Clinical suspicion remains the key to diagnose necrotising fasciitis. Even though it is rare, necrotising fasciitis can arise from septic arthritis and life threatening consequences such as septic shock, organ failure and death can be prevented with prompt diagnosis and intervention.
Dr. Naveen Gupta, Department of Orthopaedics, Dr. Yashwant Singh Parmar Government Medical College and Hospital, Nahan, Himachal Pradesh, India. E-mail: drnaveenguptapgi@gmail.com
Introduction: Septic arthritis comprises pathological invasion of the joint space followed by inflammation. Predisposing risk factors include prior rheumatic joint disease, people at the extremes of age, such as young children and elderly people who have joint prostheses. Although generally bacterial, the etiology can also be viral or fungal. Staphylococcus and streptococcus are common bacteria that cause an acute septic arthritis. However, streptococcus has been emerged as the second most frequent causative agent for septic arthritis. According to a few case reports, septic arthritis of the joint may be found to be associated with necrotising fasciitis.
Case Report: A 10-year-old male child presented with a history of pain and swelling in the left arm and left shoulder from 3 to 4 days. His mother gave a history of a fall while playing 6 days back. Swelling was grossly increased on day 2 with erythema and induration over the whole of the left arm and shoulder. X-ray image showed soft-tissue swelling of the left arm. On Ultrasonography, a hypoechoic collection noted in the anterior compartment of the entire left arm just above the elbow joint.
Conclusion: This case highlights the importance of thorough assessment in primary care, which led to the high index of suspicion of septic arthritis and necrotising soft-tissue infection and timely management of the patient
Keywords: Septic arthritis necrotising fasciitis, broad-spectrum antibiotics, nonsteroidal anti-inflammatory drugs
Orthopaedic emergencies such as septic arthritis comprise pathological invasion of the joint space followed by inflammation. Predisposing risk factors include prior rheumatic joint disease, people at the extremes of age, such as young children and elderly people who have joint prostheses, Type 1 and Type 2 diabetes, prior intra-articular injection of steroids, and skin infections are typically present when it first manifests [1]. Although generally bacterial, the etiology can also be viral or fungal. Staphylococcus and Streptococcus are common bacteria that cause an acute septic arthritis in both adults and children. However, streptococcus has been emerged as the second most frequent causative agent for septic arthritis, and it is estimated that 13% of these were recognised as Group A Streptococcus (GAS) [2]. A few case reports suggest that septic arthritis of the joint may found to be associated with necrotising fascitis [3,4]. Necrotising soft-tissue infections typically have a polymicrobial etiology [4,5,6] and GAS is reportedly identified as one of the etiological factors for these infections [4].
A 10-year-old male child presented to the emergency department with a history of pain and swelling in the left arm and left shoulder from 3 to 4 days. His mother gave a history of fall while playing 6 days back. He was afebrile with a blood pressure of 96/64 mm of Hg and Pulse rate 88/min. On examination, there was a nontender swelling in the left arm with decreased range of motion in the left shoulder joint. Distal pulses were normal, and there was not any neurological deficit. On the basis of history and examination, a clinical diagnosis of soft-tissue injury of shoulder or possibility of physeal injury of proximal humerus was made. He was advised rest, and shoulder immobilizer was applied, and oral analgesics were given. The patient was admitted and kept for observation. On Day 2 of admission, swelling was grossly increased with erythema and induration over whole of the left arm and shoulder (Fig. 1). X-ray image showed soft-tissue swelling of the left arm (Fig. 2). On palpation, the overlying skin was warm, and the patient had temperature of 100.1℉; however, vital signs were normal. WBC count was 11.24 × 103, Hb was 10 g/dL, and C-reactive protein reactive = 6.

Figure 1: Clinical picture of child’s arm.
