New minimal invasive technique can avoid many complications with the advantages of the anatomy and principle of the fixation system.
Dr. Sharon Rose Neerudi, Department of Orthopaedics, ESIC Medical College and Hospital, National Highway 65, Sanatnagar, Hyderabad - 500038, Telangana, India.E-mail: rosesharon832@gmail.com
Introduction: Plate osteosynthesis has traditionally been the preferred treatment for humeral shaft fractures requiring surgical intervention. However, plating involves an open approach, necessitating careful and meticulous handling of soft tissue. As a result, the anterior bridge plating (ABP) as minimally invasive plate osteosynthesis (MIPO) is emerging as a promising technique for managing humeral shaft fractures.We performed an analysis on both groups (40 patients each), and our primary objectives compared were radiological outcome, functional outcome using UCLA shoulder score Mayo elbow score, time period of union. Our secondary objectives were rate of infection, postoperative radial nerve palsy, surgical time, number of fluoroscopic shoots.
Material and Method: Eighty patients with humerus mid-shaft fractures which with inclusion criteria were randomly selected and divided into two groups. Group1(n= 40) patients were treated with MIPPO by ABP and group 2 (n = 40) with open reduction and internal fixation (ORIF).
Discussion: Most of the studies which have been done previously on this MIPO technique used Locking compression plate which showed good results, even when compared to intramedullary nailing and conventional plating. Using the Locking compression plate gives us confidence in terms of giving relative stability even in young patients with good bone stock. The unique feature of this study is the even Dynamic compression plate gives us good secure fixation with relative stability causing axial micro-movements at the fracture even in transverse fracture pattern.
Results: Eight patients were randomly selected by allotting them alternatively to each procedure, with 40 in each group. Group-1 patients are operated by Anterior Bridge Plating, Group-2 patients are operated by conventional posterior plating using DCP. Male to female ratio was 4:1 and the mean age group was 31-45 years. The most common type of fracture pattern seen was B2 type according to AO classification system. Group-1 (ABP) showed better results in terms of infection, post-operative radial nerve palsy, time period of union, time period of union and functional outcome. Yet, this also few shortcomings like long surgical time period with increased radiation exposure.
Conclusion: The MIPPO by ABP technique provides good results comparable to the ORIF method for all types of humeral shaft fractures. While this new technique may promote early union and better functional outcomes by minimising perioperative complications and soft tissue dissection, it also involves a significant amount of radiation exposure.
Keywords: Minimally invasive plate osteosynthesis (MIPPO), Anterior bridge plating (ABP), Open reduction and internal fixation (ORIF)
Humeral shaft fractures account for 1–3% of all the adult fractures with a reported annual incidence of 13–15/1 lakh persons [1,2]. Treatment options range from conservative options,such as functional bracing to plate fixation (via anterior, posterior, or anterolateral approaches) or intramedullary nailing (antegrade).Despite multiple options, no gold standard exists[2,3]. While non-operative methods, particularly functional bracing, have been effective in selected cases due to the humerus’s ability to tolerate displacement, surgery is gaining favor for its benefits of early mobilization and fewer immobilization-related complications.Functional bracing, dating back to ancient Egypt[4], stabilizes the fracture through soft tissue compression and allows joint movement, promoting healing while preventing stiffness[5].Surgical fixation, especially plate fixation and intramedullary nailing, offers faster recovery but comes with technical considerations[6]. Biological fixation, minimizing soft tissue disruption while maintaining stability,has become more popular, though its superiority is still debated[7].Minimally invasive plate osteosynthesis (MIPO) using the anterolateral bridge plating (ABP) method, have shown promising outcomes[8,9]. MIPO by ABP avoids radial nerve exposure, reduces soft tissue trauma, and may speed up healing compared to conventional plating, particularly the posterior approach that requires radial nerve exposure [8,9,10]. Although, a long locking compression plate (LCP) is used for ABP routinely [10], we hypothesized that a longer dynamic compression plate (DCP) in bridge mode will also yield functionally good outcomes in non-osteoporotic bones. In this study, we compared prospectively the outcome of humerus shaft fractures treated by open reduction and internal fixation (ORIF) with DCP and by ABP with DCP.
