Dynamic radiography can provide useful diagnostic information on early loosening in patients with painful total hip arthroplasty when gross mobility of the acetabular component is present.
Dr. Maria Tsatlidou, Department of Orthopaedic, European Interbalkan Medical Center, Thessaloniki, Greece. E-mail: maria.tsatlidou@yahoo.com and info@mariatsatlidou.gr
Introduction: Among all the causes of revision surgery after total hip arthroplasty (THA), loosening is the most common. However, in cases of early component loosening, the sole symptom is pain, and the diagnosis is challenging. In this study, a novel use of dynamic radiography is proposed as a diagnostic tool to detect acetabular cup gross mobility.
Case Report: A single case of early acetabular cup loosening in a 57-year-old female patient is presented. The patient complained of pain during weight-bearing 2 months postoperatively with progressive aggravation. Dynamic radiography is very rarely proposed in the literature as a valid method to detect gross movement of the acetabular cup in a suspected loose THA.
Conclusion: Aseptic loosening of THA components is frequently the cause of pain during mobilization, requiring revision arthroplasty. In cases of early loosening with component micromovement, dynamic radiography can be a useful imaging method when plain X-rays and computed tomography scans are inconclusive.
Keywords: Total hip arthroplasty, acetabular cup loosening, dynamic radiography, early loosening.
Aseptic loosening is one of the most common causes of painful total hip arthroplasty (THA) leading to revision [1,2,3]. Although aseptic loosening of either THA components is suspected in a painful hip a few years after reconstruction and is usually caused by debris of the bearing surfaces, it can also be the case in early pain during weight-bearing [1,2]. Improper fixation, or lack of osseointegration, may result in micromotion of the THA components, causing discomfort to the patient soon after the arthroplasty. Some of the factors related to insufficient osseointegration of the implant are surgical technique deficits, patient-related factors, and implant characteristics and properties [1,2].
The diagnosis of a loosen component is challenging. Multiple imaging techniques are available for the evaluation of the positioning and stability of the implants. In addition, new emerging technologies with detecting sensors may help in the diagnosis of loosen THA components [4,5,6].
We present a rare case of a 57-year-old female with persistent pain of the hip shortly after THA, who was diagnosed with loosen acetabular cup using dynamic radiographs, while no findings of osteolysis were present either in plain radiographs or computed tomography (CT) and magnetic resonance imaging (MRI) images. The serial imaging revealed movement of the acetabular cup and the decision for revision was made.
Press-fit type THA was performed on a 57-year-old patient who suffered from chronic symptoms of hip osteoarthritis (Fig. 1 and 2).
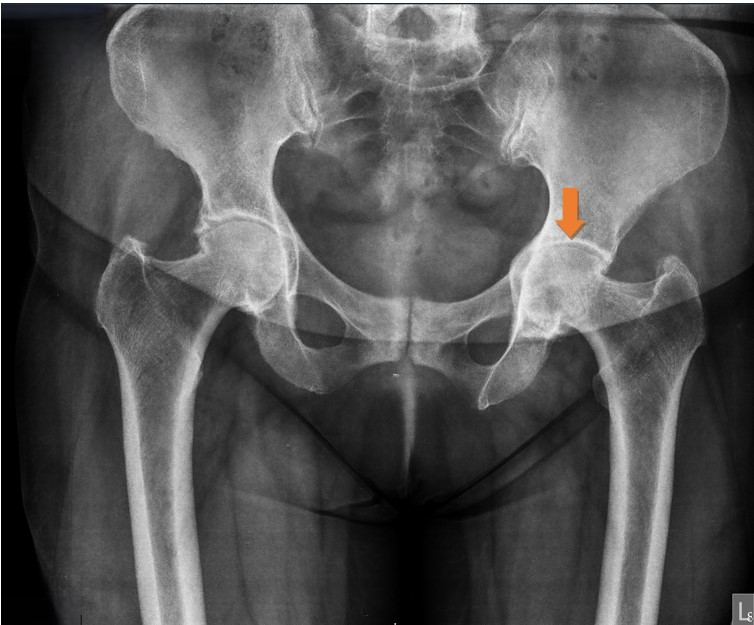
Figure 1: Pre-operative pelvis X-ray, anteroposterior view. Moderate left hip joint arthritis.
