Minimally Invasive Plate Osteosynthesis (MIPO) is a reliable and effective technique for treating proximal humeral fractures, providing high rates of fracture union and excellent functional outcomes when combined with timely intervention and structured rehabilitation.
Dr. Udit Agrawal, Department of Paediatric Orthopaedic, King George Medical University, Lucknow, Uttar Pradesh, India. E-mail: uditagrawal28@gmail.com
Introduction: Proximal humeral fractures are increasingly common due to both high-energy trauma in younger individuals and low-energy falls in the elderly. Surgical management is indicated for displaced and unstable fractures, with locking plates widely used. However, conventional open reduction techniques may compromise soft tissues and vascular supply. Minimally invasive plate osteosynthesis (MIPO) offers an alternative that preserves soft-tissue integrity while enabling stable fixation.
Objective: This study aimed to evaluate the clinical and radiological outcomes of proximal humeral fractures treated with MIPO.
Materials and Methods: This prospective study was conducted at Manipal Hospitals, Bengaluru, between August 2021 and May 2023. A total of 45 skeletally mature patients with proximal humerus fractures (classified according to Neer’s system) underwent MIPO. Patients were followed up for 6 months, and outcomes were assessed using the Constant–Murley score and radiographic parameters, including union time, head-shaft angle, and complications. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 25, with statistical significance set at P < 0.05.
Results: Among the 45 patients, 53% were male and 47% female, with a mean age of 54.38 years. The most common fracture type was Neer’s 3-part (64%). The average surgery duration was 40.5 min, and the mean blood loss was 114 mL. Fracture union was achieved in 96% of cases by 12 weeks, and the average Constant–Murley score was 77.2 ± 12.9. Functional outcomes were excellent or good in 78% of patients. Statistically significant associations were observed between outcomes and patient age (P = 0.00008) and comorbidities (P = 0.0002). The complication rate was 11%, including stiffness (7%), non-union (2%), and varus collapse (2%).
Discussion: The findings indicate that MIPO is an effective and reliable technique for treating proximal humeral fractures, offering favorable functional recovery and high union rates with minimal complications. Better outcomes were associated with younger age, fewer comorbidities, and timely surgical intervention. Compared to open techniques, MIPO reduced operative trauma and preserved the vascularity of fracture fragments.
Conclusion: MIPO provides promising clinical and radiographic outcomes in proximal humeral fractures, with a high rate of union and satisfactory functional recovery. It represents a safe and effective surgical option in appropriately selected patients, especially when combined with early rehabilitation and patient-specific care strategies.
Keywords: Proximal humerus fracture, minimally invasive plate osteosynthesis, radiological outcome, functional outcome, constant–Murley score.
The incidence of proximal humerus fractures is on the rise due to two main factors that reflect the bimodal distribution of these injuries [1]. First, the aging population is leading to an increase in low-energy injuries, especially among women over the age of 60 years who suffer from osteopenia [2]. Second, higher participation in sports and decreased mortality rates from traffic accidents are contributing to an increased occurrence of high-energy fractures that require medical treatment [3].
Due to the diverse range of anatomical and clinical circumstances, treatment options for proximal humeral fractures can vary greatly. Surgical intervention is generally advised for fractures that are displaced and/or unstable, aiming to restore proper anatomy and facilitate early rehabilitation of the shoulder [4]. Various procedures are available for fixing the fracture, with plating being the most frequently used method of osteosynthesis. The advent of locking plates has significantly enhanced clinical outcomes and broadened the indications for internal fixation [5]. Nevertheless, the rates of failure and complications still remain significant [3,6].
The deltopectoral approach for open reduction and internal fixation often necessitates significant soft tissue dissection and strong retraction of the deltoid muscle, particularly to achieve proper access to the greater tuberosity [4]. To mitigate these issues, a minimally invasive deltoid-splitting technique has been implemented for the plating of proximal humeral fractures.
This minimally invasive plate osteosynthesis (MIPO) method enhances visibility of the greater tuberosity while maintaining the integrity of the surrounding vascular structures and soft tissues, which ultimately supports improved bone healing conditions [7]. However, it does pose a higher risk of axillary nerve injury compared to the conventional deltopectoral approach [3].