Study Design: The demographic and fracture characteristics of the two treatment groups were compared using the Chi square test or Fisher’s exact test for nonparametric categorical variables or using the Student’s t test for parametric variables. Operative time and the union time were compared using the Student’s t test and complications using Fisher’s exact test. This is a prospective comparative study that was conducted at our institute (IEC Approval No – ESICMC/SNR/IEC/S0172/07-2022), where patients with fractures of humerus shaft in age group of 18 to 65 years were admitted for surgical fixation during August 2022 to February 2024. The Sample size was calculated with Formula used: n=1+2C(SD/d)2 =80, with 40 in each group. Convenient sampling was chosen for this study until 40 patients were included in each of the treatment groups. Patients were divided in to two groups by simple randomisation (SNOSE method), where in one group was operated by ABP with DCP and other group was operated by ORIF with DCP fixation. A pieces of paper with the treatment allocation (named as ORIF and ABP) are placed inside an opaque envelope and sealed. The envelopes are then sequentially numbered, and the recruiting clinician opens them in order as new participants enrol. The treatment assignment inside the envelope is revealed to the clinician and is used for the participant. The envelope is assigned a sequential number, and the treatment assignment is kept hidden until the trial is over. It is double blinded study. This is how allocation is concealed. Patients with mid-shaft humerus fracture located atleast 60 mm distal to surgical neck and 60mm proximal to olecranon fossa in the age group of18-65 years and who consented to participate in the study are included. Patients with compound Grade3C[Gustilo-Anderson Classification], suspected pathological fractures and those with radial nerve and vascular Injuries are excluded from the study. The intervention was done based on the allocated procedure as described below. The operated arm was immobilised in armsling/shoulder immobiliser for 24 hours.
- Checked neurovascular status post
- Only elbow Range of motion [ROM]is
- Wound inspection done on the second
- Suture removal on postoperative day 14
- Shoulder ROM is
- Check x-rays are taken on monthly interval to check for
Patients are followed every monthly to assess clinically and radiologically up to the period of one year. Functional assessment is done by using shoulder UCLA score and MAYO elbow score. All patients are assessed every monthly and both scores – UCLA and Mayo elbow scores were calculated at each visit. The variables which were assessed – period of radiological union, functional outcome, non-union, infection rate, radial nerve palsy rate, surgical time and number of fluoroscopy shoots. The demographic and fracture characteristics of the two treatment groups were compared using the Chi square test. Operative time and the using the Student’s t test and complications using Fisher’s exact test.
Surgicalprocedure
ABP Technique :
After thorough evaluation and the workup of the patients and under Regional or general anaesthesia, patient was placed in supine with arm abducted about 60 degrees with injured arm on radiolucent arm board an acceptable alignment was achieved, and approximate length of the plate (10-12 holed) was determined and both proximal and distal incisions were marked under C arm intensifier. A 3-5cm long incision on the upper metaphysis of the Humerus was made. The soft tissues were dissected bluntly to reach the bone. The 3-5 cm distal incision was made and with blunt dissection the bone in distal metaphysis was reached lateral border of biceps brachii 2 cm above the elbow crease with flexion of elbow joint to relax biceps brachii (Figure-1).

Figure 1: Incisions for proximal and distal windows.
The inter-nervous plane in Proximal window is between axillary nerve (deltoid) & medial & lateral pectoral nerves (pectoralis major) and in the Distal part is between Musculo-cutaneous & Radial nerve (medial & lateral ½ of brachialis). The anatomical plane is proximally lateral to the tendon of long head of biceps & detached the insertions of pectoralis major & part of deltoid. Distally identify the plane between biceps & brachialis,by retracting biceps medially, a split was made in the midline of brachialis longitudinally to develop an epi- periosteal plane. Lateral ante-brachial cutaneous nerve was protected. Forearm was placed insupinated to protect radial nerve. The sub muscular epi-periosteal plane developed at distal incision site is developed proximally using a blunt periosteal retractor, thereby connecting the two windows (Figure- 2a, b).

