ACL reconstruction using an anterolateral tibial tunnel gives similar results to an anteromedial tunnel in ACL revision surgeries.
Dr. Prannoy Paul, Department of Orthopaedics, M.O.S.C Medical College Hospital, Kolenchery, Ernakulam, Kerala, India. E-mail: prannoypaul@gmail.com
Introduction: Multiple options are available for revising a failed anterior cruciate ligament (ACL) reconstruction. A staged procedure is considered only if there is significant tunnel widening. Here, we present a case of revision ACL reconstruction done in single sitting in spite of a widened tibial tunnel of 15.9 mm through an anterolateral tibial tunnel using a peroneus graft.
Case Report: A 39-year-old male manual laborer with post-polio residual paralysis in the opposite leg with past history of trans-portal ACL reconstruction 11 years back using an ipsilateral hamstring graft presented to us with complaints of instability and swelling of the left knee following a slip and fall 2 months back. Magnetic resonance imaging showed a tear in the reconstructed ACL graft with cyclops and tibial tunnel widening of 15.9 mm. The patient underwent single stage revision ACL reconstruction through the anterolateral tibial tunnel using a peroneus longus tendon autograft. At 1 year follow-up, the patient has good knee movements with no signs of instability.
Conclusion: Single stage revision ACL reconstruction through the anterolateral tibial tunnel in a case of significantly widened tibial tunnel gives satisfactory results similar to anteromedial tibial tunnel with advantages of not requiring a second surgery, faster recovery, and good bone for the tunnel compared to the previous medial tunnel.
Keywords: Anterior cruciate ligament reconstruction, revision anterior cruciate ligament, peroneus longus graft, anterolateral tibial tunnel.
Anterior cruciate ligament (ACL) injuries are common injuries seen in the younger population with more prevalence among the athletic population. ACL reconstruction using autograft or allograft has been shown to produce excellent functional stability with a predictable return to sports. The failure rate has been reported to around between 10 and 15% in short-term follow-ups and around 27% in long-term follow-ups [1]. ACL reconstruction failures can be attributed to several factors. It can be patient-related, surgeon-related, or biology-related [2]. Fresh trauma is the most frequent single ACL reconstruction failure accounting for up to 38%, followed by technical errors (22%) and biological failures (8%) [3]. Multiple revision ACL reconstruction options are available that can be performed in a single sitting or staged procedure. Literature shows a two stage revision when there is tibial tunnel widening of more than 15 mm.. A few other factors to be considered are patient and surgeon preference, associated cartilage and meniscal status, and limb alignment [4]. Regardless of prior tunnel placement and bone abnormalities, one cannot compromise on tunnel placement while revising a failed ACL graft. The tunnel should be made through good-quality bone. Here, we present a case of revision ACL reconstruction done through a tibial tunnel placed laterally to the tibial tuberosity.
A 39-year-old male manual laborer with post-polio residual paralysis in the right leg presented to us with complaints of instability and swelling of the left knee following a slip and fall 2 months back. The patient is a known case of type 2 diabetes mellitus on oral hypoglycaemic agents. The patient was initially treated in another center with analgesics and immobilization for a week. For the past 1 month, he has had complaints of instability while walking. The patient had a history of trans-portal ACL reconstruction done 11 years back using an ipsilateral hamstring graft treated at another centre. On clinical examination of the left knee, mild effusion was present. No bony tenderness was noted. Ligament laxity examination shows a Lachmann grade 3. No neurovascular deficits were recorded. A radiograph of the left knee showed no bony injuries or mal-alignment with the EndoButton over the lateral femoral condyle (Fig. 1a and b). Magnetic resonance imaging showed a lax torn reconstructed ACL with a widened tibial tunnel of 15.9 mm. No osteochondral defects were noted (Fig. 1c and d).

