, the follow-up period, although adequate at 18 months, may not fully capture long-term complications such as late-onset avascular necrosis or post-traumatic arthritis. Third, the choice of osteosynthesis over arthroplasty was influenced by patient preference and good bone quality, which may not be applicable in patients with poor bone stock or multiple comorbidities. Finally, due to the rarity of this injury pattern, direct comparisons with larger cohorts or standardized treatment protocols are lacking, limiting the ability to draw definitive conclusions.
References
- 1. Roeder LF Jr., DeLee JC. Femoral head fractures associated with posterior hip dislocation. Clin Orthop Relat Res 1980;147:121-30. [Google Scholar] [PubMed]
- 2. Giannoudis PV, Kontakis G, Christoforakis Z, Akula M, Tosounidis T, Koutras C. Management, complications and clinical results of femoral head fractures. Injury 2009;40:1245-51. [Google Scholar] [PubMed]
- 3. Park KH, Kim JW, Oh CW, Kyung HS, Park IH. A treatment strategy to avoid iatrogenic Pipkin type III femoral head fracture-dislocations. Arch Orthop Trauma Surg 2016;136:1107-13. [Google Scholar] [PubMed]
- 4. Mehta S, Routt ML Jr. Irreducible fracture-dislocations of the femoral head without posterior wall acetabular fractures. J Orthop Trauma 2008;22:686-92. [Google Scholar] [PubMed]
- 5. Alyousif H, Aleisawi H, Alkaff H, Albusayes N. Terrible triad of the hip: A case report. Int J Surg Case Rep 2021;82:105758. [Google Scholar] [PubMed]
- 6. Pipkin G. Treatment of grade IV fracture-dislocation of the hip. J Bone Joint Surg Am 1957;39:1027-42. [Google Scholar] [PubMed]
- 7. Scolaro JA, Marecek G, Firoozabadi R, Krieg JC, Routt ML Jr. Management and radiographic outcomes of femoral head fractures. J Orthop Traumatol 2017;18:235-41. [Google Scholar] [PubMed]
- 8. Aravind R, Upadhyay S, Aggarwal AK, Gupta T. Functional outcomes following osteosynthesis versus arthroplasty in femoral neck fractures in the middle-aged population. Indian J Orthop 2021;55:1154-60. [Google Scholar] [PubMed]
- 9. Babhulkar S, Pande K. Internal fixation of femoral neck fractures in the elderly: An Indian perspective. Injury 2005;36 (Suppl 1):S93-102. [Google Scholar] [PubMed]
- 10. Jain R, Basinski A, Kreder HJ. Nonoperative treatment of femoral neck fractures in elderly patients: A meta-analysis. Clin Orthop Relat Res 2002;399:45-51. [Google Scholar] [PubMed]
- 11. Zlowodzki M, Ayeni O, Petrisor BA, Bhandari M. Femoral neck shortening after fracture fixation with multiple cancellous screws: Incidence and effect on function. J Trauma 2008;65:372-7. [Google Scholar] [PubMed]
- 12. Swiontkowski MF. Management of femoral neck fractures in the elderly: Evidence-based surgical decisions. J Bone Joint Surg Am 2014;96:1324-5. [Google Scholar] [PubMed]
- 13. Moed BR. The modified Gibson posterior surgical approach to the acetabulum. J Orthop Trauma 2010;24:315-22. [Google Scholar] [PubMed]
- 14. Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 2001;83:1119-24. [Google Scholar] [PubMed]
- 15. Yue JJ, Wilber JH, Lipuma JP, Murthi A, Carter JR, Marcus RE, et al. Posterior hip dislocations: A cadaveric angiographic study. J Orthop Trauma 1996;10:447-54. [Google Scholar] [PubMed]
- 16. Wang S, Yu X, Li B, Ding Q, Wang T, Li Q, et al. Pipkin type III femoral head fracture: Which treatment strategy can be recommended? J Orthop Traumatol 2023;24:28. [Google Scholar] [PubMed]
- 17. Lowe JA, Crist BD, Bhandari M, Ferguson TA. Optimal treatment of femoral neck fractures according to patient’s physiologic age: An evidence-based review. Orthop Clin North Am 2010;41:157-66. [Google Scholar] [PubMed]
- 18. Dai Z, Li Y, Jiang D. Meta-analysis comparing arthroplasty with internal fixation for displaced femoral neck fracture in the elderly. J Surg Res 2011;165:68-74. [Google Scholar] [PubMed]
- 19. Wilson JM, Jones CA, Holmes JS, Farley KX, Hernandez-Irizarry RC, Moore TJ Jr., et al. Fixation vs arthroplasty for femoral neck fracture in patients aged 40-59 years: A propensity-score-matched analysis. Arthroplast Today 2022;14:175-82. [Google Scholar] [PubMed]
- 20. Snoap T, Freyder J, Roberts J. Management of a combined femoral head and neck fracture: A case report. JBJS Case Connect 2016;6:e88. [Google Scholar] [PubMed]











