Successful treatment of femoral neck fractures depends on accurate reduction, preserving blood supply, and choosing the right implant.
Dr. Janki Sharan Bhadani, Secretary, Orthopaedic Research and Education foundation- India, Consultant and DNB Appraiser, Department of Orthopaedics, Paras HMRI Hospital, Patna, India, Email: jsbhadani@gmail.com
The management of femoral neck fractures, remains one of the most challenging problems. The term unsolved fracture still holds good for these. Osteosynthesis continues to hold paramount importance in preserving the native hip joint. However, the success of internal fixation depends on a better understanding of biology, mechanics, and factors which respect these two. Therefore, preserving vascularity during anatomical reduction is as vital as selecting the right implant.[1]
The precarious vascularity of the femoral head, primarily dependent on the lateral epiphyseal vessels arising from the medial femoral circumflex artery, dictates the long-term viability of osteosynthesis. the superolateral vessels supplying the pyriformis fossa are critical for the blood supply to the femoral head.[2] Every surgical step must be executed with the intent of minimizing further insult to already compromised vascularity. Avoidance of unnecessary capsulotomy, and limited periosteal stripping are essential to preserve perfusion. Moreover, the question of capsular decompression for intracapsular hematoma remains relevant; while evidence is mixed, decompression may improve head perfusion in selected cases.
The quality of reduction is one of the most important factors in deciding the outcome. Even a small mal-reduction increases the chances of nonunion and avascular necrosis. Closed reduction is the first choice, aiming for anatomic alignment without too much manipulation. Manipulation should be done through the distal limb and not by twisting the head or proximal fragment. In long spiral femoral neck fractures, usually from twisting injuries, the medial and posterior cortex may be comminuted, this must be considered during reduction.The Whitman manoeuvre is preferred over the Leadbetter manoeuvre because it requires comparatively lesser manipulation.
Preserving the capsule is important. If open reduction is required only the anterior capsule should be cut, which helps reduce the tamponade effect caused by hematoma inside the capsule. In cases where the fracture is irreducible, open reduction should be done using a minimally invasive approach. Surgeons must remember that fixation cannot make up for poor reduction, good stability comes only after proper alignment.[3] Lowell’s criteria are used intraoperatively under fluoroscopy and on postoperative X-rays to assess reduction in femoral neck fractures. A smooth, continuous S-shaped curve at the head–neck junction indicates good reduction, whereas a broken curve, notch, or double contour suggests malreductions.[4]
Guidewires help maintain reduction during reaming and fixation. Placing a few guidewires before reaming prevents rotation of the femoral head, as even slight movement can damage blood vessels and lead to avascular necrosis. The guidewire should always be directed toward the fovea for proper alignment.[1] While drilling into the femoral head, the DHS screw tip should lie just beneath the subchondral bone. This provides strong fixation and reduces the risk of failure. If the TAD is more than 25 mm, the screw may end up in Ward’s triangle, an area of poor bone quality, increasing the risk of implant failure. Thus the tip-apex distance (TAD) should be less than 25 mm for stronger fixation and fewer failures
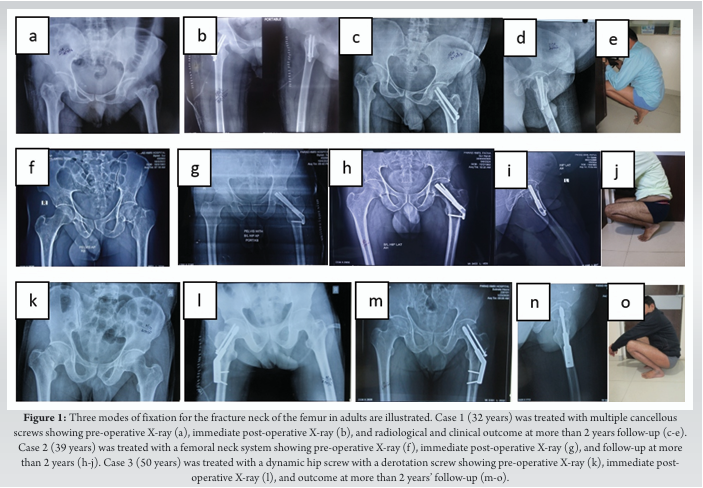
The choice of implant for neck of femur fractures depends on fracture pattern, bone quality, and patient profile. Multiple cancellous screws are a reliable option for nondisplaced or valgus-impacted fractures. In displaced or vertically oriented Pauwels type III fractures, stronger constructs such as the dynamic hip screw (DHS) with a derotation screw, or the femoral Neck System (FNS) are preferred.[5] [Fig. 1] Other available options include multiple parallel screw fixation, and the proximal femoral locking plate (PFLP), though the latter is less commonly used in current practice. Newer concepts like Biplane Double Supported Screw Fixation (BDSF) have shown improved biomechanical stability in vertical and unstable fracture patterns.[6].