Figure 1: (a) Pre-operative anteroposterior view showing EndoButton over the lateral femoral condyle. (b) Pre-operative lateral view showing posteriorly placed EndoButton and anteriorly placed tibial tunnel, (c) pre-operative proton density fat-suppressed (PDFS) coronal image showing widened tibial tunnel, and (d) pre-operative PDFS coronal image showing widened and anteriorly placed tibial tunnel. Since the patient was diabetic and showed signs of effusion in the knee joint suggestive of synovitis, to rule out infection, aspiration of the left knee joint under sterile conditions was done along with blood counts. Results showed no signs of infection. Hence, the patient was taken up for arthroscopic revision ACL reconstruction with anterolateral tibial tunnel using peroneus longus graft. The patient was positioned in a supine position. An anterolateral viewing portal and an anteromedial instrument portal with an accessory anteromedial portal were made. Diagnostic arthroscopy was performed. The old femoral tunnel was found to be anterior, more vertical and in non-isometric position which was the cause for the failure. The medial meniscus and lateral meniscus were found to be normal. Peroneus longus tendon graft harvested from the ipsilateral ankle. The graft was quadrupled and found to be 8.5 mm in diameter. Transportal drilling of femoral tunnel done selecting the isometric point keeping the knee hyper-flexed. This resulted in a very separate tunnel maintaining a bone bridge between the old and new femoral tunnel. The tunnel length was 40 mm, 4 mm reamer reamed throughout and over-reamed with 8.5 mm reamer to 30 mm.
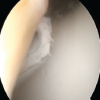
The previous tibial tunnel was assessed and it was found to be expanded and anteriorly placed. To avoid a staged procedure, an anterolateral tibial tunnel was created. Tunnel length was 50 mm and reamed with 9 mm reamer. Graft passed through tunnels (Fig. 2a, b, c, d), and the EndoButton was flipped, which was later ensured using fluoroscopy. The knee was cycled and an interference screw of size 30 × 9 mm (Titanium) was inserted with negative Lachman and internal rotation. The graft was checked to have adequate tension and the button flip was confirmed under the fluoroscopy again.
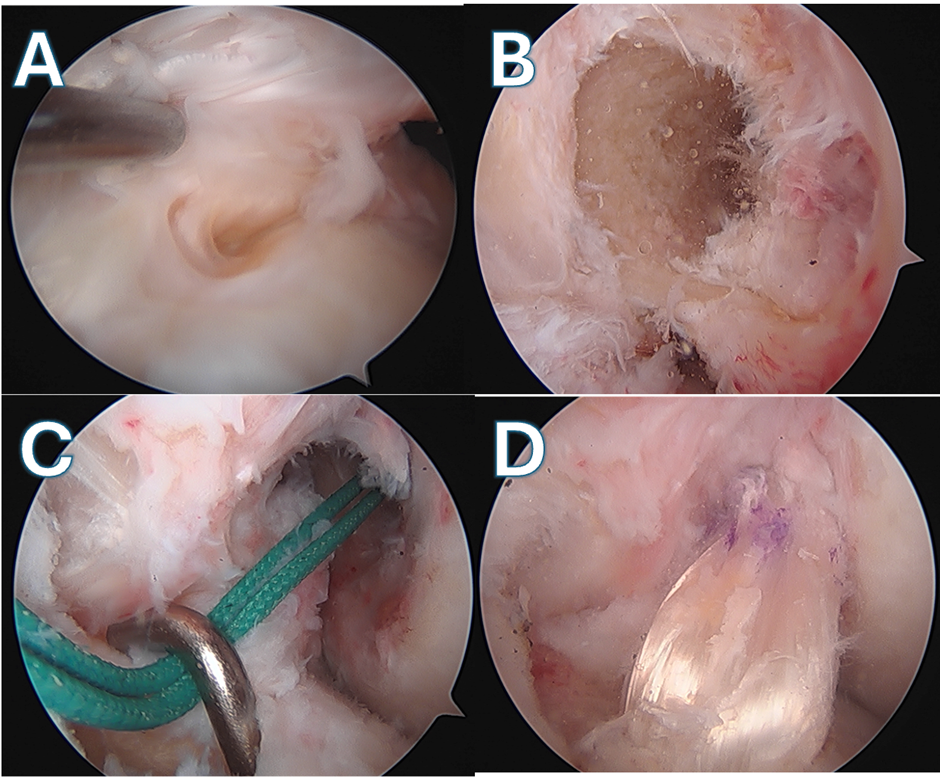
Figure 2: Arthroscopic images showing, (a) lax anterior cruciate ligament, (b) old and the new femoral tunnel, (c) new tibial tunnel from the anterolateral aspect, and (d) peroneus graft seated in the anterolateral and femoral tunnel.