Figure 2: Periosteal plane was developed on anterior surface of humerus and connected the two windows.
A 10-12 holed 4.5mm Narrow Dynamic compression plate (DCP) was inserted through the proximal window & proximal segment of the plate was aligned with the anterior surface of Humerus shaft. Proximally one screw was inserted (Figure-3-4) and the fracture is manipulated and reduced
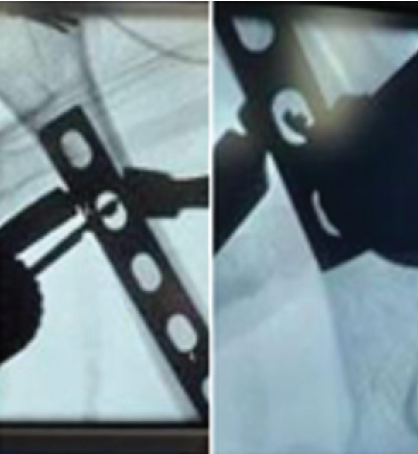
Figures3: Proximal and distal but one screws are inserted first.

Figure 4: Final reduction images, wound closure.
under c-arm guidance. Then distal most screw was inserted. Finally, four more screws – 2 proximal and 2 distal were inserted depending on the access through the surgical incision window. Arm sling pouch was given and elbow range of motion was started immediately, shoulder motion was started at 2 weeks. Case follow-up radiological and clinical images- Figures 5-8. Fluoroscopy shoots are taken frequently during this procedure to confirmed the placement of the plate (equidistant from the fracture and maintain the working length), reduction of the fracture site and screw length.

Figure 5: Anterior bridge plating.10 months postoperative.

Figures 6: Clinical images showing shoulder and elbow rom.
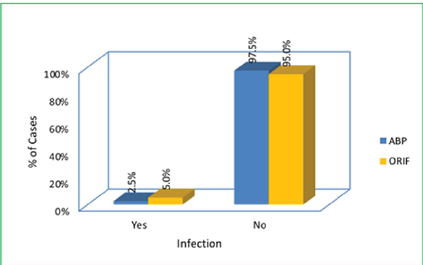
Figure7: Rate of infection: Infection rate in both groups.
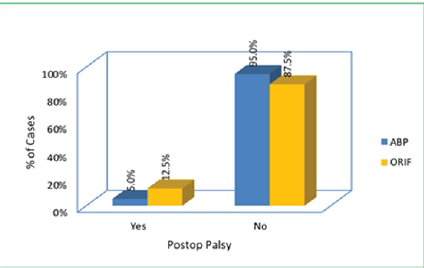
Figure 8: Post-operative radial nerve palsy rate in this study.
ORIF with DCP Plating : Conventional Anterolateral approach or a posterior approach was used to reduce fracture by open reduction and then an adequate sized DCP plate was used to stabilise it with at least 7-8 screws.
Patients are followedevery month to assess clinically and radiologically up to 1 year.Functional assessment was done by using shoulder UCLA score and MAYO elbow score.The variables which were assessed are period of radiological union, functional outcome, non-union, infection, Radial nerve palsy, range of motion (flexion, extension. Abduction, adduction, internal and external rotations). The need of fluoroscopy is less comparatively as the fracture reduction, its stability and plate placement are visible with naked eye and shoots are taken rarely just to confirm the screw length.
Statistical analysis
The demographic and fracture characteristics of the two treatment groups were compared using the Chi-square test.Operative time and the use of the Student’s t-test and complications using Fisher’s exact test.
