Schwannoma should be suspected in long-standing, localized, tender swellings around the knee, particularly when imaging and clinical features do not correlate with more common benign lesions such as ganglion cysts.
Dr. Hunaid Haider, Department of Orthopaedics, Seth G.S. Medical College and KEM Hospital, Mumbai, Maharashtra, India. E-mail: hzhad98@gmail.com
Introduction: Schwannomas are benign, encapsulated peripheral nerve sheath tumors derived from Schwann cells. They are rarely seen around the knee, accounting for <1% of all schwannomas, and can mimic other benign swellings such as ganglion cysts or bursae.
Case Report: We report a 32-year-old female who presented with anteromedial right knee pain and a tender swelling for 2 years. Radiographs were normal, and a provisional diagnosis of a ganglion cyst was made. The lesion was excised under local anesthesia through a vertical incision and found to be a well-encapsulated mass measuring approximately 1 × 1 × 1 cm, located superficial to the joint capsule. Based on its location, the swelling was suspected to arise from a branch of the saphenous nerve, most likely the infrapatellar branch. Histopathological examination confirmed the diagnosis of schwannoma.
Conclusion: Schwannomas, though benign and uncommon around the knee, should be included in the differential diagnosis of localized knee pain with soft-tissue swelling and normal radiographs.
Keywords: Anterior knee pain, ganglion cyst, schwannoma.
Schwannomas, also known as neurilemmomas, are non-malignant and typically slow-growing tumors that originate from Schwann cells – the specialized cells responsible for forming the myelin sheath surrounding peripheral nerves. These lesions develop eccentrically along the course of peripheral nerves and remain encapsulated, allowing for clear distinction from surrounding tissues. Although they can arise in any part of the body containing peripheral nerves, schwannomas represent only a small fraction of benign soft-tissue tumors, accounting for roughly 5% of all such cases reported in clinical practice [1,2]. Most schwannomas occur in the head, neck, and flexor aspects of the upper limbs. Lesions around the knee are extremely rare representing <1% of all schwannomas and usually originate from sensory branches of the saphenous or tibial nerves [3,4]. Due to their rarity and non-specific presentation, schwannomas of the knee are often misdiagnosed as ganglion cysts, lipomas, or bursae. This report describes a schwannoma arising from the infrapatellar branch of the saphenous nerve presenting as chronic anteromedial knee pain.
A 32-year-old female presented with dull, aching pain and a swelling over the anteromedial aspect of the right knee for 2 years. The swelling was gradually progressive such that initially it was just palpable to now having grown to the size of a pea, with tenderness and discomfort during kneeling. There was no contributing history like that of trauma, fever, or constitutional symptoms.
Examination
A small, well-defined, firm swelling was noted over the anteromedial aspect of the right knee, superficial to the joint line. It was tender, mobile transversely, and not adherent to the skin. Overlying skin was normal, and knee range of motion was full and painless. There were no neurological deficits.
Investigations
Plain radiographs were unremarkable. No ultrasound or MRI was performed initially. Based on the clinical findings, a ganglion cyst was suspected.
Procedure
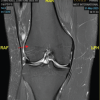
Under local anesthesia, a vertical incision was made over the swelling (Fig. 1).
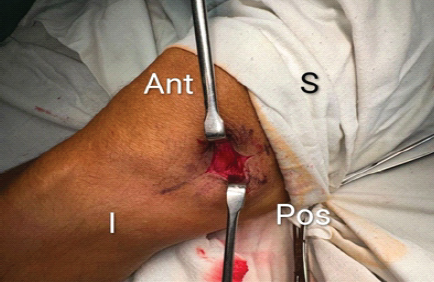
Figure 1: A vertical incision was taken on the anteromedial aspect of the right knee directly over the swelling.
A well-encapsulated, reddish-white mass measuring approximately 1 × 1 × 1 cm (Fig. 2) was identified superficial to the joint capsule, in the natural course of a cutaneous branch of the saphenous nerve, likely the infrapatellar branch. The lesion was excised in toto and sent for histopathological evaluation (Fig. 3).
