Screwless press-fit acetabular cups can provide reliable early stability in uncemented total hip arthroplasty and allow safe early full weight-bearing with good short-term outcomes.
Dr. Indrajeet Kumar, Department of Orthopaedics, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India. E-mail: indrajeet98ortho@gmail.com
Introduction: Total hip arthroplasty (THA) remains one of the most effective surgical interventions for advanced hip pathology, providing reliable pain relief and functional restoration. Despite widespread use, outcomes from different regions and clinical settings continue to be valuable for benchmarking the quality of care.
Materials and Methods: A prospective observational study was conducted in the department of orthopedics at a tertiary care center in eastern India. Thirty adult patients undergoing uncemented THA for various hip pathologies were enrolled. All procedures were performed using a porous press-fit acetabular cup through the modified Hardinge approach. Perioperative parameters, radiographic findings, and functional outcomes, including the Harris Hip Score (HHS), were recorded. Patients were followed at 1, 3, 6, and 12 months. One patient was lost to follow-up.
Results: Among the 30 patients, 24 (80%) were male, and 6 (20%) were female. Primary indications included osteoarthritis secondary to avascular necrosis (16; 53.33%), post-traumatic arthritis (10; 33.33%), rheumatoid arthritis (3; 10%), and corticosteroid-induced arthritis (1; 3.33%). The mean pre-operative HHS was 43.33 ± 10.8, categorized as poor. The average operative duration was 87.23 min (range: 60–135), with a mean intraoperative blood loss of 388.67 mL (range: 220–820). Radiographically, none of the 29 evaluated patients demonstrated component loosening in either the acetabular or femoral zones at any follow-up interval (1, 3, 6, or 12 months). Functional outcomes showed statistically significant improvement: mean HHS increased to 80.97 ± 5.1 at 1 month, 86.07 ± 4.0 at 3 months, 90.42 ± 2.9 at 6 months, and 92.59 ± 2.7 at 12 months (P < 0.001 for all comparisons).
Conclusion: Uncemented THA using a porous press-fit acetabular cup demonstrated excellent early outcomes, with no evidence of component migration or osteolysis during 1-year follow-up. Patients experienced significant and sustained improvement in functional scores, with no major complications reported.
Keywords: Press-fit acetabular cup, uncemented total hip arthroplasty, screwless fixation, avascular necrosis, osteoarthritis hip, eastern India, modified Hardinge approach.
Total hip arthroplasty (THA) is among the most successful orthopedic procedures for managing degenerative joint disease and post-traumatic hip pathology. In uncemented THA, the stability and long-term survival of the acetabular component play a crucial role in overall implant performance. Press-fit acetabular cups have gained widespread acceptance because their porous-coated surfaces enable biological fixation through bone ingrowth [1,2]. Traditionally, adjunctive screw fixation was used to enhance primary stability, particularly in cases with compromised bone quality. However, with advances in implant design and surface engineering, the necessity of screws has become increasingly debated. Biomechanical evidence demonstrates that correctly reamed hemispherical cups can provide adequate initial stability without screw augmentation [3,4]. Clinical studies and systematic reviews further support this, reporting comparable radiological stability, migration rates, survivorship, and functional outcomes between screw-assisted and screwless press-fit cups [5,6,7]. At the same time, the use of screws introduces potential risks, including neurovascular injury, increased operative time, and screw-track osteolysis due to fluid ingress at the implant–bone interface [8,9]. Modern porous metal technologies and bioactive coatings such as hydroxyapatite (HA) have further strengthened the rationale for screwless cup fixation by improving implant–bone integration and frictional stability [10,11]. The present study aims to evaluate the safety and clinical outcomes of early full weight-bearing following uncemented THA using a screwless press-fit acetabular cup, focusing on radiological stability and functional recovery during short-term follow-up.
Study design and patient selection
This prospective observational study was conducted at a tertiary care center in eastern India after approval from the Institutional Ethics Committee (IEC No. 373/IEC/2021, dated December 13, 2021). Patients aged 20–60 years undergoing primary THA for various etiologies were eligible for inclusion. Exclusion criteria were pathological fractures, metabolic bone disorders, active infection, or refusal to provide informed consent. All patients underwent standardized pre-operative clinical evaluation, laboratory testing, and radiological assessment in accordance with the institutional THA protocol.
Implant specifications
All patients received a cementless, proximally HA-coated femoral stem paired with a porous, hemispherical, titanium press-fit acetabular cup. The acetabular cup was manufactured with a high-friction, porous surface to promote bone ingrowth and enhance primary stability. Device trade names are not disclosed in accordance with institutional anonymization policy; complete implant identifiers are provided to the journal editor upon request.
Surgical technique
All surgeries were performed by a single senior surgeon using the Modified Hardinge approach with the patient in the lateral decubitus position. After exposure, the acetabulum was sequentially reamed to achieve a peripheral rim fit. In patients with normal bone quality, the acetabulum was typically under-reamed by approximately 1 mm relative to the final cup size to achieve an optimal press-fit. In cases exhibiting softer bone or acetabular defects, reaming was adjusted pragmatically to prioritize secure peripheral rim contact rather than a fixed numerical under-reaming target. No screws were used in any patient for cup fixation. The femoral canal was prepared using standard broaching techniques, ensuring axial and rotational stability before inserting the cementless HA-coated stem. Trial components were used to confirm stability, impingement-free range of motion, and leg length before final implantation.