Eighty patients were taken in this study who had Humerus mid-shaft fractures. They were divided into two groups. In ABP group, only 1 case showed superficial infection, whereas in ORIF group,2 cases showed infective non-union. 2 cases of group-1 and 5 cases of group-2 had postoperative radial nerve palsy which all of them recovered spontaneously. Hence, the rate of palsy is more with ORIF group which is significant [p-value<0.5]. One case of ABP resulted in non-union whereas two cases of ORIF showed nonunion due to infection, out of which one case went through grafting and the other case was lost in follow-up (Table 1).We studied that the range of motion at shoulder joint is more with ABP group comparatively as the p-values are significant more with flexion, extension, abduction, internal rotation and external rotation. Out of 40 cases of ABP, 19 cases showed score34, 10 cases showed 33,10 cases-32,1case showed 30.Outof 40 case s ORIF, 10 cases showed 34, 7-33, 9-32, 2-28, 1-24, 1-22. Because of less soft tissue dissection, ABP shows good shoulder outcome (p-value<0.05) (Table-2).In ABP group, 24cases showed 100,1-98,1-975.InORIFgroup,21cases showed100,15-95,3-90,1-85. Hence, ABP shows better elbow outcome than ORIF cases (Table-3).ABP cases shows early radiological union comparatively{12weeks-mean} with p-value<0.05 (Table-4).The surgical time is more with ABP since it is a closed reduction method (Table-5). The mean number of c-arm shoots was 104.28 in Group-1 and 8.05 in group-2. There was no difference in the outcome when compared to age, sex, side or obesity.
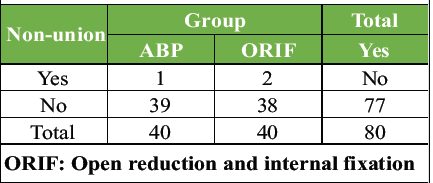
Table 1:Non-union rate inthis study