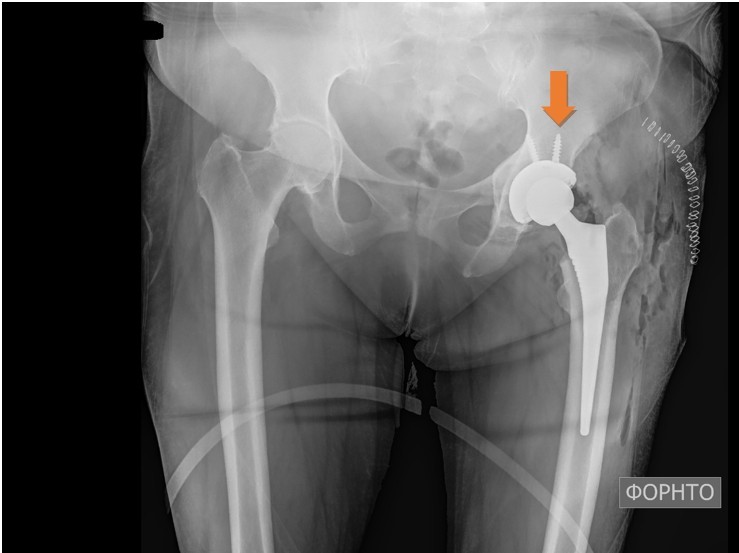
Figure 2: Post-operative X-ray of the hips. Left total hip replacement.
Although no instability or gross motion of any of the components was detected intraoperatively, the acetabular cup was fixated with two screws to reinforce the stability of the construct. The post-operative protocol comprised non-weight-bearing for the first 2 weeks, partial weight-bearing for the following weeks and initiation of full weight-bearing at 6 weeks postoperatively. At the 2-month follow-up visit the patient was able to weight bear and walk but complained of pain when rising from the seated position and during the first steps. The symptoms were improving during walking. Clinical examination revealed a leg-length discrepancy of approximately 2 cm, but the radiological evaluation showed no pathological findings. The patient was encouraged to continue rehabilitation, return to moderate daily activities, but to avoid overload. Six months postoperatively, the symptoms significantly worsened with severe pain during loading and a “snapping” feeling on every step. A thorough laboratory investigation was obtained showing no increase in inflammation markers and no other pathological findings. Further imaging with new X-rays, MRI, and CT was also inconclusive (Figs. 3, 4, 5).

Figure 3: No periprosthetic lucencies at the 6-month post-operative X-ray.
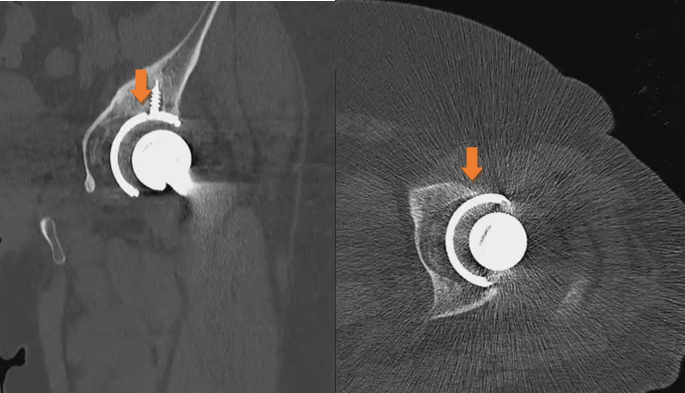
Figure 4: Pre-operative computed tomography scan with no sign of acetabular cup loosening.