Therefore, this study aims to evaluate the clinical and radiographic outcomes following MIPO plating for acute proximal humeral fractures.
This prospective study was conducted at the Manipal Hospitals, Bengaluru, from August 2021 to May 2023, following ethical approval from the Ethics Committee (MHB/01/220950/54). A total of 45 patients who met the established inclusion and exclusion criteria were enrolled in the study. The inclusion criteria consisted of patients aged over 18 years who presented within 3 weeks of sustaining an injury. The exclusion criteria encompassed patients with pathological fractures, open fractures, polytrauma, or neurovascular deficits. All fractures were classified according to Neer’s classification, and each patient underwent fracture fixation utilizing the MIPO technique, following informed consent and comprehensive preoperative evaluations. Intraoperative fluoroscopy was employed for both reduction and implant placement. Postoperatively, the limb was immobilized in an arm pouch, and mobilization commenced within the 1st week through pendulum exercises, based on the patient’s tolerance. Patients were discharged with an arm pouch and were instructed to continue pendulum exercises as well as shoulder muscle-strengthening activities. Active range of motion of the shoulder was initiated between 2 and 4 weeks postoperatively, contingent on the stability of the osteosynthesis. Movements of the elbow and hand were encouraged from the 1st day post-surgery. By the 4–6th week, immobilization was terminated, and active assisted movements were permitted up to 90° of abduction, avoiding forced external rotation. Full-range motion exercises began between the 6th and 8th weeks postoperatively. Clinical outcomes were evaluated at the final follow-up visit at 6 months by utilizing the Constant–Murley Score [8]. Shoulder stiffness was defined as a limitation in both active and passive motion in at least two directions, specifically forward flexion <120° or a 50% restriction of contralateral external rotation and internal rotation. Radiographic evaluations were conducted routinely at 2 weeks, 6 weeks, 12 weeks, and 24 weeks. These assessments aimed to evaluate fracture healing, alignment, and potential complications, including implant failure or malunion. Non-union was defined as the lack of progression in radiographic healing during the 3-month evaluation period. The neck-shaft angle was measured on anteroposterior radiographs at 20° of external rotation immediately after the operation and again at the final follow-up to ascertain the precise value. Varus collapse was identified as a reduction in the neck-shaft angle to <120° on follow-up radiographs. Malreduction was characterized by a neck-shaft angle of <120° on immediate postoperative radiographs. Operating time was defined as the interval from the initial skin incision to closure. The outcomes of this study were meticulously documented and analyzed using SPSS version 25.0 (SPSS Inc., Chicago, IL, USA). Descriptive evaluations were conducted based on means and standard errors, as well as percentages. Age, time interval to operation, operation duration, and Constant–Murley Score were expressed as median and range due to their rank-sum scale. The Kruskal–Wallis test was applied to compare non-normally distributed data among groups. The Mann–Whitney U test was used for parametric data, and Fisher’s exact test was employed for nonparametric pair comparisons to ascertain significant differences. A P < 0.05 was deemed statistically significant.
The patient was positioned in a beach chair at a 30° incline (Fig. 1A), and the surgical site was prepared under sterile protocols. Fractures were initially reduced using closed techniques and temporarily stabilized with K-wires before employing a minimally invasive approach for definitive fixation. Longitudinal traction was applied to the humeral shaft with the elbow flexed at 90° to correct displacements and angulations. The shoulder was adjusted internally and externally until the proximal and distal fragments aligned (Fig. 1B), maintained with a Kirschner wire. The greater tuberosity was reduced using a K-wire as a joystick (Fig. 1C), while significantly fewer tuberosity fragments were secured with a separate interfragmentary screw. Fixation was then performed using a locking plate and screws via the MIPPO technique (Fig. 1D-L).