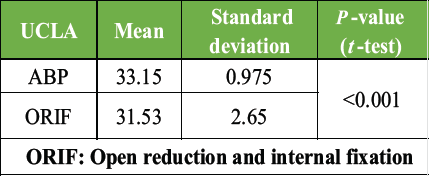
Table 2:UCLA scoring in this study
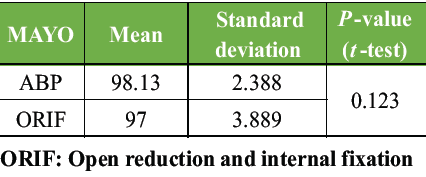
Table 3: Mayo scoring in this study
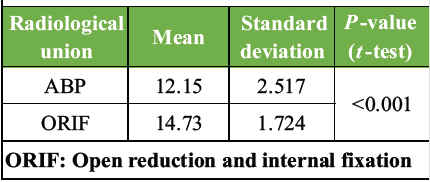
Table 4:Radiological time period in this study
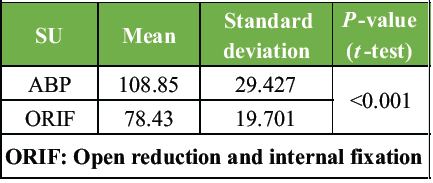
Table 5:Surgical time in this study
ENROLLMENT Assessed for eligibility (n=80)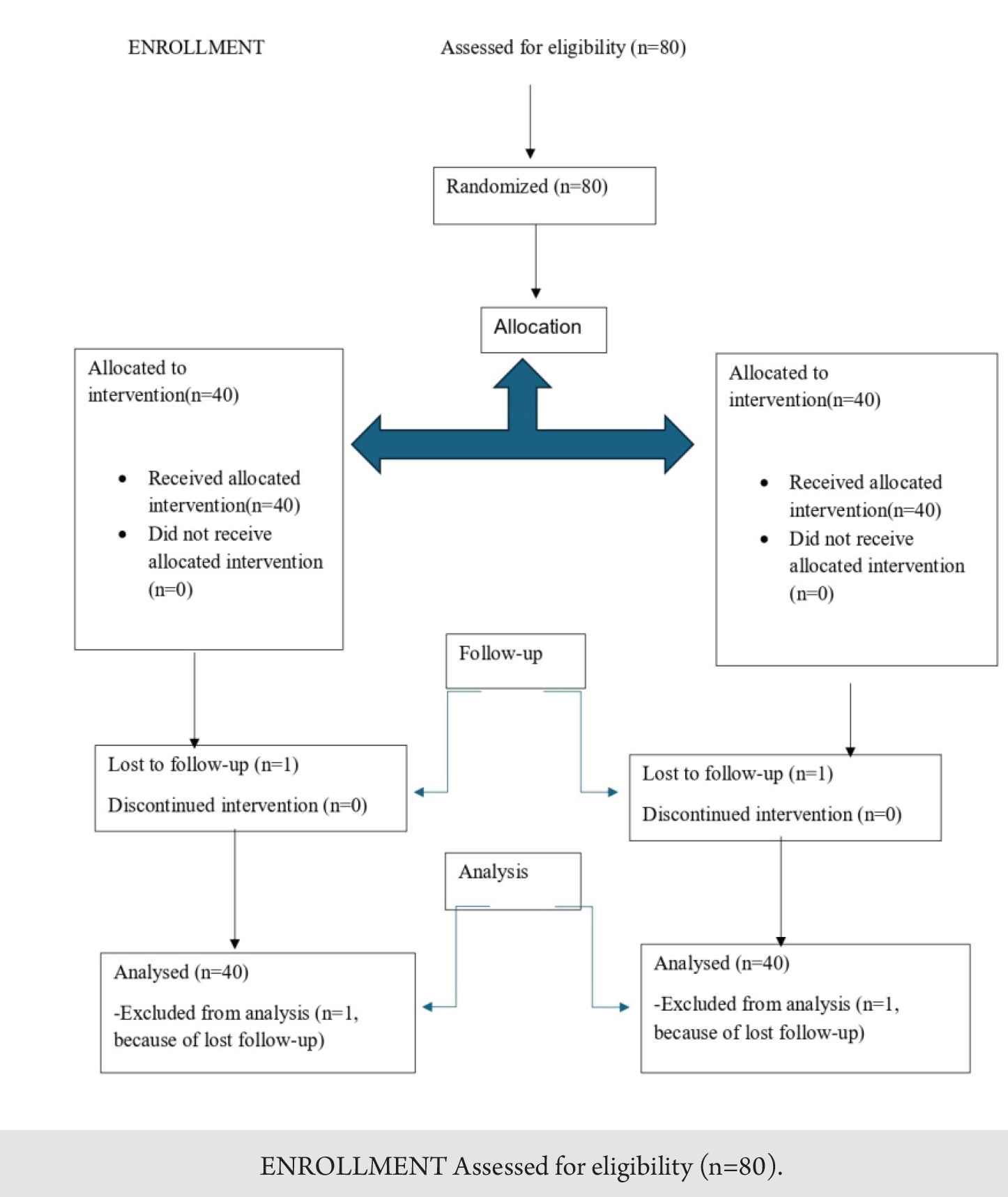
Anterior bridge plating (ABP) has emerged as a reliable, minimally invasive option for managing humeral shaft fractures. While the LCP has traditionally been favored due to its biomechanical strength and compatibility with MIPO principles, recent evidence – including findings from this study – supports the use of DCPs as a cost-effective and clinically comparable alternative. This study demonstrates that DCP, when used in ABP, can yield satisfactory radiological and functional outcomes, aligning with earlier research on the technique’s efficacy. Despite technical challenges, such as indirect fracture visualization and difficulty in plate positioning, procedural adjustments – such aselbow flexion during fluoroscopy – can mitigate these issues. The reduced operative time and lower implant cost make DCP a viable choice, particularly in resource-limited settings. Multiple studies support the clinical value of ABP. Kumar et al. noted early return to function with minimal soft tissue disruption [11]. Similarly, in our study, 2 cases of ORIF resulted in infection which were eventually ended non- union. 2 cases of ABP showed superficial infection which was subsided with antibiotics and implant removal after fracture was united completely (5-6 months) due to minimal soft tissue disruption.