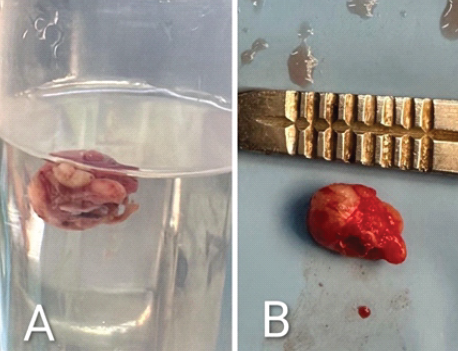
Figure 2: (a) Excised swelling in formalin container, (b) Excised swelling approx side of 1 × 1 × 1 cm.
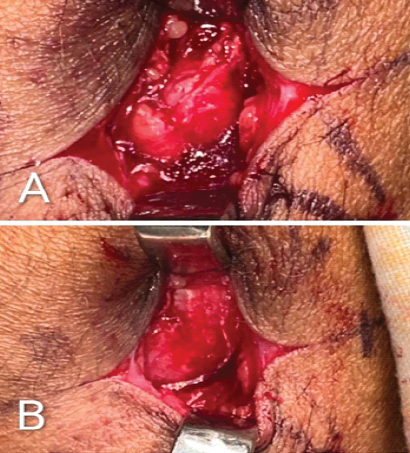
Figure 3: (a) Swelling seen after incision, (b) After removal of swelling capsule seen.
Histopathological findings
Histopathological examination revealed a well-circumscribed, encapsulated neoplasm composed of two distinct histologic patterns. The first pattern, corresponding to Antoni A areas, displayed compact, spindle-shaped cells arranged in interlacing fascicles with prominent nuclear palisading, forming characteristic Verocay bodies. The second pattern, known as Antoni B areas, showed a more loosely organized, hypocellular architecture with myxoid stroma and scattered cells. These microscopic features were characteristic of a benign peripheral nerve sheath tumor, confirming the diagnosis of schwannoma (Fig. 4).
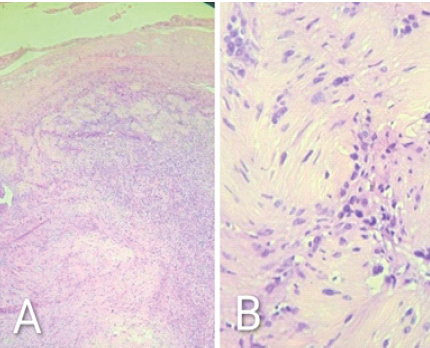
Figure 4: (a) 10× – microscopy shows encapsulated spindle cell neoplasm with Antoni A and B areas (b) 100× – Characteristic Verocay bodies are seen.
Outcome
The post-operative period was uneventful, and the patient experienced complete relief of pain and tenderness. At six months follow-up, there was no recurrence, and full knee function was restored (Fig. 5).

Figure 5: Anteroposterior and lateral images of the suture site.
Schwannomas are benign peripheral nerve sheath tumors that grow eccentrically to the parent nerve, displacing rather than infiltrating nerve fibers [5,6]. They are encapsulated, solitary, and slow-growing. In the lower limb, the tibial and peroneal nerves are most commonly affected, while schwannomas arising from the infrapatellar branch of the saphenous nerve are exceedingly rare [7]. Their rarity (<1% of schwannomas) and small size often lead to misdiagnosis. Clinically, they present as firm, tender swellings with localized pain but minimal neurological deficit.
Differential diagnoses for anteromedial knee swellings include:
- Ganglion cyst
- Synovial or pes anserine bursitis
- Lipoma
- Fibroma
- Neurofibroma
- Hemangioma
- Epidermoid cyst
- Soft-tissue sarcoma (rare)
Imaging
MRI is the investigation of choice, revealing a well-circumscribed lesion with low T1 and high T2 signal intensity and sometimes a characteristic “target sign” [8]. In this case, due to clinical similarity with a ganglion cyst, the diagnosis was only confirmed postoperatively.