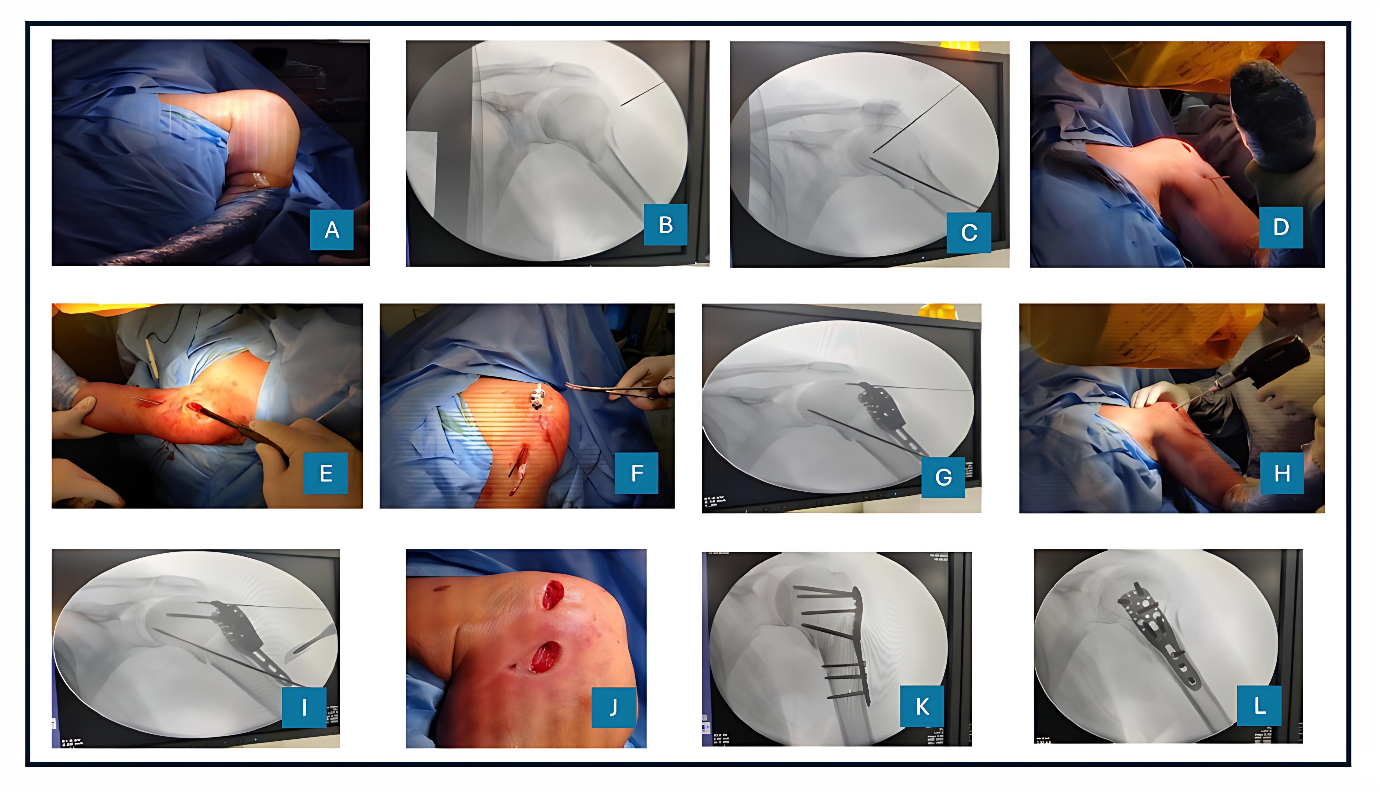
Figure 1: (A) Patient position – beach chair, (B) Fluoroscopy confirmation, (C) Temporary k wire fixation, (D) Proximal incision, (E) Sub-muscular tunnel using blunt dissection, (F) Plate insertion, (G) Plate position under fluoroscopy, (H) Proximal locking screw fixation, (I) Distal incision marking, (J) After both incision, (K) Final fluoroscopy image anteroposterior view, (L) Final fluoroscopy image lateral view.
This study encompasses a total of 45 consecutive cases of MIPO conducted over 18 months. Among the participants, 24 patients (53%) were male, and 21 patients (47%) were female, yielding a male-to-female ratio of 1.1:1. The patients were classified into three age groups: 10 patients (22%) were aged 18–35 years, 15 patients (33%) were aged 36–60 years, and 20 patients (45%) were over 60 years (Table 1).