Postoperatively, he was placed in a long knee brace and post-operative rehabilitation started from post-operative day 1 according to ACL reconstruction protocol. The patient was followed up at 6 weeks (Fig. 3), 3 months, 6 months, and then yearly for assessment of pain, ligament laxity, and functional scores. The patient was allowed for sporting activities after 9 months. Two years post-surgery, the patient had no limitation of activities with no ligament laxity. After 2 years, clinical scores were assessed with the tegner activity level scale and modified cincinnati score improving from pre-operative average of 39 and 37 to post-operative average of 90 and 88 (Fig. 4).
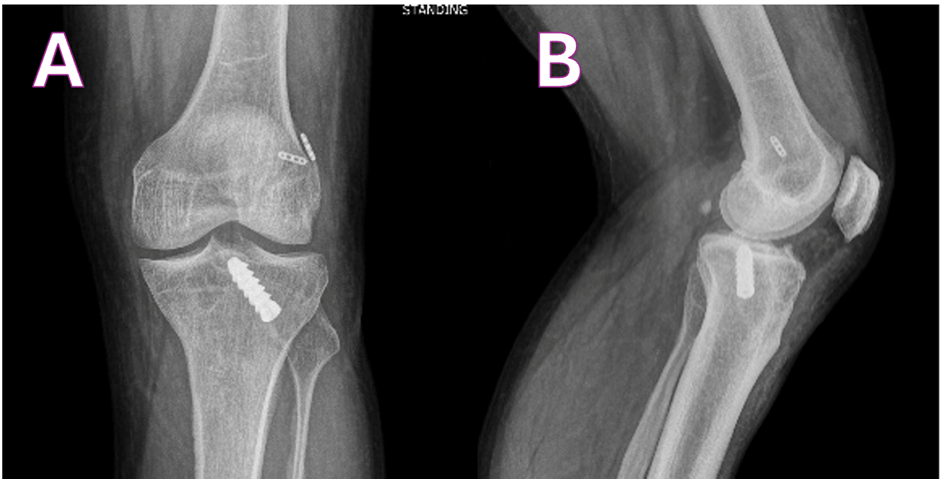
Figure 3: Post-operative X-ray at 6 weeks (a) post-operative anteroposterior view showing BioScrew placed from the anterolateral aspect and (b) post-operative lateral view showing well seated EndoButton and BioScrew.

Figure 4: (a and b) Post-operative range of movement.
Revision ACL reconstructions are typically more challenging due to old tunnels created in the index surgery, graft-holding implants used in the index case, and the increased number of associated injuries [5]. The indication for a single-stage revision depends on the index surgery’s bone tunnel position and size that positions for a good aperture fixation of the graft, while the indications of two-stage revision are specific in that index surgery tunnel expansion and the revision surgery tunnel should not coalesce [6]. Two stage revision poses significant problems in terms of cost, morbidity and the recovery time compared to a single stage revision. Long-term data suggest no significant difference in single versus staged revision, unless it is a complex case.
Widened bone tunnel of the index surgery is a major problem encountered in the revision scenarios. This affects the revision surgery in terms of inferior bone to graft incorporation and an inadequate strength of graft fixation [7]. Therefore, it is crucial to have a graft placed in anatomical position with the tunnel in a good quality bone. Some of the techniques that are accepted to direct the tunnel related problems in a single sitting revision scenario are the funnel technique [8], stacking screw technique [9], instant bone allograft technique, and dilatation technique [10].
One of the novel techniques described in the literature is the use of an anterolateral tibial tunnel. The indication for the use of a lateral tibial tunnel is a dilated tunnel of more than 15 mm that too specifically in the middle and the distal portion. The anterolateral tibial tunnel prevents the possibility of a proximal tibial fracture near the previous tunnel site and offers a strong bone for fixation of the graft [11]. The anterolateral tibial offers several advantages not requiring a second surgery, faster recovery in terms of early return to sports and work, and good bone for the tunnel compared to the previous medial tunnel with bone graft inside it. The drawback of a anterolateral tibial tunnel is the acute turn the graft needs to go through from tibia to femur tunnel causing graft abrasion similar to posterior cruciate ligament reconstruction.