Definitive management and recurrence
The standard treatment is complete surgical excision with preservation of the parent nerve. Because schwannomas are encapsulated and eccentric, they can usually be removed without neurological compromise [9]. Recurrence is rare and generally associated with incomplete excision. Malignant transformation is extremely uncommon [10]. Post-operative outcomes are excellent, and patients typically achieve complete symptom relief. Follow-up for 12–24 months is recommended to rule out recurrence.
This case report throws light on the importance of considering schwannoma in the differential diagnosis of chronic, localized anteromedial knee pain, particularly when imaging is normal, and the lesion mimics more common benign cystic swellings. Although schwannomas account for <1% of all cases around the knee, even small superficial lesions arising from the infrapatellar branch of the saphenous nerve can cause significant pain. This case holds clinical relevance for orthopedic surgeons, musculoskeletal oncologists, and general practitioners. It underscores the need for vigilance in atypical soft-tissue swellings, the value of histopathological confirmation, and the effectiveness of simple excision under local anesthesia as definitive management. By adding to the limited literature on infrapatellar schwannomas, this report enhances understanding of their clinical presentation, diagnostic challenges, and surgical outcomes, contributing to improved recognition and management of rare nerve sheath tumors.
Chronic, localized anteromedial knee pain associated with a small tender swelling – even with normal radiographs – should alert clinicians to the possibility of a peripheral nerve sheath tumor such as a schwannoma. Early suspicion and simple excision can ensure a complete cure and prevent prolonged misdiagnosis.
References
- 1. Kransdorf MJ. Benign soft-tissue tumors in a large referral population: distribution of specific diagnoses by age, sex, and location. AJR Am J Roentgenol. 1995 Feb;164(2):395-402 [Google Scholar] [PubMed]
- 2. Adani R, Baccarani A, Guidi E, Tarallo L. Schwannomas of the upper extremity: diagnosis and treatment. Chir Organi Mov. 2008 Sep;92(2):85-8. [Google Scholar] [PubMed]
- 3. Kang HJ, Shin SJ, Kang ES. Schwannomas of the upper extremity. J Hand Surg Br 2000;25:604-7. [Google Scholar] [PubMed]
- 4. Oberle J, Kahamba J, Richter HP. Peripheral nerve schwannomas–an analysis of 16 patients. Acta Neurochir (Wien) 1997;139:949-53. [Google Scholar] [PubMed]
- 5. Debs P, Luna R, Fayad LM, Ahlawat S. MRI features of benign peripheral nerve sheath tumors: how do sporadic and syndromic tumors differ? Skeletal Radiol. 2024 Apr;53(4):709-723. [Google Scholar] [PubMed]
- 6. Kim DH, Murovic JA, Tiel RL, Moes G, Kline DG. A series of 397 peripheral neural sheath tumors: 30-year experience at Louisiana State university health sciences center. J Neurosurg 2005;102:246-55. [Google Scholar] [PubMed]
- 7. Cherraqi A, El Haddad S, Messaoud O, Andour H, Tbouda M, El Ansari N, Kili A, Hessissen L, Allali N, Chat L. Saphenous Nerve Schwannoma: A Rare Differential Diagnosis of Knee Pain in Children. Glob Pediatr Health. 2023 Feb 17;10:2333794X231156047 [Google Scholar] [PubMed]
- 8. Beaman FD, Kransdorf MJ, Menke DM. Schwannoma: Radiologic-pathologic correlation. Radiographics 2004;24:1477-81. [Google Scholar] [PubMed]
- 9. Knight DM, Birch R, Pringle J. Benign solitary schwannomas: A review of 234 cases. J Bone Joint Surg Br 2007;89:382-7. [Google Scholar] [PubMed]
- 10. Zhang H, Cai C, Wang S, Liu H, Ye Y, Chen X. Extracranial head and neck schwannomas: a clinical analysis of 33 patients. Laryngoscope. 2007 Feb;117(2):278-81. [Google Scholar] [PubMed]