Synovial sarcoma, particularly when intra-articular and small (<5 cm), can present with symptoms and imaging features similar to benign conditions such as ganglion cysts, venous malformations, or PVNS, making diagnosis challenging. Long-standing “Nodular synovitis/ Ganglion cyst” is not benign enough to be ignored. Prompt evaluation must be done radiologically before surgery to prevent unwarranted consequences. Multi-disciplinary approach helps in preventing recurrence and improves the long-term survival rate of the patient.
Dr. Akilesh Kumar, Department of Orthopeadics, MIOT International Hospital, Chennai, Tamil Nadu, India. E-mail: akhilesh2475@gmail.com
Introduction: An uncommon malignant soft-tissue tumor, synovial sarcoma (SS) usually develops close to large joints like the knee and ankle, and most frequently affects young adults. These tumors might be confused for benign intra-articular lesions such as pigmented villonodular synovitis, synovial osteochondromatosis, or ganglion cysts because they frequently manifest as slow-growing, painless masses. The diagnostic difficulties and significance of taking SS into account when making a differential diagnosis for chronic intra-articular lesions are highlighted by this case.
Case Report: A 25-year-old man from South India came in complaining of right knee pain and limited flexion that had gotten worse for 6 months. Physiotherapy has not alleviated his symptoms in the past. Although the quality of the initial imaging was poor, it showed a cystic lesion close to the lateral femoral condyle. A clinical examination revealed a limited range of motion (0–100°), point discomfort over the lateral femoral condyle, and no indications of joint instability or effusion. Arthroscopic excision of the lesion was done, followed by Radio and Chemotherapy. According to MRI and PET CT, the patient was still disease-free and had good knee function 14 months after surgery. A Yearly follow-up was recommended for him due to the possibility of a late relapse.
Conclusion: Prompt diagnosis and the best possible care depend on early surgical intervention and comprehensive histological assessment. To prevent treatment delays and enhance patient outcomes, clinicians should take SS consideration when establishing a differential diagnosis for any persistent or unusual intra-articular mass, especially in young adults.
Keywords: Synovial sarcoma, biphasic synovial sarcoma, pigmented villonodular synovitis, ganglion cyst.
Synovial sarcomas (SSs) are uncommon malignancies predominantly seen in the younger population [1]. Less than 10% of soft-tissue sarcomas are SS, which are malignant mesenchymal spindle cell tumors with variable epithelial differentiation and unknown histogenesis. SS can be either monophasic or biphasic. However, intra-articular SS is quite uncommon [2,3]. These sarcomas usually appear as a slow-growing non-tender mass found more common in the extremities with male predominance and no ethnic variance in incidence [4]. Due to its slow growth and non-specific clinical and radiologic features, the diagnosis and treatment of intra-articular SS are often delayed [5,6,7]. While larger lesions tend to appear more heterogeneous on magnetic resonance imaging (MRI), smaller SS lesions (<5 cm) may present with well-demarcated margins and homogeneous signal intensity, mimicking benign conditions such as intra-articular localized nodular synovitis [7]. The most common site of occurrence is around large joints frequently knee joints and ankle, comprising approximately two-thirds of total incidences [8]. This malignancy usually has an overall poor prognosis with a 5-year survival rate of 59–75% [8,9]. In a few cases, these tumors may be confused with benign intra-articular lesions such as pigmented villonodular synovitis (PVNS), synovial osteochondromatosis (SOC), and synovial hemangioma [10,11,12]. Various surgical interventions were employed in the case series, including excision (arthroscopic/open), radical tumor resection, neoadjuvant chemotherapy, radiotherapy, and even amputation, depending on the individual case’s characteristics and requirements. The present case underwent excision via arthroscopy. Even though SS can present as benign lesions, certain cases of SS appear to exhibit distinct behavioral patterns compared to others. Hence, it is important for prompt diagnosis and appropriate treatment.
A 25-year-old South Indian man, doing his graduation and playing recreational sports, presented with right knee pain and restricted flexion beyond 100° for the past 4 years and increased in severity for the past 6 months. In 2023, he sought treatment for knee pain and restricted mobility in the form of physiotherapy with no relief from his symptoms Even though the image quality was poor; a cystic lesion could be identified close to the lateral femoral condyle proximal aspect with surrounding soft-tissue edema (Fig. 1). Despite undergoing multiple physiotherapy sessions, the stiffness persisted along with mild intermittent anterolateral knee pain. Although he reported no systemic symptoms, he had pain and discomfort during his regular and sports activities.