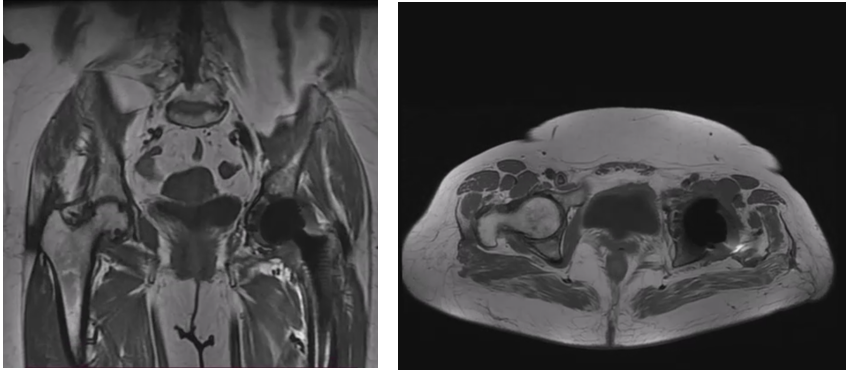
Figure 5: Pre-operative evaluation with MRI, no loosening findings.
Taking into consideration the short post-operative time, it was decided to avoid any nuclear medicine examination, such as single-photon emission computed tomography (SPECT)-CT or positron emission tomography (PET) to limit the risk of exposure. It is shown that these imaging modalities present lower accuracy in the early post-operative period. Given the fact that there were no signs of infection, early loosening of the THA components was suspected, and so a dynamic radiographic imaging was scheduled to examine the THA prostheses during movement. The examination was undertaken in the radiology department with the equipment of a barium meal gastrointestinal series for high-resolution imaging. The patient was placed in a supine position with the affected limb free and the chest, abdomen, and genitalia of the patient covered with a radioprotective gown. The surgeon passively performed hip flexion, hip extension, internal and external rotation to the extremes of the hip range of motion of the left lower extremity under radiography. The movements were performed in a circular manner, anti-clockwise starting from 60° flexion and internal rotation to full external rotation followed by hip extension. The same movement protocol was followed in 90° flexion and in 100° of hip flexion. Dynamic imaging revealed gross motion of the acetabular cup during passive movements of the hip joint, so the diagnosis of aseptic loosening was established (Fig. 6 and Video 1).
The patient was scheduled for revision arthroplasty. The surgery was undertaken 2 weeks after, and loosening of acetabular cup was confirmed intraoperatively. There were no signs of loosening of the femoral component or infection. Samples were sent to detect possible infection. Loosen cup was removed and exchanged to a larger tantalum cup. The post-operative course was uneventful, and a full recovery was succeeded. At 2, 6, and 12-month follow-up the patient had a painless range of motion and had fully returned to her activities (Fig. 7). At a final follow-up at 18 months, the patient presented with a significant improvement in function and quality of life compared to the pre-operative evaluation. Her pain was limited from a Visual Analog Scale (VAS) = 7 preoperatively to VAS = 2 postoperatively.
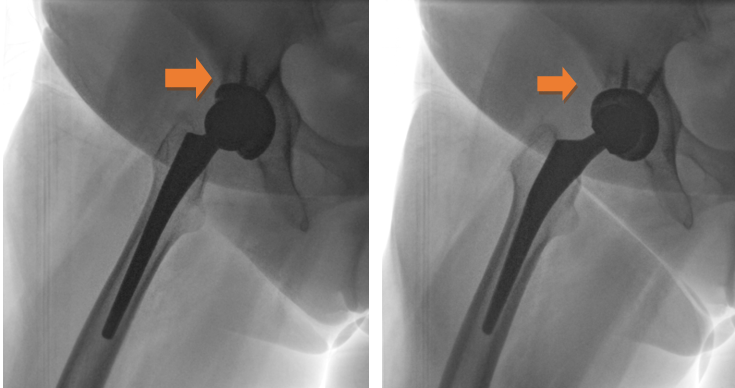
Figure 6: Images during dynamic radiography.

Figure 7: Post-operative imaging after revision surgery.
Video 1: Gross motion and instability of the acetabular cup during dynamic radiography.