Thakor et al. highlighted the construct’s ability to withstand biomechanical stresses through relative stability[12]. Hence in our analysis, ABP cases had radiological union by 12.75 weeks (mean)and ORIF cases had by 14.75 weeks (mean). Even though there is absolute stability in conventional method, ABP showed less time period of time. Yang’s comparison of MIPO and ORIF favoured ABP for its superior safety and functional outcomes [13], and Bhandra et al. confirmed its safety in straightforward fracture patterns when performed by experienced surgeons [14]. In our study, mean UCLA shoulder score was 33.15 in ABP and 31.53 in ORIF. The mean Mayo elbow score was 98.13 in ABP and 97 in ORIF. Therefore, the functional outcome is better in ABP group similarly to the previous studies. Anatomical safety remains paramount. Apivatthakakul et al. identified high-risk zones for nerve injury during screw placement, emphasizing the need for precise technique [15]. Suwannaphisit et al. further demonstrated the variability in radial nerve anatomy, underlining the importance of preoperative planning and intraoperative vigilance [16]. 5 cases of ORIF and 2 cases of ABP showed postop radial nerve palsy in our research. All of them recovered spontaneously. The reason to have radial nerve palsy in ABP is because not having knowledge about the precise location of radial nerve and it varies in each individual and may have anatomical anomalies, and uncontrolled drilling where the drill bit can hit the nerve posteriorly. ABP preserves periosteal blood supply, limits soft tissue disruption, and allows micromotion conducive to callus formation—all factors that support fracture healing and reduce complications such as infection and non-union. Although technically demanding, ABP with DCP represents a promising and practical alternative to traditional plating methods, especially when performed by skilled surgeons. This study is a reliable research as it covers a good sample in both groups with no sexual bias and the most common age group and followed the cases for the period of 1year. However, it doesn’t include the elderly population where DCP cannot be used, doesn’t include post-traumatic radial nerve palsy (GA-3C with wrist drop), as whether ABP does not involve radial nerve exploration or the need of exploration is a must, as most of them are conserved in all types of nerve injury except in transection. These are its limitations and a meta-analysis should be done, which can include all types of open fractures with and without radial nerve palsy or should be studied alone.
This study compares the outcomes of humeral diaphysis fractures treated with minimally invasive plate osteosynthesis (MIPPO) using anterior bridge plating (ABP) with dynamic compression plates (DCP) to open reduction and internal fixation (ORIF) with DCP. Both groups achieved favorable clinical outcomes at one-year follow-up, confirming the overall effectiveness of DCP in fracture management. This study evaluated key clinical and surgical outcomes in the management of humeral shaft fractures, focusing on period of radiological union, functional recovery, and complication rates. Primary endpoints included time to radiological union and postoperative functional outcomes. Secondary measures assessed the incidence of non-union, infection, and radial nerve palsy. Operative efficiency was examined through analysis of surgical duration and number of intraoperative fluoroscopy shots. The findings provide a comparative overview of healing patterns, functional performance, complication profiles, and technical demands associated with the studied intervention. Additionally, the study highlights the economic viability of using DCP in ABP-MIPO as a cost-effective alternative to locking compression plates, especially in resource-limited settings. Overall, the findings support broader adoption of ABP-MIPO with DCP for humeral shaft fractures, promoting a shift toward techniques that offer both clinical efficacy and economic accessibility.
Minimally invasive Anterior Bridge technique is a new evolving technique and can be done using DCP which can serve its purpose while giving relative stability in young and good healthy bones with less soft tissue dissection.