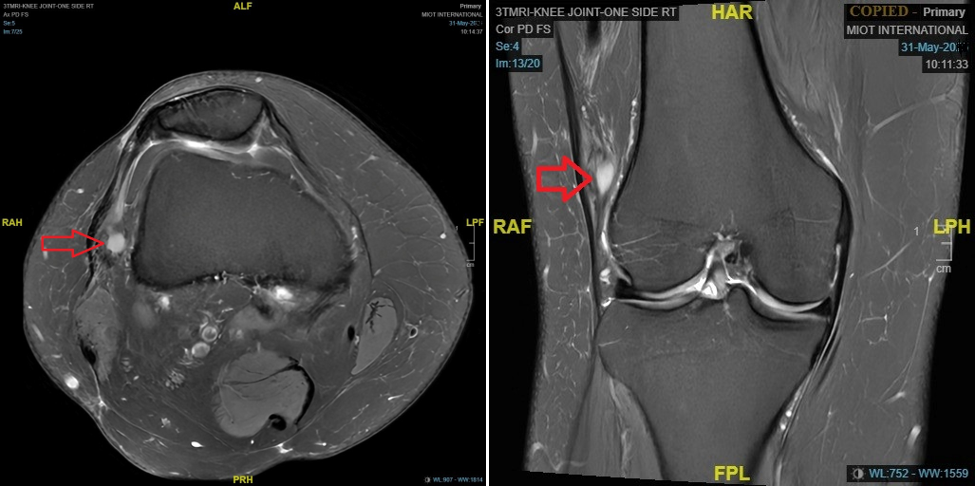 During the clinical examination, a point tenderness was appreciated over the lateral femoral condyle with no effusion or synovitis. Range of motion was 0–100° further restricted and associated with pain. The Lachman test indicated no laxity. Collateral ligaments were stable, and no distal neurovascular deficits. MRI images (Fig. 1) reported by the senior musculoskeletal radiologist suggested a probability of nodular synovitis/ganglion cyst/venous malformation as potential diagnoses, as the lesion is <5 cm with no distinct features suggesting toward the SS, it is not included in the differentials. The lesion demonstrated well-defined margins, homogenous signal, lack of aggressive bone or soft-tissue invasion, and no red flags, including periosteal reaction or bone destruction so contrast MRI was not done. Surgery was conducted under general anesthesia and adductor canal block with tourniquet control. Standard anterolateral, anteromedial portals, superolateral, and accessory anterolateral portals were established. During the arthroscopic evaluation, anterior cruciate ligament and posterior cruciate ligament appeared intact and the medial and lateral compartments appeared pristine, except for the lateral gutter showing a cystic swelling adhered to the lateral femoral condyle, we thought of venous malformation/ganglion cyst (Fig. 2 and 3) for which biopsy was obtained and sent for histopathological examination, rest of the lesion removed by using motorized shaver and surrounding tissue was cauterized to ensure lesion free margins and knee portals were closed and regular physiotherapy initiated postoperatively.
During the clinical examination, a point tenderness was appreciated over the lateral femoral condyle with no effusion or synovitis. Range of motion was 0–100° further restricted and associated with pain. The Lachman test indicated no laxity. Collateral ligaments were stable, and no distal neurovascular deficits. MRI images (Fig. 1) reported by the senior musculoskeletal radiologist suggested a probability of nodular synovitis/ganglion cyst/venous malformation as potential diagnoses, as the lesion is <5 cm with no distinct features suggesting toward the SS, it is not included in the differentials. The lesion demonstrated well-defined margins, homogenous signal, lack of aggressive bone or soft-tissue invasion, and no red flags, including periosteal reaction or bone destruction so contrast MRI was not done. Surgery was conducted under general anesthesia and adductor canal block with tourniquet control. Standard anterolateral, anteromedial portals, superolateral, and accessory anterolateral portals were established. During the arthroscopic evaluation, anterior cruciate ligament and posterior cruciate ligament appeared intact and the medial and lateral compartments appeared pristine, except for the lateral gutter showing a cystic swelling adhered to the lateral femoral condyle, we thought of venous malformation/ganglion cyst (Fig. 2 and 3) for which biopsy was obtained and sent for histopathological examination, rest of the lesion removed by using motorized shaver and surrounding tissue was cauterized to ensure lesion free margins and knee portals were closed and regular physiotherapy initiated postoperatively.