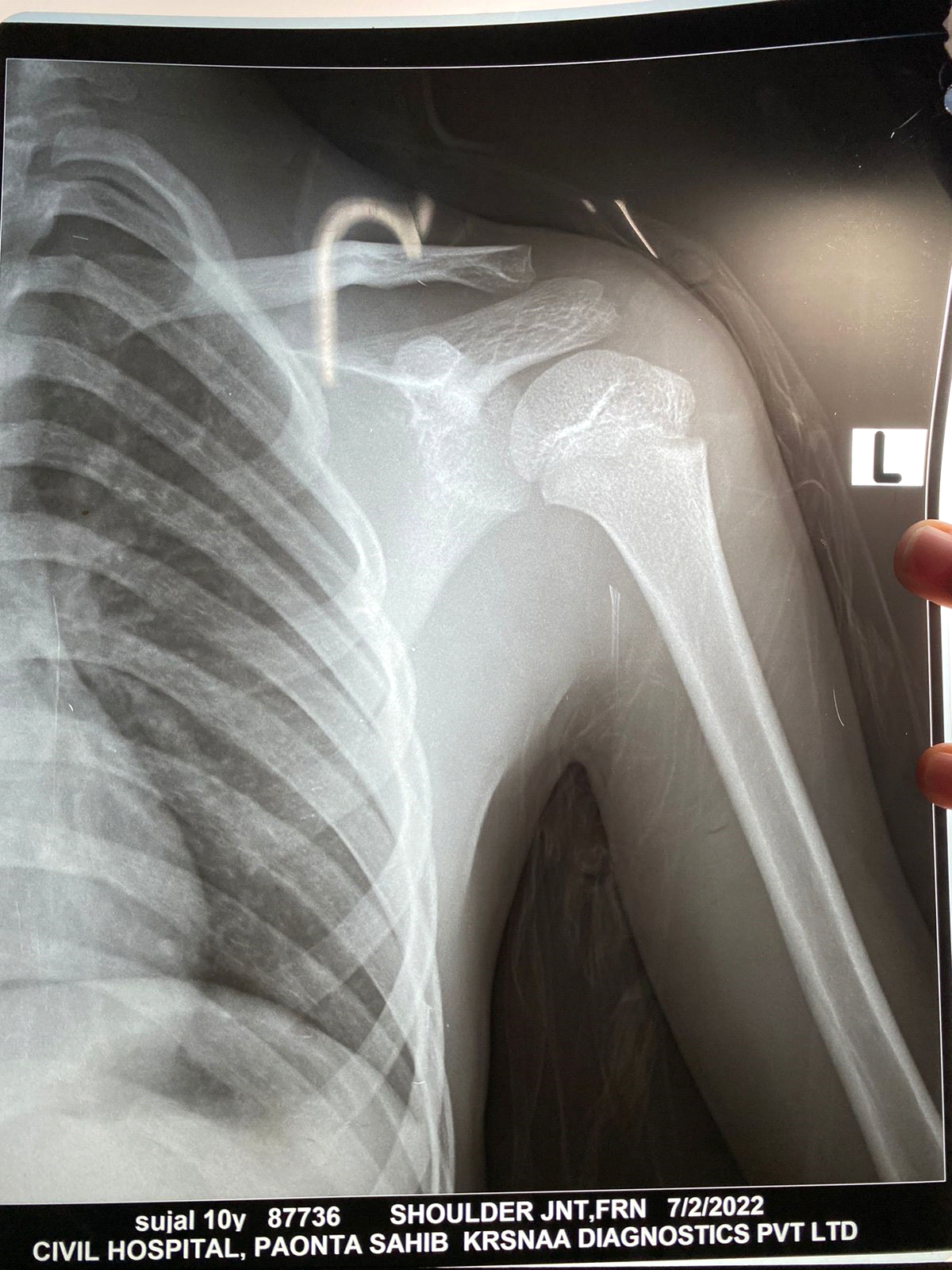
Figure 2: X-ray showing soft-tissue swelling of the left arm.
On Ultrasonography, a hypoechoic collection noted in the anterior compartment of the entire left arm just above the elbow joint. Collection was also seen in subdeltoid space and the left shoulder joint.