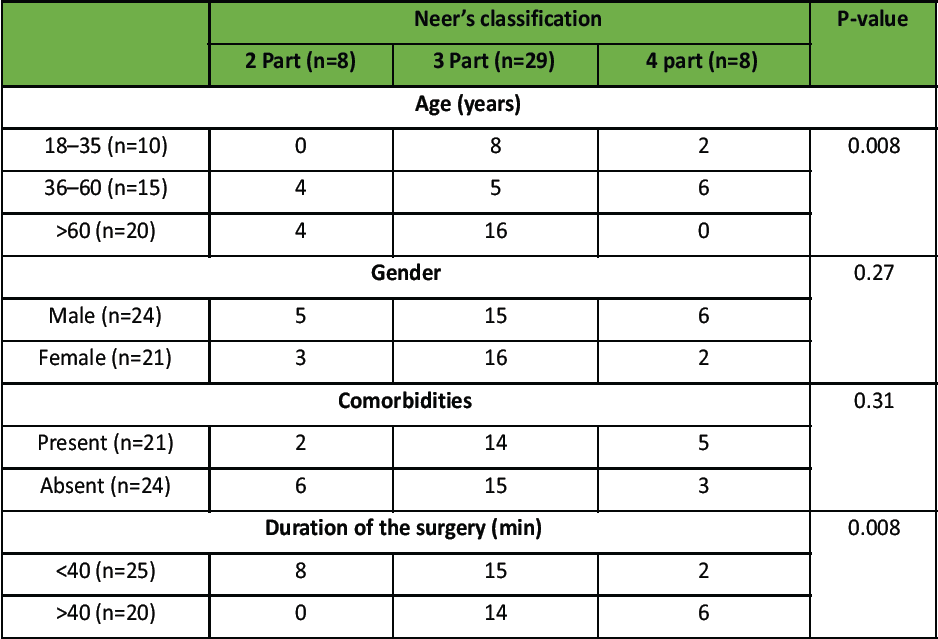
Table 1: Patient demographic details as per Neer’s classification
Following Neer’s classification, the fractures were categorized as follows: 8 patients (18%) presented with a 2-part fracture, 29 patients (64%) with a 3-part fracture, and 8 patients (18%) with a 4-part fracture, with the 3-part fracture representing the most prevalent type. Notably, 24 patients (53%) reported no comorbidities, whereas the remaining 21 patients (47%) exhibited single or multiple comorbidities, including diabetes, hypertension, ischemic heart disease, congestive heart failure, chronic renal disease, chronic obstructive pulmonary disease, chronic liver disease, and Parkinson’s disease (Table 1).
The association between comorbidities and Neer’s classification was observed; however, it did not reach statistical significance (P = 0.31). Conversely, the relationship between age and type of fracture was found to be significant (P = 0.008), while the correlation between gender and fracture type was not statistically significant (P = 0.27) (Table 1).
Furthermore, the duration of surgery was markedly influenced by patient-related factors such as comorbidities and fracture type. There was a significant correlation identified between the duration of surgery and the presence of comorbidities (P = 0.005), as well as between the duration of surgery and the type of fracture (P = 0.008) (Table 1).
The average blood loss observed in this study was quantified at 114 mL, as determined through mop soakage measurements. Among the 45 patients evaluated, 19 patients (42%) experienced blood loss within the range of 75–100 mL, while the remaining 26 patients (58%) exhibited blood loss between 125 and 150 mL. All patients underwent hospitalization for 3–7 days following the surgical procedure, after which they were discharged. Notably, 36 patients (80%) were hospitalized for 3–4 days, whereas 9 patients (20%) remained in the hospital for 5–7 days. The mean duration of hospitalization was calculated to be 3.8 days (Table 2).