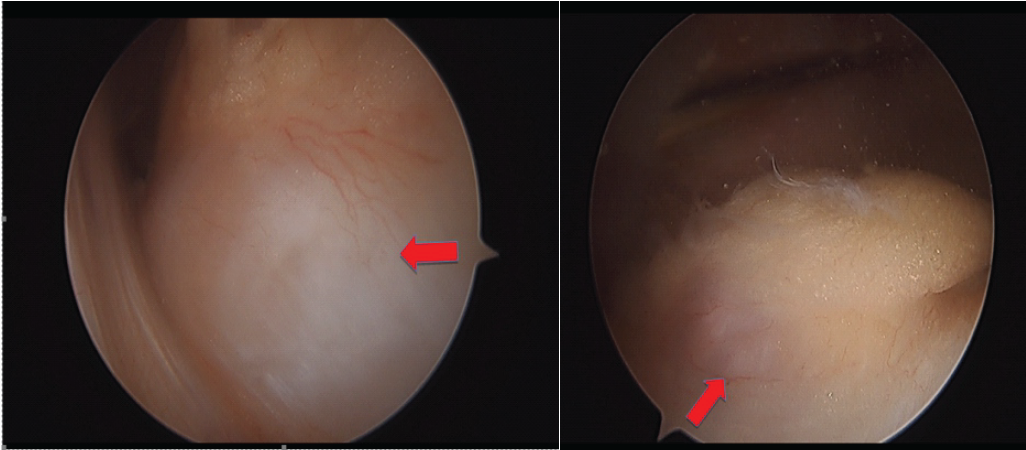
Figure 2: Intraoperative picture of the arthroscopic lateral gutter view with lesion in the right knee.

Figure 3: Photograph of removed gross specimen
Surprisingly, the biopsy revealed SS, characterized by tumor cells forming short intersecting fascicles with nuclear pleomorphism, elongated spindle cells, fine chromatin, scant cytoplasm, low mitotic activity, and no necrosis (Fig. 4). Immunohistochemistry indicated positivity for Pan Cytokeratin and Transducin-like enhancer of split 1 consistent with a monophasic type of SS. An expert oncology panel was convened to plan further management. Follow-up positron emission tomography-computed tomography (PET-CT) at 3 weeks post-surgery showed post-operative inflammation in the right knee joint synovium without residual disease with no systemic involvement. Subsequent treatment included local radiotherapy with a total dose of 54 Gy and 6 cycles of adjuvant chemotherapy with Adriamycin, Mesna, and ifosfamide over 16 weeks. The patient tolerated the therapy with no complications. The patient maintains good knee function, with no signs of disease recurrence at 14 months post-surgery. Follow-up PET-CT scan at 12 months post-operative showed no residual disease. He was advised to have yearly follow-ups due to the potential for late relapse.