Recently, a biomechanical study by Van Der Bracht et al., concluded that anterolateral tibial tunnel is a good alternative to overcome problems related to tunnel enlargement in the distal part of the tibial tunnel [12]. In this case, since the patient was a manual laborer who required to be back at work as early as possible, with a tibial tunnel width of more than 15 mm as evident on magnetic resonance imaging, he was taken up for single-stage ACL reconstruction using an anterolateral tibial tunnel. At 1-year follow-up, the patient has good knee movements with no signs of instability.
Single stage revision ACL reconstruction through the anterolateral tibial tunnel in a case of significantly widened tibial tunnel gives satisfactory results similar to anteromedial tibial tunnel with advantages of not requiring a second surgery, faster recovery, and good bone for the tunnel compared to the previous medial tunnel.
In ACL revision surgeries, an anterolateral tibial tunnel can give equally good results to that of an anteromedial tibial tunnel.
References
- 1. Crawford SN, Waterman BR, Lubowitz JH. Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy 2013;29:1566-71. [Google Scholar] [PubMed]
- 2. Tapasvi S, Shekhar A. Revision ACL reconstruction: Principles and practice. Indian J Orthop 2021;55:263-75. [Google Scholar] [PubMed]
- 3. Vermeijden HD, Yang XA, Van Der List JP, DiFelice GS, Rademakers MV, Kerkhoffs GM. Trauma and femoral tunnel position are the most common failure modes of anterior cruciate ligament reconstruction: A systematic review. Knee Surg Sports Traumatol Arthrosc 2020;28:3666-75. [Google Scholar] [PubMed]
- 4. Colatruglio M, Flanigan DC, Long J, Dibartola AC, Magnussen RA. Outcomes of 1- versus 2-stage revision anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Am J Sports Med 2020;49:798-804. [Google Scholar] [PubMed]
- 5. Rahardja R, Zhu M, Love H, Clatworthy MG, Monk AP, Young SW. Factors associated with revision following anterior cruciate ligament reconstruction: A systematic review of registry data. Knee 2020;27:287-99. [Google Scholar] [PubMed]
- 6. Wright R, Spindler K, Huston L, Amendola A, Andrish J, Brophy R, et al. Revision ACL reconstruction outcomes: MOON cohort. J Knee Surg 2011;24:289-94. [Google Scholar] [PubMed]
- 7. De Beus A, Koch JE, Hirschmann A, Hirschmann MT. How to evaluate bone tunnel widening after ACL reconstruction – a critical review. Muscles Ligaments Tendons J 2017;7:230-9. [Google Scholar] [PubMed]
- 8. Buller LT, Best MJ, Baraga MG, Kaplan LD. Trends in anterior cruciate ligament reconstruction in the United States. Orthop J Sports Med 2014;3:2325967114563664. [Google Scholar] [PubMed]
- 9. Werner BC, Gilmore CJ, Hamann JC, Gaskin CM, Carroll JJ, Hart JM, et al. Revision anterior cruciate ligament reconstruction: Results of a single-stage approach using allograft dowel bone grafting for femoral defects. J Am Acad Orthop Surg 2016;24:581-7. [Google Scholar] [PubMed]
- 10. Kraeutler MJ, Welton KL, McCarty EC, Bravman JT. Revision anterior cruciate ligament reconstruction. J Bone Joint Surg Am 2017;99:1689-96. [Google Scholar] [PubMed]
- 11. Keyhani S, Hanafizadeh B, Verdonk R, Sajjadi MM, Soleymanha M. Revision single-stage anterior cruciate ligament reconstruction using an anterolateral tibial tunnel. J Knee Surg 2019;33:410-6. [Google Scholar] [PubMed]
- 12. Van Der Bracht H, Verhelst L, Goubau Y, Fieuws S, Verdonk P, Bellemans J. The lateral tibial tunnel in revision anterior cruciate ligament surgery: A biomechanical study of a new technique. Arthroscopy 2012;28:818-26. [Google Scholar] [PubMed]