Instability of the cementless acetabular cup is caused either due to lack of osseointegration, found mainly early after the operation, or due to aseptic loosening which is associated with wear debris that initiates an inflammatory response leading in bone resorption. It has been shown that regarding the implant properties, trabecular acetabular cups fixated with screws have a lower risk of loosening [1]. However, comorbidities as diabetes, rheumatoid arthritis, sickle cell anemia, and obesity may delay the osseointegration process [3]. Surgeon’s experience, optimal implant positioning, and implant stability as confirmed intraoperatively are related to lower aseptic loosening risk and lower revision rates [1,3]. Cherian et al. found that male sex and high activity levels are the only factors that are associated with a higher risk of THA aseptic loosening [3].
According to Mjoberg, early acetabular cup loosening is initiated intraoperatively or shortly after surgery due to poor bone quality or bone resorption after bone trauma. Its further progression is related purely to the biomechanical traits of the arthroplasty and the loading of the components during simple daily activities. Another factor contributing to early loosening is fluid pressure fluctuation that leads to further osteolysis, especially in uncemented cups with screw holes [2].
A variety of imaging techniques have been described to assess the outcome of a reconstruction surgery and differentiate a possible complication. Lombard et al. have introduced a diagnostic algorithm to THA complications based on CT scanning of bone and hardware defects and dynamic US to appreciate soft tissue problems [5].
The diagnosis of aseptic loosening is mainly based on osteolytic findings and proximal migration, either on X-rays or CT scans. Although advanced imaging options are available, radiography is the gold standard for diagnosing early loosening. The positioning of the implants and their alignment, as well as radiolucency, is being assessed and may lead to a risk estimation for component instability [4]. It has been shown that radiolucent areas of thickness >2 mm are highly indicative of loosening. Even the location of the radiolucency, according the DeLee and Charnley classification, plays a role in identifying the risk of loosening [4,5,6]. The addition of a contrast agent may increase the sensitivity of the examination by 4% according to Hosseini et al. [4]. However, there are considerations over the use of arthrography, and the literature is inconclusive regarding its diagnostic value [4].
According to many authors [5,6,7], MRI can reliably diagnose bone resorption and fibrous tissue formation around the THA components, as well as to differentiate mechanical loosening from infection. However, there can be limitations in MRI quality due to the hardware that frequently results in image distortion. Koff et al. have provided a detailed protocol to reduce the artifacts and raise the sensitivity level of MRI when assessing THA to up to 95–100%, significantly higher than CT scan and radiographs [7].
Furthermore, nuclear medicine provides great sensitivity in the imaging of a loose THA component. SPECT-CT combines the CT technology and the gamma cameras. With the use of Tc99 in the three-phase scintigraphy, the obtained information is more detailed. Apart from the possible migration and the lucencies, an increased radioactivity around the implants on all phases can establish the diagnosis of component loosening [8]. The use of scintigraphy may be restricted due to relatively low specificity and high radiation exposure. Fludeoxyglucose-18-PET can be a good alternative with higher sensitivity and specificity. PET scan is shown to be very useful for the differentiation between infection and aseptic loosening with relatively lower exposure. However, the high cost of both these imaging methods is a significant limitation to their wide use.
New technologies have also been introduced in medical research and clinical practice to enable early diagnosis of implant micromovement. Acoustic emission (ΑΕ) monitoring could be a non-invasive diagnostic tool for early loosening as it is based on the conversion of dynamic surface motion into electric signals. The current literature provides very promising results of the use of AE sensors to distinguish early defects, especially regarding THA implants [4,9].
Sonography is a significant tool for guided joint aspiration, dynamic evaluation of periarticular soft tissues, and possible impingement. However, it is not reported to be suitable for the imaging of the THA hardware [10,11]. The sensitivity of US imaging regarding aseptic loosening is very low, and usually the detection of joint effusion or extra-articular fluid is indicative of infection.
Dynamic imaging has been proposed as a technique that can detect gross mobility in TKA [10]. Homma et al. 2020 presented a case of trunniosis, in which dynamic fluoroscopy was implemented and movement of the femoral stem in the head was detected as a result to disruption of the head-neck junction [12]. This is the closest to our approach, where the movement of the acetabular component was found under dynamic radiography.