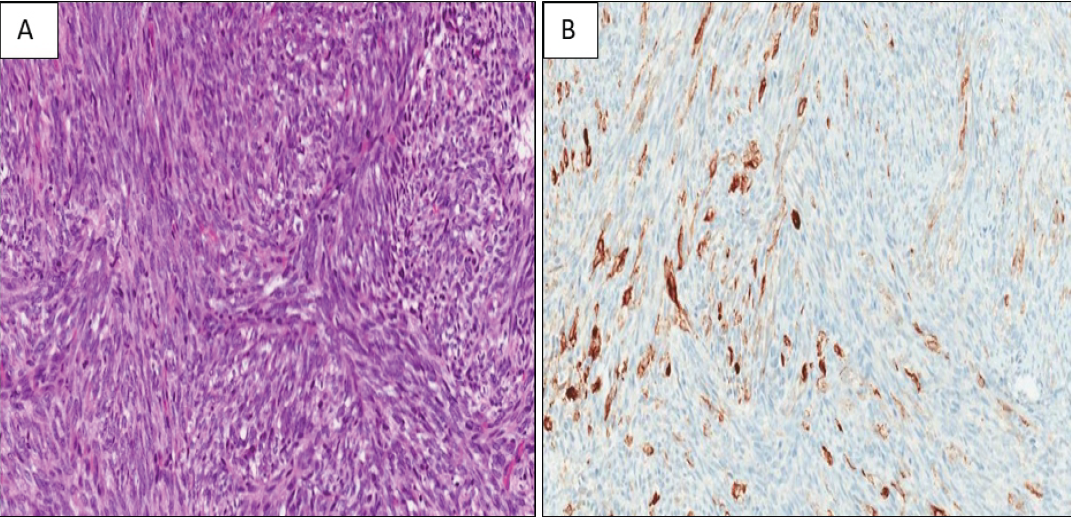
Figure 4: Histopathology assessment (a) Hematoxylin and Eosin staining of ×200 magnification fascicles of spindle cells seen with minimal atypia. (b) Pan Cytokeratin ×200 magnification.
Most intra-articular tumors are benign (non-cancerous), and they are rare. Rarely do primary intra-articular sarcomas occur. Less than 5% of instances of SS begin in a joint, despite the fact that it makes up 5–10% of all soft-tissue sarcomas [13]. SS are not derived from synovial tissue, despite their name. Rather, the misnomer comes from the fact that they typically occur close to joint gaps [14]. Only 23 cases of primary, intra-articular SS, including our patient, have been published in the literature, and only 13 cases of intra-articular SS have been reported in the last 10 years, demonstrating how uncommon this condition is still. Along with our instance, the majority of all cases that have been recorded to yet started in the knee.

Table 1: Table presenting the other similar type of cases
SS is known to have a benign presentation often diagnosed after surgical excision of misdiagnosed benign lesions, same happened with our case as well, but with suspicion of lesion we have employed complete resection of lesion through arthroscopy and thermal ablation of the margins for tumor-free margins as it is one of the employed technique in the reviewed literature. As the MRI characteristics of intra-articular SS are generally non-specific, as the lesion is <5 cm, demonstrating homogenous signal intensity with well-circumscribed margins, making accurate diagnosis more difficult [15], which made our diagnosis doubtful. Till to date, only nine cases of intra-articular SS have been reported with specific MRI findings [16]. Intra-articular SS is a highly uncommon condition. The knee joint is the most frequently affected site, accounting for 88% of cases. Due to its uncommon occurrence, slow growth and vague clinical and radiological features, intra-articular SS can cause a significant delay in diagnosis and treatment [6]. Biphasic SS demonstrated a markedly higher survival rate in histological comparisons to monophasic variants, indicating distinct biological behaviors associated with the different histotypes [10,17]. This case report is interesting in the sense that we could have been easily misled to not address the nodular lesion, as the patient was not significantly symptomatic except for terminal flexion restriction. Despite the higher threshold to explore the lesion, a correct decision was made ultimately which guided us to the reality of the presence of a SS. The fact that the patient had symptoms for 4 years before the first “evidence” of the cyst creates the possibility of this lesion being undercover for several years which was excised through arthroscopy and followed by chemo and radiotherapy. Excision of these masses has shown to leave residual tumor in up to 82% of cases [15,18,19]. (Table 1). Radiotherapy has a well-established role in improving local control, but while surgery and radiation therapy have achieved excellent local control, distant metastasis remains the principal problem limiting survival [20,21]. Adjuvant chemotherapy helped to increase long-term survival for SS, a soft-tissue sarcoma that is susceptible to chemotherapy [9]. Ifosfamide-based chemotherapy has been associated with an improved survival in patients with SS [22]. Chemotherapy combined with surgical excision and radiation therapy increases overall survival to 80–95% after 3 years [23,24]. This was employed in our case showing no recurrence after 12 months with follow-up PET CT and MRI. Nevertheless, it is important to include intra-articular SS in the differential diagnosis of an intra-articular mass, particularly in the knee joint, when the radiological features do not align with those of SOC, synovial hemangioma, or PVNS.