Post-operative care and rehabilitation
All patients underwent an immediate post-operative anteroposterior pelvis radiograph on post-operative day 1 to confirm component positioning. Supervised physiotherapy began on day 1, including bed mobilization, isometric strengthening, and assisted sitting/standing. Full weight-bearing as tolerated was initiated on post-operative day 2 following radiographic confirmation of satisfactory implant seating. A standardized rehabilitation protocol was followed for all patients, incorporating gait training with a walker or crutches, progression to a cane based on physiotherapist assessment, and routine outpatient physiotherapy after discharge. Deep vein thrombosis prophylaxis consisted of mechanical compression devices and pharmacologic agents per institutional guidelines.
Clinical evaluation
Follow-up assessments were performed at 1, 3, 6, and 12 months postoperatively. Functional outcomes were assessed using the Harris Hip score (HHS). Any post-operative complications or re-interventions were documented.
Radiographic assessment
Standardized anteroposterior pelvic radiographs were obtained at each follow-up visit. Radiographs were independently reviewed by two senior orthopedic consultants who were blinded to clinical outcomes. Acetabular component stability was assessed using the DeLee and Charnley classification for radiolucent lines [12], while femoral component evaluation used Gruen zones [13,14]. Component migration, inclination angle, and the presence of polar gaps were also recorded. In cases of discrepancy between the two readers, images were re-evaluated jointly and resolved by consensus. Inter-observer agreement was quantified using Cohen’s kappa for categorical variables (presence of radiolucent lines and zone involvement) and intraclass correlation coefficient (ICC) for continuous variables (acetabular inclination and migration). These statistics are reported in the results section and the Appendix.
Patient demographics and baseline characteristics
A total of 30 patients (24 males and 6 females) underwent uncemented THA using screwless press-fit acetabular cups. One patient was lost to follow-up after the 3-month evaluation; hence, final 12-month results are reported for 29 patients (Fig. 1). Mean age was 39.3 years (range: 22–55). The majority were aged 31–50 years (60%) with male-to-female ratio 4:1. Majority of the cases, 16 (53.33%) were of osteonecrosis due to avascular necrosis (AVN) of femoral head, 10 (33.33%) were post-traumatic, 3 (10%) were secondary to rheumatoid arthritis and 1 (3.33%) was secondary to use of corticosteroid for prolonged duration.
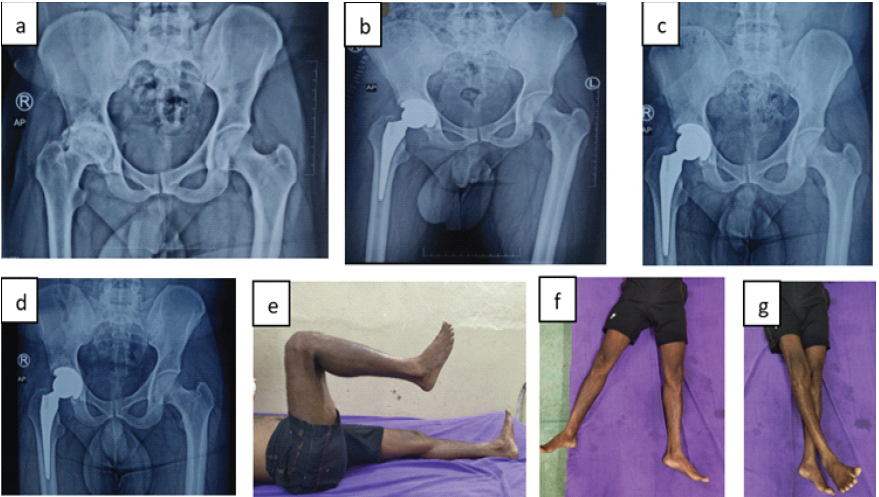
Figure 1: A 33-year-old male with secondary osteoarthritis of the right hip due to osteonecrosis of the femoral head. Sequential radiographic and clinical images demonstrate stable press-fit acetabular cup fixation without screws and progressive recovery with early weight bearing. (a) Pre-operative radiograph showing secondary osteoarthritis changes with a deformed head due to osteonecrosis of the femoral head. (b) Immediate post-operative radiograph showing a well-seated press-fit cup in optimal position. (c) Three-month post-operative radiograph showing maintained cup alignment. (d) Twelve-month follow-up radiograph confirming osseointegration and stable fixation. (e, f, g) Clinical photographs at 12 months demonstrating pain-free hip flexion, abduction, and adduction.