In younger patients with good bone quality, multiple cancellous screws are usually sufficient and help preserve bone stock. However, repeated attempts with guidewires should be avoided, as this may weaken the bone and create stress risers for future fractures.[7] In middle-aged or older patients, bone quality is weaker, so DHS with an anti-rotation screw is often a better option. The screw should engage the calcar region for stronger purchase. Newer implants like the femoral neck system (FNS) show promising early results, but their small area of fixation can be a disadvantage in osteoporotic bone. The basic biomechanical principles remain the same like achieve good spread of screws across the femoral head, place them subchondral for strong purchase, and maintain a TAD <25mm.
The decision to attempt osteosynthesis is based on the meticulous technique including precise execution, achieving reduction that restores femoral neck anatomy, employing implants considering bone quality that match biomechanical demands, and respecting the biology of blood supply. While arthroplasty offer reliable alternatives, the preservation of the native hip through osteosynthesis remains a worthy whenever possible. Thus, one must approach these fractures judiciously, keeping in mind that the price of error is high, but the reward of a preserved and smoothly functioning hip after osteosynthesis is equally valuable, giving us a deep sense of satisfaction.
Every surgical step in femoral neck fracture fixation must respect the precarious blood supply, of the femoral head, as preservation is key to long-term success. Anatomical reduction, preferably achieved with minimal manipulation, is more critical than any implant choice since fixation cannot compensate for poor alignment. When performed meticulously, osteosynthesis offers patients the invaluable reward of retaining their native hip.
References
- 1. Randelli F, Viganò M, Liccardi A, Mazzoleni MG, Basile G, Menon A, Cosmelli N. Femoral neck fractures: Key points to consider for fixation or replacement a narrative review of recent literature. Injury. 2023 Mar;54 Suppl 1: S70-S77. doi: 10.1016/j.injury.2021.09.024. Epub 2021 Sep 25. PMID: 34615597. [Google Scholar] [PubMed] [CrossRef]
- 2. Zhao D, Wang Z, Cheng L, et al. The Significance of Evaluating the Femoral Head Blood Supply after Femoral Neck Fracture: A New Classification for Femoral Neck Fractures. Orthop Surg. 2022;14(4):742-749. doi:10.1111/os.13241 [Google Scholar] [PubMed] [CrossRef]
- 3. Liang C, Cao Y, Lin Z, Liu G, Zhang C, Hu Y. Open reduction and internal fixation of irreducible displaced femoral neck fracture with femoral Neck System: a preliminary study. BMC Musculoskelet Disord. 2023;24(1):826. Published 2023 Oct 19. doi:10.1186/s12891-023-06839-3. [Google Scholar] [PubMed] [CrossRef]
- 4. Karanicolas PJ, Bhandari M, Walter SD, Heels-Ansdell D, Sanders D, Schemitsch E, Guyatt GH. Interobserver reliability of classification systems to rate the quality of femoral neck fracture reduction. J Orthop Trauma. 2009 Jul;23(6):408-12. doi: 10.1097/BOT.0b013e31815ea017. PMID: 19550226. [Google Scholar] [PubMed] [CrossRef]
- 5. Mukhopadhaya, J., Bhadani, J.S. (2023). Implantology of Fractures of the Neck of Femur. In: Banerjee, A., Biberthaler, P., Shanmugasundaram, S. (eds) Handbook of Orthopaedic Trauma Implantology. Springer, Singapore. https://doi.org/10.1007/978-981-19-7540-0_118 [Google Scholar] [PubMed] [CrossRef]
- 6. Filipov O. Biplane double-supported screw fixation (F-technique): a method of screw fixation at osteoporotic fractures of the femoral neck. Eur J Orthop Surg Traumatol. 2011 Oct;21(7):539-543. doi: 10.1007/s00590-010-0747-9. Epub 2011 Jan 5. PMID: 21966288; PMCID: PMC3178023. [Google Scholar] [PubMed] [CrossRef]
- 7. Della Rocca GJ. Gaps and opportunities in the management of the young femoral neck fracture. Injury. 2015 Mar;46(3):515-8. doi: 10.1016/j.injury.2014.11.015. Epub 2014 Nov 26. PMID: 25496856. [Google Scholar] [PubMed] [CrossRef]