Dynamic radiography, as presented in this case report, can provide the clinician with an additional diagnostic tool when the traditional imaging is unclear or hardly applicable due to low sensitivity in the early post-operative period after THA. Naturally, as a case report, the present article has specific limitations regarding the generalization of the findings in all painful THA cases. The short follow-up period and the lack of a standardized protocol that increases the variability of how the test is performed are further limitations of the study. However, in cases of painful THA when infection is excluded but the imaging is inconclusive, the dynamic radiography can offer a direct confirmation of the loosening. As the motion of the loose component is visualized, the diagnosis is established with a method that is safe, easy to perform, and cost-effective, compared to more advanced imaging or nuclear studies.
To the best of our knowledge, serial radiography during passive movement has not been described in the literature as an imaging modality to assess a suspected THA loosening. The present article shows that dynamic radiography can be an excellent method to distinguish gross mobility of THA components being also relatively safe and cost-effective as well as easily accessible.
Dynamic radiography is proposed as a diagnostic approach for THA cases where lack of osseointegration is suspected. The detected component mobility may overcome the limitations of the traditional diagnostic methods.
References
- 1. Apostu D, Piciu D, Oltean-Dan D, Cosma D, Lucaciu O, Popa C, et al. How to prevent aseptic loosening in cementless arthroplasty: A review. Appl Sci 2022;12:1571. [Google Scholar] [PubMed]
- 2. Mjöberg B. Is early migration enough to explain late clinical loosening of hip prostheses? EFORT Open Rev 2020;5:113-7. [Google Scholar] [PubMed]
- 3. Cherian JJ, Jauregui JJ, Banerjee S, Pierce T, Mont MA. What host factors affect aseptic loosening after THA and TKA? Clin Orthop Related Res 2015;473:2700-9. [Google Scholar] [PubMed]
- 4. Hosseini S, Claramunt R, Ros A. Non-invasive technologies for diagnostics of orthopaedic implant fixation. Med Devices Sens 2020;3:e10125. [Google Scholar] [PubMed]
- 5. Lombard C, Gillet P, Germain E, Boubaker F, Blum A, Gondim Teixeira PA, et al. Imaging in hip arthroplasty management part 2: Postoperative diagnostic imaging strategy. J Clin Med 2022;11:4416. [Google Scholar] [PubMed]
- 6. Deshmukh S, Omar I. Imaging of hip arthroplasties: Normal findings and hardware complications. Semin Musculoskeletal Radiol 2019;23:162-76. [Google Scholar] [PubMed]
- 7. Koff MF, Burge AJ, Potter HG. Clinical magnetic resonance imaging of arthroplasty at 1.5 T. J Orthop Res 2020;38:1455-64. [Google Scholar] [PubMed]
- 8. Tam HH, Bhaludin B, Rahman F, Weller A, Ejindu V, Parthipun A. SPECT-CT in total hip arthroplasty. Clin Radiol 2014;69:82-95. [Google Scholar] [PubMed]
- 9. Khokhlova L, Komaris DS, Tedesco S, O’Flynn, B. Assessment of hip and knee joints and implants using acoustic emission monitoring: A scoping review. IEEE Sens J 2021;1:14379-88. [Google Scholar] [PubMed]
- 10. Feiock DA, Newman JS, Newberg AH. Radiological evaluation of total knee arthroplasty. In: Bono JV, Scott RD, editors. Revision Total Knee Arthroplasty. New York: Springer; 2005. [Google Scholar] [PubMed]
- 11. Long SS, Surrey D, Nazarian LN. Common sonographic findings in the painful hip after hip arthroplasty. J Ultrasound Med 2012;31:301-12. [Google Scholar] [PubMed]
- 12. Homma Y, Morikawa T, Ishii S, Baba T, Kaneko K. Bowing-head sign: Rare but detectable in pre-catastrophic hip implant failure. Arch Orthop Trauma Surg 2020;140:2085-9. [Google Scholar] [PubMed]








