Spinal osteochondroma, though an uncommon entity, should be considered in the differential diagnosis of chronic lumbar pain and swelling in young patients, as it can lead to pain, cosmetic deformity, fractures, or neurological complications, with surgical excision being the definitive treatment to alleviate symptoms, prevent recurrence, and mitigate the risk of malignant transformation.
Dr. Vishal Sharma, Department of Orthopaedics, Christian Medical College and Hospital, Ludhiana, Punjab, India. E-mail: vishal4145@hotmail.com
Introduction: Osteochondroma is a common benign bone tumor, but its occurrence in the spine is rare, particularly in the lumbar region. Among spinal osteochondromas, involvement of the pedicle is uncommon. This case highlights a rare presentation of a pedunculated exostosis arising from the right pedicle of the first lumbar vertebra (L1) with a fracture at its base, leading to persistent lumbar pain and swelling. Given its potential for neurological compromise and malignant transformation, timely recognition and surgical intervention are crucial.
Case Report: A 19-year-old male presented with a progressively painful swelling in the lumbar region for 5 years. He had no history of trauma or systemic illness. Examination revealed tenderness over the right paraspinal area of the upper lumbar region with a palpable bony mass. Magnetic resonance imaging showed a pedunculated bony lesion arising from the right pedicle of L1, projecting postero-superiorly, with a fracture at its base. The patient underwent surgical excision through a posterior approach. Histopathology confirmed the diagnosis of osteochondroma. Postoperatively, the patient experienced significant symptom relief, with no recurrence on regular follow-ups.
Conclusion: This case underscores the importance of considering spinal osteochondroma in young patients with chronic lumbar pain and swelling. Although rare, spinal osteochondromas can lead to fractures, neurological compression, and potential malignant transformation, surgical excision provides definitive treatment, relieving symptoms and preventing complications. Reporting such cases enhances awareness and guides timely diagnosis and management.
Keywords: Osteochondroma, fracture, spine, pedicle, exostosis.
Osteochondroma (osseocartilaginous exostosis) is the most common benign bone tumor. Considered more like a hamartoma than a tumor, it accounts for 45% of benign bone tumors and 12% of all bone tumors [1]. Most often found in long bones, reports suggest osteochondroma of the spine to be relatively rare, accounting for only 4% to 7% of primary benign spinal tumors and <3% of all osteochondromas [2]. Spinal osteochondromas are classified into two types: Multiple osteochondromas or multiple hereditary exostosis and solitary osteochondroma or solitary exostosis [3]. Spine involvement usually requires advanced imaging for diagnosis like magnetic resonance imaging (MRI) [4]. They are most commonly found in the posterior elements of the spine, and intra-spinal extension is uncommon [5]. When the tumor causes pain, cosmetic deformity and/or neurological complications or when the diagnosis is unclear, it should be excised surgically [6]. In this paper, we present a 19-year-old male with a pedunculated exostosis arising from the right pedicle of 1st lumbar vertebral body (L1) with a fracture at the base, as a rare cause of lumbar pain and swelling.
A 19-year-old male with no comorbidities presented with a progressive painful swelling in the lumbar region for 5 years with cosmetic complains as his primary concern. There were no recorded neurological and constitutional symptoms. Therefore, in spite of the above complaints, there was no limitation of daily activities. On examination, there was tenderness over the right paraspinal region in the upper lumbar area with a fixed palpable mass of size approximately 4 × 3.5 cm, hard in consistency and no pulsation. Skin over the mass was normal and the mass was separate from the skin. There was no restriction in flexion-extension and rotational trunk movements (Fig. 1a and b).