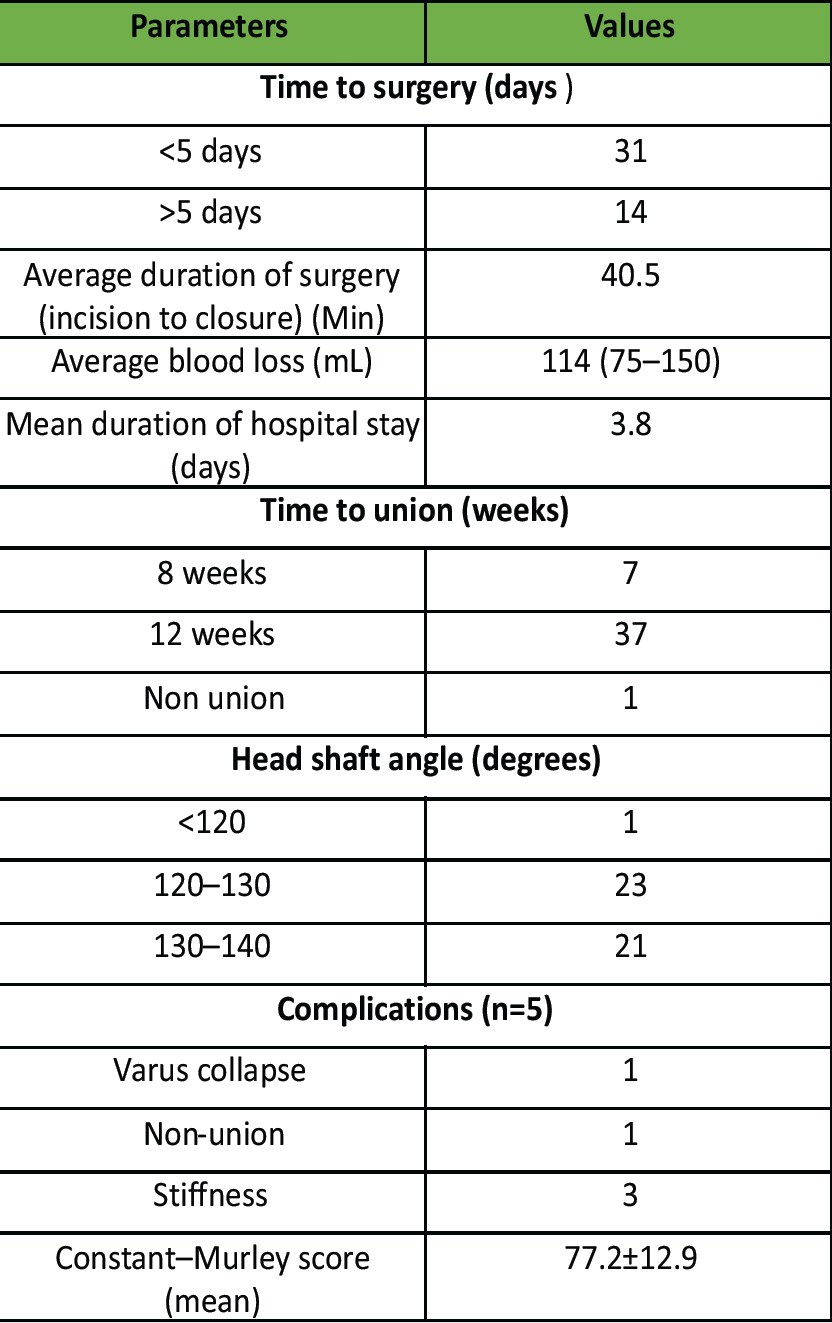
Table 2: Patient operative, radiographic ,and functional parameters
In terms of bone union, 7 patients (15.8%) achieved this outcome within 8 weeks, whereas 37 patients (82%) attained union at 12 weeks. Only 1 patient (2.2%) presented with non-union. The head-shaft angle varied between 120 and 140°: 23 patients (51%) had an angle ranging from 120 to 130°, 21 patients (47%) had an angle between 130 and 140°, and 1 patient (2.2%) had an angle of <120° (Table 2).
With respect to complications, 5 patients (11%) experienced adverse outcomes: 1 patient exhibited varus collapse (2%), 1 patient experienced non-union (2%), and 3 patients (7%) reported stiffness (Table 2).
A functional assessment was conducted utilizing the Constant–Murley score, with the outcomes classified as poor, fair, good, or excellent. Among the 45 patients evaluated, 3 (6.6%) exhibited a poor outcome, 7 (15.5%) demonstrated a fair outcome, 21 (46.6%) achieved a good outcome, and 14 (31%) attained an excellent outcome. The mean score recorded was 77.2 ± 12.9, indicating that the majority of patients exhibited good outcomes (Table 3).