This case highlights the diagnostic challenge posed by intra-articular SS, particularly when presenting with non-specific symptoms and radiological findings. Despite long-standing knee pain and restricted motion, the lesion was initially presumed benign, underscoring the importance of maintaining a broad differential diagnosis for persistent intra-articular masses. Early arthroscopic intervention, followed by histopathological evaluation, was crucial in identifying the true nature of the pathology. The timely diagnosis and multidisciplinary management enabled a favorable outcome, with the patient showing no recurrence at 14 months postoperatively. This case emphasizes the need for heightened clinical suspicion and thorough evaluation in cases of atypical or unresolving joint symptoms, even in young, otherwise healthy individuals.
This case emphasizes that not every long-standing “Nodular synovitis/Ganglion cyst” is benign enough to be ignored. Prompt evaluation must be done radiologically before surgery to prevent unwarranted consequences. Multi-disciplinary approach helps in preventing recurrence and improves the long-term survival rate of the patient.
References
- 1. Almodumeegh AS, Nouri MT, Mortada H, AlHasan MO, Obeid FM, Kattan AE. The potential pitfalls of synovial sarcoma mimicking intraneural ganglion cyst: A case report and literature review. Int J Surg Case Rep 2023;104:107916. [Google Scholar] [PubMed]
- 2. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors. 5th ed. Philadelphia, PA: Mosby-Elsevier; 2008. [Google Scholar] [PubMed]
- 3. Friedman MV, Kyriakos M, Matava MJ, McDonald DJ, Jennings JW, Wessell DE. Intra-articular synovial sarcoma. Skeletal Radiol 2013;42:859-67. [Google Scholar] [PubMed]
- 4. Toro JR, Travis LB, Wu HJ, Zhu K, Fletcher CD, Devesa SS. Incidence patterns of soft tissue sarcomas, regardless of primary site, in the surveillance, epidemiology and end results program, 1978-2001: An analysis of 26,758 cases. Int J Cancer 2006;119:2922-30. [Google Scholar] [PubMed]
- 5. Hellwinkel JE, Farmer RP, Heare A, Smith J, Donaldson N, Fadell M, et al. Primary intra-articular synovial sarcoma of the knee: A report of two cases and review of the literature. Int J Radiol Imaging Technol 2018;4:031. [Google Scholar] [PubMed]
- 6. Al-Mohrej OA, Al-Jarallah SA, Al-Dakhil Allah HH, Pant R, Al-Zayed ZS. Synovial sarcoma presenting as an intra-articular mass in a pediatric patient: A case report. BMC Musculoskelet Disord 2020;21:283. [Google Scholar] [PubMed]
- 7. Caravias P. Sarcoma sinovial de rodilla. Rev Asoc Argent Ortop Traumatol 1996;60:79-83. [Google Scholar] [PubMed]
- 8. Sultan I, Rodriguez-Galindo C, Saab R, Yasir S, Casanova M, Ferrari A. Comparing children and adults with synovial sarcoma in the surveillance, epidemiology, and end results program, 1983 to 2005: An analysis of 1268 patients. Cancer 2009;115:3537-47. [Google Scholar] [PubMed]
- 9. Steinstraesser L, Agarwal R, Stricker I, Steinau HU, Al-Benna S. Biphasic synovial sarcoma of the extremity: Quadruple approach of isolated limb perfusion, surgical ablation, adipofascial perforator flap and radiation to avoid amputation. Case Rep Oncol 2011;4:222-8. [Google Scholar] [PubMed]
- 10. Ishida T, Iijima T, Moriyama S, Nakamura C, Kitagawa T, Machinami R. Intra-articular calcifying synovial sarcoma mimicking synovial chondromatosis. Skeletal Radiol 1996;25:766-9. [Google Scholar] [PubMed]
- 11. Namba Y, Kawai A, Naito N, Morimoto Y, Hanakawa S, Inoue H. Intraarticular synovial sarcoma confirmed by SYT-SSX fusion transcript. Clin Orthop Relat Res 2002;395:221-6. [Google Scholar] [PubMed]