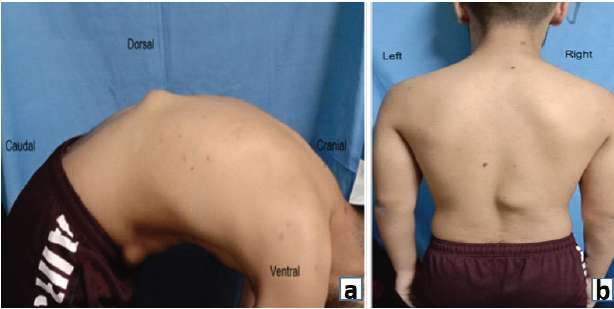
Figure 1: (a and b) Mass in the right paraspinal region in the upper lumbar area approximately 4 × 3.5 cm, hard in consistency and no pulsation. Skin over the mass was normal and the mass was separate from the skin.
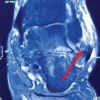
Neurological examination was normal. Computed tomography (CT) scan showed a pedunculated bony outgrowth arising from the right pedicle of L1 vertebral body projecting postero-superiorly, with a fracture at the base (Fig. 2a, b and c). MRI done also showed similar findings and an overlying cartilaginous cap of 2.3 mm thickness. The bony central spinal canal dimensions were normal with no evidence of primary canal stenosis (Fig. 3a and b). Under general anesthesia, an excision biopsy of the tumor mass was done through a posterior approach. Histopathological examination of the specimen as showed in Fig. 4. Postoperatively, the patient was symptomatically better, and on subsequent follow-ups did not show any recurrence or pain.
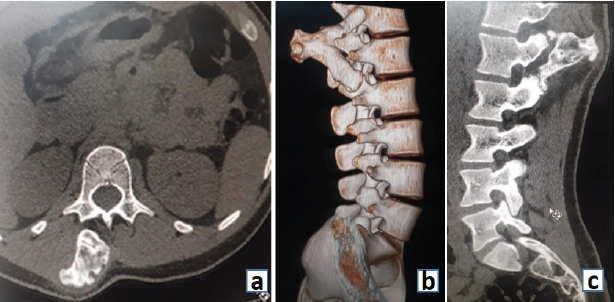
Figure 2: (a, b and c) Computed tomography scan images as described.

Figure 3: (a and b) Magnetic resonance images as described.
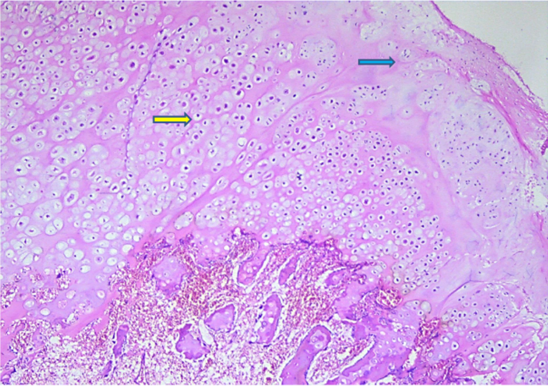
Figure 4: Microphotograph showing cartilaginous cap with fibrous perichondrium (blue arrow) and endochondral ossification (yellow arrow) (×40).
Osteochondromas are the most common benign bone tumors, accounting for 35–40% of such cases, typically affecting the appendicular skeleton and long bones, with spinal involvement being rare (3–4% in solitary cases, ~9% in hereditary multiple exostosis) [7,8]. The tumor affects mainly cervical and dorsal spine, possibly related to different durations of ossification that occur in secondary centers of ossification. It is speculated that more rapidly the ossification of these centers takes place, greater is the probability that aberrant cartilage will develop. In adolescence, secondary ossification centers which lie in the endplate of vertebral body, spinous process, transverse process, and articular process, complete the growth of vertebral column. These ossification centers appear in children between ages of 11 and 18 years. They develop into complete ossification in the cervical spine during adolescence and in the thoracic and lumbar spine at the end of second decade of life [9,10].