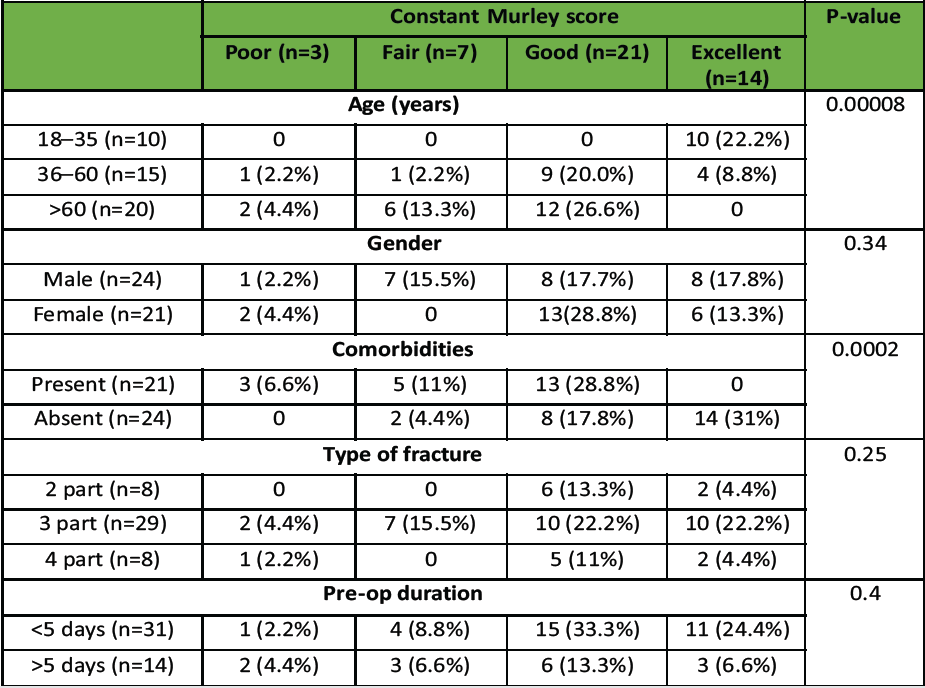
Table 3: Patient demographic details as per constant Murley score
Several factors were identified as being associated with the functional outcomes. The age of the patients demonstrated an inverse relationship with the outcomes, which was statistically significant (P = 0.00008). Conversely, the relationship between outcome and gender was not found to be significant (P = 0.34). The presence of comorbidities was significantly correlated with the outcomes (P = 0.0002). Although the type of fracture influenced the outcomes, this association was not statistically significant (P = 0.25). Furthermore, the duration between the occurrence of trauma and subsequent surgical intervention appeared to positively impact functional outcomes; however, this finding did not reach statistical significance (P = 0.4) (Table 3).