Management
About 10 cc of frank pus aspirated from the left shoulder joint and sent for culture and sensitivity. Arthrotomy was performed along with incision and drainage of pus from the whole of the anterior compartment of the left arm, done by deltopectoral approach. About 35 cc of pus was drained from the left arm and shoulder joint. On Gram stain, diplococci were seen. Sensitivity could not be established due to low colony count. Intraoperatively, necrosis of biceps and brachialis muscles was found in the superficial planes (Fig. 3). Postoperatively, broad-spectrum IV antibiotics (Ampoxin and Clindamycin) were given to the patient. He responded very well as swelling and erythema decreased slowly, and the process of wound healing took place on subsequent dressings. Patient was on IV antibiotics for three weeks and oral antibiotics for 3 weeks. Now wound is completely healed, and the child is doing well with physiotherapy. Biopsy report showed necrosis with inflammatory changes suggestive of necrotising inflammation.

Figure 3: Intraoperative picture showing necrotic fascia and subcutaneous tissue of the left arm.
Septic Arthritis is a type of inflammatory arthritis that can adversely affect people of any age group. According to review study with meta-analysis based on two prospective studies of patients with painful and swollen joints, the overall prevalence of septic arthritis was estimated to be 8–27% [7]. However, septic arthritis can be a diagnostic challenge, especially in the case of young children. The incidence rates are higher in children with age group of 0–4 years [8] and the most common affected joints are hip (32–39%) and knee (26–47%) whereas, other affected joints are ankle (9–18%), elbow (4–13%), shoulder (2–12%) and wrist (1–2%) [8,9,10,11,12,13]. Risk factors to develop necrotizing fasciitis are comparable to the risk factors to develop septic arthritis. However, a review study conducted by Wong et al., reported that only 13.5% patients were without any risk factors to develop necrotizing fasciitis [14]. In adults, numerous studies about necrotising fasciitis are available, but the literature studies related to paediatric patients are scarce. The most frequent site of involvement in children is abdominal wall, followed by thorax, back, scalp, and extremities. Though there is no gender variation, the incidence is slightly more in males [15]. In this case study, we presented a rare case of septic arthritis of the left shoulder joint associated with necrotizing fasciitis of the left arm in 10-year-old child. After presumptive diagnosis, immediately child was operated with arthrotomy of the left shoulder joint, along with incision and drainage of pus from the left arm was done. Thorough toileting and debridement of necrosed muscles and soft tissue were performed. Bilton et al., have reported in their study that timing and adequacy of early surgical debridement are the most crucial factor affecting mortality, as delayed or inadequate surgical debridement will result in rise in mortality [16]. Necrotising fasciitis is diagnosed histologically by the presence of necrosis of the superficial fascia and infiltration of leukocytes and polymorphonuclear cells in fascia, subcutaneous fat tissue, and dermis with the presence of bacteria in the dermis and fascia and absence of muscular damage [17]. These findings were similar to our case study in which fibrinoexudative material was reported on tissue biopsy with intact and degenerated neutrophils admixed with lymphocytes involving muscle and adipose tissue, in addition to it, necrotic debris was also seen suggesting necrotising inflammation. Predisposing factors for Necrotising fasciitis vary with age. Diabetes is the most common factor in adults [17]. However, other chronic diseases such as hypertension, peripheral vascular disease, renal failure, obesity, alcoholism, and malnutrition are important underlying factors [18]. Use of nonsteroidal anti-inflammatory drugs (NSAID) has been found as predisposing factor, although its association remains controversial. A few cases in children have been found with immunosuppressive diseases such as acute lymphoblastic leukemia. In our case, the patient had received NSAID for about 1 week (i.e., Tab Aceclofenac) on his initial visit to a physician. It has been shown that NSAIDS act as a contributory factor to worsen the severity of necrotising fasciitis [4]. The proposed theory behind it was that NSAID inhibits the chemotaxis phagocytosis, and bactericidal activity against Gram-positive cocci including GAS [4]. Hence, a detailed clinical assessment is essential to ensure that Necrotising fasciitis is excluded before NSAID is given.
Recognising a septic joint and necrotising soft-tissue infection can be a challenging task for Primary health care providers at the frontline, especially in patients without any documented risk factors. This case highlights the importance of thorough assessment in primary care, which led to the high index of suspicion of septic arthritis and necrotising soft-tissue infection and timely management of the patient, as early diagnosis and timely intervention are crucial in such cases.