Osteochondromas have gender predilection and have been reported more in males (64%). Most common level of origin was 4th lumbar vertebra (38%). Most common anatomic site of origin was the inferior articular process (1/3rd) [11]. A review of English language literature has returned 44 cases of lumbar osteochondroma till 2015 including the article by Rymarczuk et al [12]. Cases reported in and after 2015 are illustrated in Table 1.
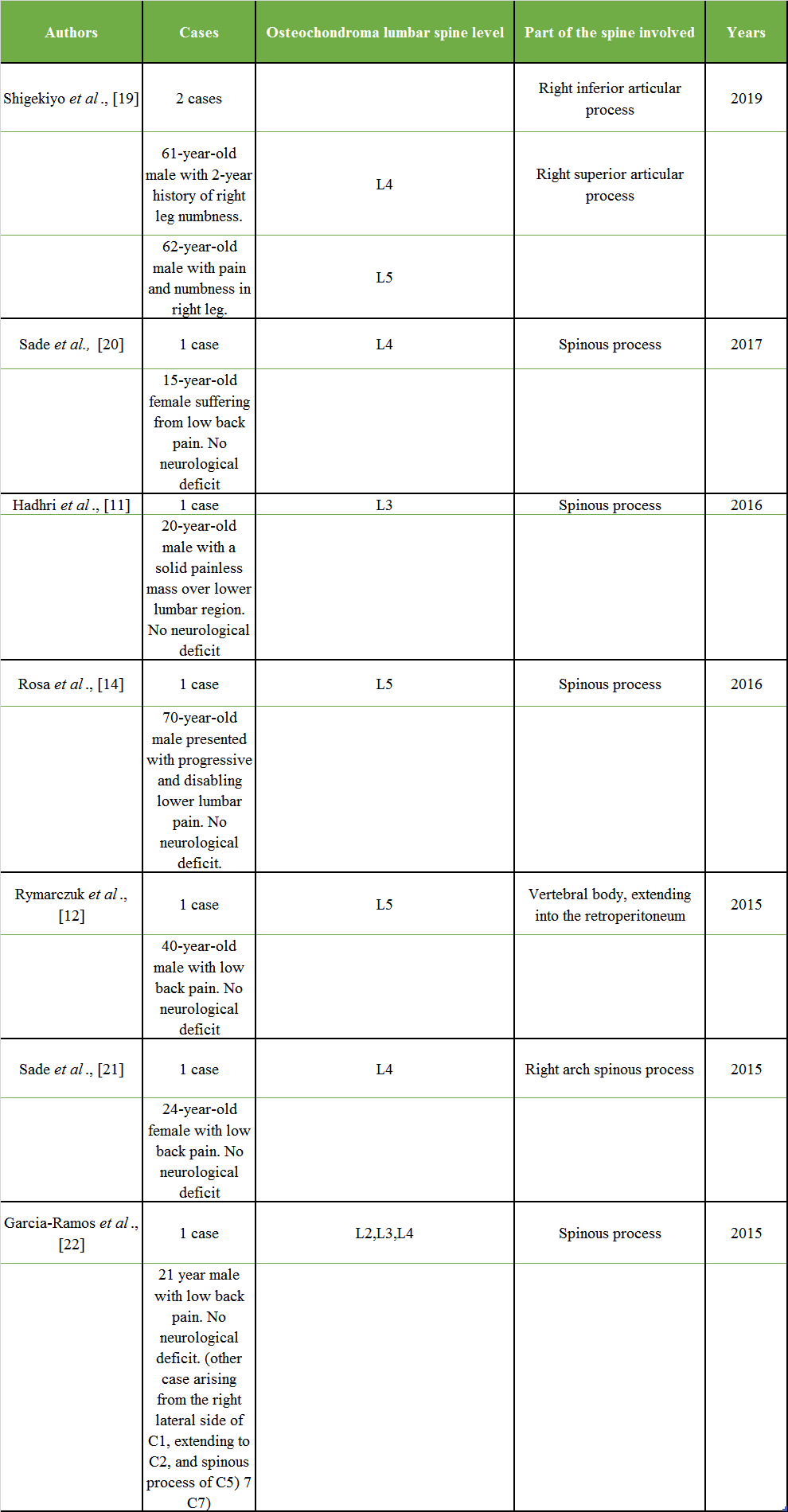
Table 1: Summary of reported cases of lumbar spine osteochondroma from 2015 onwards, including patient demographics, clinical presentation, affected vertebral level, specific part of the vertebra involved, and year of publication. This compilation highlights the anatomical variability and symptomatology associated with lumbar osteochondromas
Osteochondroma can cause pain by applying pressure on adjacent soft tissues when it grows posteriorly (with fracture also causing pain as well, as in our case). Asymptomatic lesions can be followed conservatively, but surgery can be considered whenever the diagnosis is not definite, or severe pain or in progressive neurological deficit [6], like foot-drop [13]. These lesions have both marrow and cortical continuity with the underlying bone and this is better seen on CT scan. MRI can be used to determine the extent of compromise of the underlying neurologic structures and to identify any suspicious malignant transformation [14,15]. Moreover, this is the most concerning complication of osteochondromas, fortunately a rare complication [16]. The most consistent finding that suggests malignant transformation may be a cap thickness >2 cm, but the diagnosis is only confirmed with a lesional biopsy [17]. Given the risk of malignant transformation, Gille et al., recommend surgical resection of all solitary spinal osteochondromas. In the majority of cases, the resection can be done without spinal instrumentation because it rarely compromises spinal stability, as osteochondromas show focal growth in posterior elements [18].
We report a rare case of lumbar osteochondroma arising from the right pedicle of L1 vertebral body with fracture at the base. Osteochondroma even though rarely involves the spine, most commonly involves the cervical and dorsal vertebrae with fewer cases in the lumbar spine. The patient was symptomatic due to fracture at the base of the tumor and pressure over the posterior structures. Diagnosis can be made using CT scan and MRI. Surgical resection and biopsy is the treatment of choice if the mass is symptomatic. Malignant transformation is the most dreaded complication but is rare.