This prospective study was conducted at a tertiary care hospital and involved 45 patients diagnosed with proximal humerus fractures, all of whom underwent MIPO. Proximal humerus fractures are particularly prevalent among the elderly; in this study, 45% of the participants were aged 60 years or older. The mean age of the cohort was 54.38 ± 18.35 years, which is consistent with findings reported by Sohn and Shin [9] and Gonc et al. [10]. Among the study population, 53% were male, resulting in a male-to-female ratio of 1.1:1, which corroborates with earlier reports by Aggarwal et al. [11]. Participants included individuals with 2-part, 3-part, and 4-part fractures according to Neer’s classification, with 3-part fractures being the most prevalent at 64% which is consistent with findings reported by Alberio et al. [3] and Wang et al. [12]. A significant correlation (P = 0.008) was observed between age and fracture type, independent of gender and comorbidities. The interval from injury to surgery was <5 days for 69% of the patients, with a mean duration of 4 days. This timing aligns with findings articulated by Wang et al. [12]. The mean surgical duration was recorded at 40.5 min, consistent with durations reported by Gao et al. [13], while the average intraoperative blood loss was 114 mL, which is consistent with figures reported by Wang et al. [12]. Functional outcomes were assessed utilizing the Constant–Murley score, revealing that 78% of participants achieved good-to-excellent outcomes. Conversely, 15% attained fair outcomes, and 7% experienced poor outcomes. Significant associations were identified with age (P = 0.000002), comorbidities (P = 0.00027), and fracture type (P = 0.008). The mean Constant score was calculated at 77.2 ± 12.9, consistent with findings from Lin et al. [14], and Kim et al. [15]. Of the 45 cases analyzed, 43 patients achieved radiological fracture union within 12–14 weeks, constituting 96%. One patient experienced delayed union, while another case resulted in non-union due to a complex four-part fracture. These outcomes are in agreement with findings reported by Egol et al. [16], indicating that most patients attain union within 12 weeks. Notably, early fracture union correlated with more favorable functional outcomes. In this study, 98% of patients (44 individuals) demonstrated a head-shaft angle between 120 and 140° at the 6-month follow-up. Varus collapse was observed in one elderly patient with a three-part fracture, likely attributable to a preoperative head-shaft angle of <130°. This finding is consistent with the work of Gonc et al. [10], which correlated varus malunion with the use of guide sleeves that may have contributed to screw misalignment and compromised stability. The mean head-shaft angle in this study was determined to be 130°, corroborating findings from Kim et al. [15]. Notably, 89% of patients (40 out of 45) experienced no complications. However, three patients developed shoulder stiffness, leading to fair-to-poor outcomes, primarily due to insufficient compliance with rehabilitation protocols. The incidence of complications was 11%, which is lower than the rates reported by Wang et al. [12] and Falez et al. [17].
Strengths and limitations
The primary strength of this study lies in its prospective design, conducted at a tertiary care center with standardized surgical techniques, thereby minimizing procedural variability. The use of MIPO was systematically applied across all patients, and outcomes were objectively assessed using validated clinical (Constant–Murley Score) and radiological parameters. The inclusion of fracture classification, comorbidity assessment, and statistical correlation analysis provides a comprehensive understanding of factors influencing outcomes. Moreover, the study demonstrates a high rate of fracture union and low complication incidence, highlighting the efficacy of MIPO in the management of proximal humeral fractures. This study has several limitations. The relatively small sample size and single-center design restrict the generalizability of the findings and may introduce institutional biases. The absence of a control group precludes comparative analysis with other treatment modalities such as open reduction, conservative management, or intramedullary nailing. A short follow-up duration of 6 months may not capture long-term complications such as avascular necrosis, late implant failure, or post-traumatic arthritis. The use of only standard radiographs, without advanced imaging or biomechanical analysis, limits the depth of postoperative assessment. Rehabilitation compliance was not formally quantified, potentially affecting functional outcomes. Moreover, relying solely on the Constant–Murley score may not fully reflect overall upper limb function or quality of life. Finally, the lack of cost-effectiveness analysis limits conclusions regarding the broader applicability of MIPO, especially in resource-limited settings.
MIPO is a minimally invasive technique that offers excellent clinical and radiographic outcomes in the treatment of proximal humeral fractures. The procedure demonstrated high union rates, low complication incidence, and favorable functional recovery in the majority of patients. Patients who were younger, had fewer comorbidities, and underwent early surgical intervention achieved the best results. These findings highlight the effectiveness and safety of MIPO as a primary surgical option for appropriately selected proximal humeral fractures. Optimal outcomes depend on precise surgical technique, early mobilization, and adherence to rehabilitation protocols.
Minimally Invasive Plate Osteosynthesis enables stable fixation of proximal humeral fractures while preserving soft tissue and vascular integrity. Careful patient selection, meticulous surgical technique, and early mobilization are essential to achieve optimal clinical and radiographic outcomes.