- 12. Blay JY, Von Mehren M, Jones RL, Martin-Broto J, Stacchiotti S, Bauer S, et al. Synovial sarcoma: Characteristics, challenges, and evolving therapeutic strategies. ESMO Open 2023;8:101618. [Google Scholar] [PubMed]
- 13. Gazendam AM, Popovic S, Munir S, Parasu N, Wilson D, Ghert M. Synovial sarcoma: A clinical review. Curr Oncol 2021;28:1909-20. [Google Scholar] [PubMed]
- 14. Jo VY, Fletcher CD. WHO classification of soft tissue tumours: An update based on the 2013 (4th) edition. Pathology 2014;46:95-104. [Google Scholar] [PubMed]
- 15. Ferrari A, De Salvo GL, Brennan B, Van Noesel MM, De Paoli A, Casanova M, et al. Synovial sarcoma in children and adolescents: The European pediatric soft tissue sarcoma study group prospective trial (EpSSG NRSTS 2005). Ann Oncol 2015;26:567-72. [Google Scholar] [PubMed]
- 16. Talamo F, Varaona JM, Jorge F, Muzzio A. Synovial sarcoma of the knee: Case report. Rev Asoc Argent Ortop Traumatol 2024;89:538-43. [Google Scholar] [PubMed]
- 17. Guillou L, Benhattar J, Bonichon F, Gallagher G, Terrier P, Stauffer E, et al. Histologic grade, but not SYT-SSX fusion type, is an important prognostic factor in patients with synovial sarcoma: A multicenter, retrospective analysis. J Clin Oncol 2004;22:4040-50. [Google Scholar] [PubMed]
- 18. Choi ES, Han I, Cho HS, Kang HG, Kim JH, Kim HS. Distinct clinical characteristics of unplanned excision in synovial sarcoma. Clin Orthop Surg 2015;7:254-60. [Google Scholar] [PubMed]
- 19. Ferrari A, Miceli R, Rey A, Oberlin O, Orbach D, Brennan B, et al. Non-metastatic unresected paediatric non-rhabdomyosarcoma soft tissue sarcomas: Results of a pooled analysis from United States and European groups. Eur J Cancer 2011;47:724-31. [Google Scholar] [PubMed]
- 20. Fiore M, Sambri A, Spinnato P, Zucchini R, Giannini C, Caldari E, et al. The biology of synovial sarcoma: State-of-the-art and future perspectives. Curr Treat Options Oncol 2021;22:109. [Google Scholar] [PubMed]
- 21. Bergovec M, Smerdelj M, Bacan F, Seiwerth S, Herceg D, Prutki M. Intraarticular synovial sarcoma of the knee rising from a lateral meniscus – a case report. Orthop Traumatol Surg Res 2018;104:227-30. [Google Scholar] [PubMed]
- 22. Asiri Y, Almushayqih M, Alshamlan N, Alshaalan M. Case report of intra-articular synovial sarcoma in the hip joint. Radiol Case Rep 2020;15:1256-60. [Google Scholar] [PubMed]
- 23. McLain R, Buckwalter J, Platz CE. Synovial sarcoma of the knee: Missed diagnosis despite biopsy and arthroscopic synovectomy. A case report. J Bone Joint Surg Am 1990;72:1092-4. [Google Scholar] [PubMed]
- 24. Saito K, Kawabata Y, Kobayashi N, Iwashita H, Kato I, Otani M, et al. A rare case of intra-articular synovial sarcoma of the hip joint: A case report with intra-articular findings via hip arthroscopy. J Surg Case Rep 2023;2023:rjad066. [Google Scholar] [PubMed]
- 25. Hara H, Kawamoto T, Onishi Y, Fujioka H, Nishida K, Kuroda R, et al. Reconstruction of the midfoot using a free vascularized fibular graft after en bloc excision for giant cell tumor of the tarsal bones: A case report. J Foot Ankle Surg 2016;55:838-41. [Google Scholar] [PubMed]
- 26. Gupta A, Choudhary M, Gupta N, Kulhari S, Pachar S. Monophasic synovial sarcoma: A case report and literature review. Int J Contemp Pediatr 2016;3:1092-5. [Google Scholar] [PubMed]
- 27. Hara S, Hatori M, Hosaka M, Komatsu T, Tsuchiya T, Kimura N. Synovial sarcoma with massive ossification–a case report. Ups J Med Sci 2003;108:151-8. [Google Scholar] [PubMed]