Spinal osteochondroma, though rare, should be considered in young patients with chronic lumbar pain and swelling, as it can lead to fractures, neurological complications, or malignant transformation, with surgical excision being the definitive treatment for symptom relief and prevention of recurrence.
References
- 1. Patel A, Parry M, Vaiyapuri S, James SL, Botchu R, Jeys L. An unusual case of an intra-articular osteochondroma arising from the tibia: A case report. J Bone and Soft Tissue Tumors 2018;4:14-6. [Google Scholar] [PubMed]
- 2. Yakkanti R, Onyekwelu I, Carreon LY, Dimar JR. Solitary osteochondroma of the spine-a case series: Review of solitary osteochondroma with myelopathic symptoms. Glob Spine J 2018;8:323-39. [Google Scholar] [PubMed]
- 3. Fowler J, Takayanagi A, Fiani B, Cathel A, Sarhadi KJ, Arshad M, et al. Diagnosis, management, and treatment options: A cervical spine osteochondroma meta-analysis. World Neurosurg 2021;149:215-25.e6. [Google Scholar] [PubMed]
- 4. Jackson TJ, Shah AS, Arkader A. Is routine spine MRI necessary in skeletally immature patients with MHE? Identifying patients at risk for spinal osteochondromas. J Pediatr Orthop 2019;39:e147-52. [Google Scholar] [PubMed]
- 5. Raswan US, Bhat AR, Tanki H, Samoon N, Kirmani AR. A solitary osteochondroma of the cervical spine: A case report and review of literature. Childs Nerv Syst 2017;33:1019-22. [Google Scholar] [PubMed]
- 6. Lotfinia I, Vahedi A, Aeinfar K, Tubbs RS, Vahedi P. Cervical osteochondroma with neurological symptoms: Literature review and a case report. Spinal Cord Ser Cases 2017;3:16038. [Google Scholar] [PubMed]
- 7. Akhaddar A, Zyani M, Rharrassi I. Multiple hereditary exostoses with tetraparesis due to cervical spine osteochondroma. World Neurosurg 2018;116:247-8. [Google Scholar] [PubMed]
- 8. Qasem SA, Deyoung BR. Cartilage-forming tumors. Semin Diagn Pathol 2014;31:10-20. [Google Scholar] [PubMed]
- 9. Pawar E, Gavhale S, Bansal S, Dave H, Yadav AK, Akshay KS. Solitary osteochondroma of posterior elements of the spine: A rare case report. J Orthop Case Rep 2020;10:1-5. [Google Scholar] [PubMed]