References
- 1. Lind T, Krøner K, Jensen J. The epidemiology of fractures of the proximal humerus. Arch Orthop Trauma Surg 1989;108:285-7. [Google Scholar] [PubMed]
- 2. Bahrs C, Tanja S, Gunner B, Stig B, Badke A, Ulrich S, et al. Trends in epidemiology and patho-anatomical pattern of proximal humeral fractures. Int Orthop 2014;38:1697-704. [Google Scholar] [PubMed]
- 3. Alberio RL, Del Re M, Grassi FA. Minimally invasive plate osteosynthesis for proximal humerus fractures: A retrospective study describing principles and advantages of the technique. Adv Orthop 2018;2018:5904028. [Google Scholar] [PubMed]
- 4. Agrawal U, Vaibhav BK, Rao HK, Praseeth KR, Narayandas DK. Assessment of functional outcome and postoperative complications in proximal humerus fracture patients managed with proximal humerus internal locking system (PHILOS) plating. Cureus 2024;16:e63250. [Google Scholar] [PubMed]
- 5. Sproul RC, Iyengar JJ, Devcic Z, Feeley BT. A systematic review of locking plate fixation of proximal humerus fractures. Injury 2011;42:408-13. [Google Scholar] [PubMed]
- 6. Agudelo J, Schürmann M, Stahel P, Helwig P, Morgan SJ, Zechel W, et al. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma 2007;21:676-81. [Google Scholar] [PubMed]
- 7. Hepp P, Theopold J, Voigt C, Engel T, Josten C, Lill H. The surgical approach for locking plate osteosynthesis of displaced proximal humeral fractures influences the functional outcome. J Shoulder Elbow Surg 2008;17:21-8. [Google Scholar] [PubMed]
- 8. Vrotsou K, Ávila M, Machón M, Mateo-Abad M, Pardo Y, Garin O, et al. Constant-Murley Score: Systematic review and standardized evaluation in different shoulder pathologies. Qual Life Res 2018;27:2217-26. [Google Scholar] [PubMed]
- 9. Sohn HS, Shin SJ. Minimally invasive plate osteosynthesis for proximal humeral fractures: Clinical and radiologic outcomes according to fracture type. J Shoulder Elbow Surg 2014;23:1334-40. [Google Scholar] [PubMed]
- 10. Gönç U, Atabek M, Teker K, Tanrıöver A. Minimally invasive plate osteosynthesis with PHILOS plate for proximal humerus fractures. Acta Orthop Traumatol Turc 2017;51:17-22. [Google Scholar] [PubMed]
- 11. Aggarwal S, Bali K, Dhillon MS, Kumar V, Mootha AK. Displaced proximal humeral fractures: An Indian experience with locking plates. J Orthop Surg Res 2010;5:60. [Google Scholar] [PubMed]
- 12. Wang Y, Chen H, Wang L, Chen X, Zhi X, Cui J, et al. Comparison between osteosynthesis with interlocking nail and minimally invasive plating for proximal- and middle-thirds of humeral shaft fractures. Int Orthop 2021;45:2093-102. [Google Scholar] [PubMed]
- 13. Gao YB, Tong SL, Yu JH, Lu WJ. Case control study on open reduction internal fixation (ORIF) and minimally invasive percutaneous plate osteosynthesis (MIPPO) for the treatment of proximal humerus fractures in aged. Zhongguo Gu Shang 2015;28:335-9. [Google Scholar] [PubMed]
- 14. Lin T, Xiao B, Ma X, Fu D, Yang S. Minimally invasive plate osteosynthesis with a locking compression plate is superior to open reduction and internal fixation in the management of the proximal humerus fractures. BMC Musculoskelet Disord 2014;15:206. [Google Scholar] [PubMed]
- 15. Kim YG, Park KH, Kim JW, Oh JK, Yoon JP, Kim HJ, et al. Is minimally invasive plate osteosynthesis superior to open plating for fixation of two-part fracture of the proximal humerus? J Orthop Surg (Hong Kong) 2019;27:2309499019836156. [Google Scholar] [PubMed]
- 16. Egol KA, Ong CC, Walsh M, Jazrawi LM, Tejwani NC, Zuckerman JD. Early complications in proximal humerus fractures (OTA Types 11) treated with locked plates. J Orthop Trauma 2008;22:159-64. [Google Scholar] [PubMed]
- 17. Falez F, Papalia M, Greco A, Teti A, Favetti F, Panegrossi G, et al. Minimally invasive plate osteosynthesis in proximal humeral fractures: One-year results of a prospective multicenter study. Int Orthop 2016;40:579-85. [Google Scholar] [PubMed]