Childhood necrotising fasciitis has far lower incidence and case fatality rates than adult cases. However, in more than half of the pooled instances, necrotising fasciitis appears to pose a relevant risk of morbidity as evidenced by skin grafting. To further elucidate necrotising fasciitis in childhood, a systematic multi-institutional research study is required to obtain significant results from future investigations.
References
- 1. García-Arias M, Balsa A, Mola EM. Septic arthritis. Best Pract Res Clin Rheumatol 2011;25:407-21. [Google Scholar] [PubMed]
- 2. Dubost JJ, Soubrier M, De Champs C, Ristori JM, Sauvezie B. Streptococcal septic arthritis in adults. A study of 55 cases with a literature review. Joint Bone Spine 2004;71:303-11. [Google Scholar] [PubMed]
- 3. Siva C, Velazquez C, Mody A, Brasington R. Diagnosing acute monoarthritis in adults: A practical approach for the family physician. Am Fam Physician 2003;68:83-90. [Google Scholar] [PubMed]
- 4. Leitch HA, Palepu A, Fernandes CM. Necrotizing fasciitis secondary to group a streptococcus. Morbidity and mortality still high. Can Fam Physician 2000;46:1480-6. [Google Scholar] [PubMed]
- 5. Davoudian P, Flint NJ. Necrotizing fasciitis. Crit Care Pain 2012;12:245-50. [Google Scholar] [PubMed]
- 6. Misiakos EP, Bagias G, Patapis P, Sotiropoulos D, Kanavidis P, Machairas A. Current concepts in the management of necrotizing fasciitis. Front Surg 2014;1:36. [Google Scholar] [PubMed]
- 7. Margaretten ME, Kohlwes J, Moore D, Bent S. Does this adult patient have septic arthritis? J Am Med Assoc 2007;297:1478-88. [Google Scholar] [PubMed]
- 8. Okubo Y, Nochioka K, Marcia T. Nationwide survey of pediatric septic arthritis in the United States. J Orthop 2017;14:342-6. [Google Scholar] [PubMed]
- 9. Peltola H, Pääkkönen M, Kallio P, Kallio MJ, Osteomyelitis-Septic Arthritis (OM-SA) Study Group. Prospective, randomized trial of 10 days versus 30 days of antimicrobial treatment, including a short-term course of parenteral therapy, for childhood septic arthritis. Clin Infect Dis 2009;48:1201-10. [Google Scholar] [PubMed]
- 10. Speiser JC, Moore TL, Osborn TG, Weiss TD, Zuckner J. Changing trends in pediatric septic arthritis. Semin Arthritis Rheum 1985;15:132-8. [Google Scholar] [PubMed]
- 11. Cole WG, Elliott BG, Jensen F. The management of septic arthritis in childhood. Aust N Z J Surg 1975;45:178-82. [Google Scholar] [PubMed]
- 12. Griffet J, Oborocianu I, Rubio A, Leroux J, Lauron J, Hayek T. Percutaneous aspiration irrigation drainage technique in the management of septic arthritis in children. J Trauma 2011;70:377-83. [Google Scholar] [PubMed]
- 13. Wiley JJ, Fraser GA. Septic arthritis in childhood. Can J Surg 1979;22:326-30. [Google Scholar] [PubMed]
- 14. Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL, Low CO. Necrotizing fasciitis: Clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am 2003;85:1454-60. [Google Scholar] [PubMed]
- 15. Hsieh WS, Yang PH, Chao HC, Lai JY. Neonatal necrotizing fasciitis: A report of three cases and review of the literature. Paediatrics 1999;103:e53. [Google Scholar] [PubMed]
- 16. Bilton BB, Zibarui GB, McMillan RW, Aultman DF, Dunn G, McDonald JC. Aggressive surgical management of necrotizing fasciitis serves to decrease mortality: A retrospective study. Am Surg 1998;64:397-401. [Google Scholar] [PubMed]
- 17. Oh C, Lee C, Jacobson JH 2nd. Necrotizing fasciitis of the perineum. Surgery 1982;91:49-51. [Google Scholar] [PubMed]
- 18. Sudarsky L, Laschinger JC, Coppa GF, Spencer FC. Improved results from a standardized approach in treating patients with necrotizing fasciitis. Ann Surg 1987;206:661-5. [Google Scholar] [PubMed]