References
- 1. Ekholm R, Adami J, Tidermark J, Hansson K, Tornkvist H, Ponzer S. Fractures of the shaft of the humerus. An epidemiological study of 401 fractures. J Bone Joint Surg Br 2006;88:1469-73. [Google Scholar] [PubMed]
- 2. Mattila H, Keskitalo T, Simons T, Ibounig T, Rämö L. Epidemiology of 936 humeral shaft fractures in a large Finnish trauma center. J Shoulder Elbow Surg 2023;32:e206-15. [Google Scholar] [PubMed]
- 3. Gosler MW, Testroote M, Morrenhof JW, Janzing HM. Surgical versusnon surgical interventions for treating humeral shaft fractures in adults. Cochrane Database Syst Rev 2012;1:CD008832 [Google Scholar] [PubMed]
- 4. Van Bergen SH, Mahabier KC, Van Lieshout EM, Van der Torre T, Notenboom CA, Jawahier PA, et al. Humeral shaft fracture: Systematic review of non-operative and operative treatment. Arch Orthop Trauma Surg 2023;143:5035-54. [Google Scholar] [PubMed]
- 5. Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am 2000;82:478-86. [Google Scholar] [PubMed]
- 6. Lotzien S, Hoberg C, Rausch V, Rosteius T, Schildhauer TA, Gessmann J. Open reduction and internal fixation of humeral midshaft fractures: Anterior versus posterior platefixation. BMC Musculoskelet Disord 2019;20:527. [Google Scholar] [PubMed]
- 7. Walker M, Palumbo B, Badman B, Brooks J, VanGelderen J, Mighell M. Humeral shaft fractures: A review. J Shoulder Elbow Surg 2011;20:833-44. [Google Scholar] [PubMed]
- 8. Heineman DJ, Poolman RW, Nork SE, Ponsen KJ, Bhandari M. Platefixation orintramedullary fixation of humeral shaft fractures: Anupdatedmeta- analysis. Acta Orthopaedica 2010;81:216-23. [Google Scholar] [PubMed]
- 9. Sharma G,Shah A,Chhallani A,Kadam R,Asawa T, Anbalaganl PK. Mid-term outcome of minimally invasive anterior bridge plating versus conventional posterior plating for diaphyseal fracture humerus- a prospective randomized trial. J Orthop Trauma Surg Rel Res 2021;16(12):16-21. [Google Scholar] [PubMed]
- 10. Esmailiejah AA, Abbasian MR, Safdari F, Ashoori K. Treatment of humeral shaft fractures: Minimally invasive plate osteosynthesis versus open reduction and internal fixation. Trauma Mon 2015;20:e26271. [Google Scholar] [PubMed]
- 11. Dey JK, Shetty SH, Singh SD, Srivastava A, Agrawal S, Modi RR, et al. Prospective study of radiological and functional outcomes of humeral mid-shaft fractures by anterior bridge plating technique. Int J Res Orthop 2023;9:245-9. [Google Scholar] [PubMed]
- 12. Thakor PP, Sabharish Reddy SC, Dodamni SM. Functional and clinical outcome of minimally invasive anterior bridge platting in humerus shaft fractures. Int J Orthop Sci 2023;9:314-8. [Google Scholar] [PubMed]
- 13. Yang J, Liu D, Zhang L, Lu Z, Liu T, Tao C. Treatment of humeral shaft fractures: A new minimally-invasive plate osteosynthesis versus open reduction and internal fixation: A case control study. BMC Surg 2021;21:349. [Google Scholar] [PubMed]
- 14. Bhandara PV, Devkate S, Gaikwad Y. Functional outcome of submuscular plating for diaphyseal long bone fractures. Indian J Orthop Surg 2020;6:103-10. [Google Scholar] [PubMed]
- 15. Apivatthakakul T, Patiyasikan S, Leuvitoonvechkit S. Danger zone for locking crew placement inminimally invasive plate osteosynthesis of humerus shaft fractures. Indian J Care Injured 2010;41:169-72. [Google Scholar] [PubMed]
- 16. Suwannaphisit S, Aonsong W, Suwanno P, Chuaychoosakoon C. Location of the radial nerve along the humeral shaft between the prone and lateral decubitus positions at different elbow positions. Sci Rep 2021;11:17215. [Google Scholar] [PubMed]