- 10. Fiumara E, Scarabino T, Guglielmi G, Bisceglia M, D’Angelo V. Osteochondroma of the L-5 vertebra: A rare cause of sciatic pain. Case report. J Neurosurg 1999;91:219-22. [Google Scholar] [PubMed]
- 11. Hadhri K, Tebourbi A, Saidi M, Kooli M. Solitary osteochondroma arising in lumbar spinous process: Case report. Acta Orthop Traumatol Turc 2016;50:694-7. [Google Scholar] [PubMed]
- 12. Rymarczuk GN, Dirks MS, Whittaker DR, Neal CJ. Symptomatic lumbar osteochondroma treated via a multidisciplinary military surgical team: Case report and review of the literature. Mil Med 2015;180:e129-33. [Google Scholar] [PubMed]
- 13. Kahveci R, Ergungor MF, Gunaydin A, Sanli AM, Temiz A. Solitary lumbar osteochondroma presenting with foot-drop: A case report. Turk Neurosurg 2012;22:386-8. [Google Scholar] [PubMed]
- 14. Rosa B, Campos P, Barros A, Karmali S, Ussene E, Durão C, et al. Spinous process osteochondroma as a rare cause of lumbar pain. Case Rep Orthop 2016;2016:2683797. [Google Scholar] [PubMed]
- 15. Thiart M, Herbrst H. Lumbar osteochondroma causing spinal compression. SA Orthopaedic J Winter 2010;9:44-6. [Google Scholar] [PubMed]
- 16. Ruivo C, Hopper MA. Spinal chondrosarcoma arising from a solitary lumbar osteochondroma. JBR-BTR 2014;97:21-4. [Google Scholar] [PubMed]
- 17. Strovski E, Ali R, Graeb DA, Munk PL, Chang SD. Malignant degeneration of a lumbar osteochondroma into a chondrosarcoma which mimicked a large retropertioneal mass. Skeletal Radiol 2012;41:1319-22. [Google Scholar] [PubMed]
- 18. Gille O, Pointillart V, Vital JM. Course of spinal solitary osteochondromas. Spine (Phila Pa 1976) 2005;30:E13-9. [Google Scholar] [PubMed]
- 19. Shigekiyo S, Nishisho T, Takata Y, Toki S, Sugiura K, Ishihama Y, et al. Intracanalicular osteochondroma in the lumbar spine. NMC Case Rep J 2019;7:11-5. [Google Scholar] [PubMed]
- 20. Sade R, Ulusoy OL, Mutlu A, Yuce I, Kantarci M. Osteochondroma of the lumbar spine. Joint Bone Spine 2017;84:225. [Google Scholar] [PubMed]
- 21. Sade R, Yuce I, Karaca L, Ogul H, Kantarci M, Eren S. Lumbar osteochondroma presented with low back pain. Spine J 2015;15:e35. [Google Scholar] [PubMed]
- 22. Garcia-Ramos CL, Buganza-Tepole M, Obil-Chavarría CA, Reyes-Sánchez AA. Spinal osteochondroma: Diagnostic imaging and treatment. Case reports. Cir Cir 2015;83:496-500. [Google Scholar] [PubMed]