Intraoperative findings and operative parameters
Out of 30 patients, 25 (83.3%) had normal intraoperative findings. One patient (3.3%) each showed fragile soft tissue, a membranous acetabular roof, soft-tissue ingrowth, soft-tissue metallosis, or a thick acetabular capsule. The average surgery duration was 87.23 min (range: 60–135 min), and the mean intraoperative blood loss was 388.67 mL (range: 220–820 mL). Mean cup inclination was 44.3° ± 2.4° (range: 38°–48°). 23 (76.7%) of femoral stems were centrally aligned, 7 (23.3%) were in slight valgus. Five patients had minor LLD (<1 cm): 0.3 cm (1 patient), 0.5 cm (1 patient), and 0.7–0.8 cm (3 patients). No functional complaints or corrective interventions were necessary. No significant change in acetabular inclination or evidence of component migration was observed between the immediate post-operative and 12-month radiographs. None of the patients (0.0%) exhibited loosening at 1 month, 3 months, 6 months, and 12 months follow-up intervals. All femoral components showed stable fixation with no radiolucent lines across any Gruen zone.
Functional outcomes
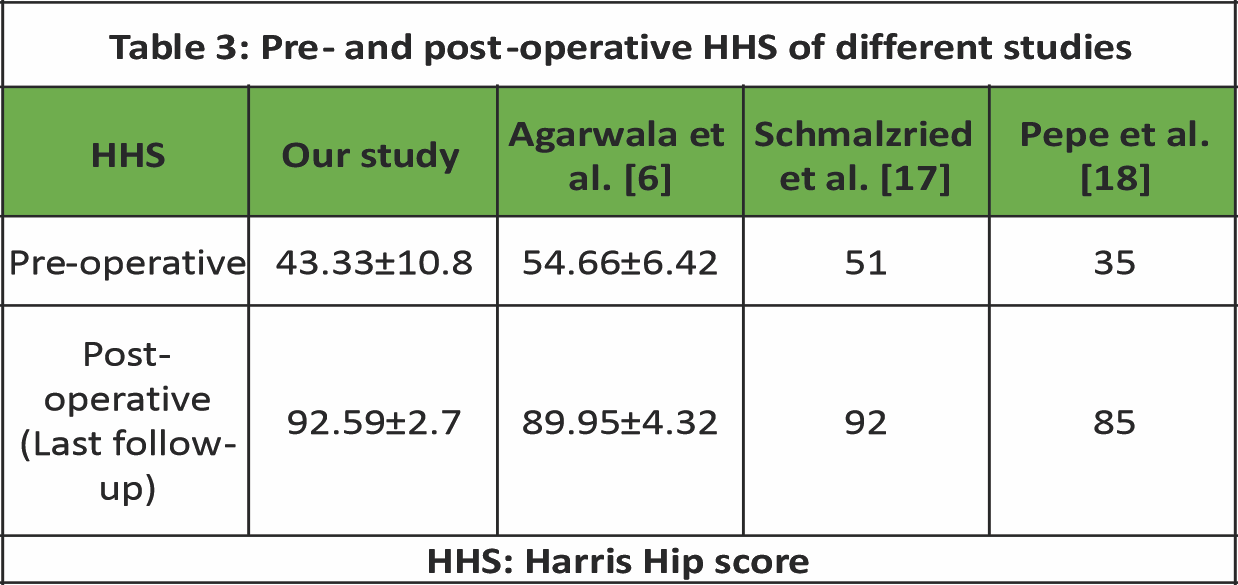
The HHS showed statistically significant improvement at all post-operative time points. Statistical analysis included paired t-tests and repeated-measures analysis of variance (α = 0.05). All improvements from baseline were statistically significant (P < 0.001). The pre-operative mean Harris Hip score was 43.33 ± 10.8, which improved to 92.59 ± 2.7 at 12 months follow-up (Table 1 and Fig. 2).
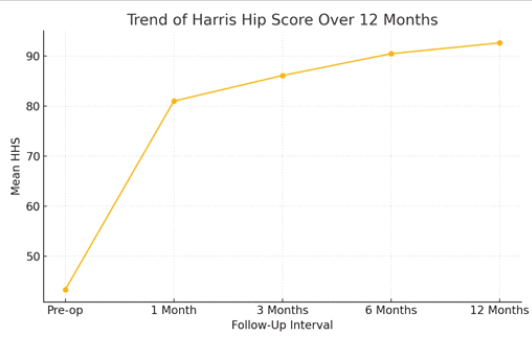
Figure 2: Illustrates the trend demonstrating sustained improvement over 12 months.
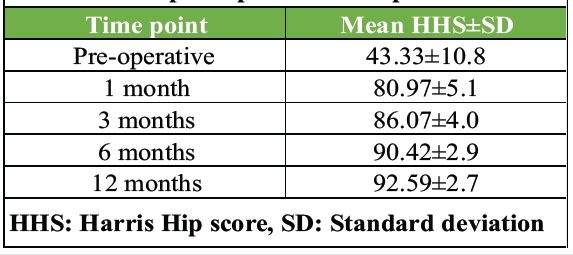
Table 1: Significant improvement in HHS from baseline to all post-operative time points
Acetabular component (DeLee–Charnley zones)
All radiographs were assessed independently by two senior orthopedic surgeons to ensure consistency in radiographic interpretation. No cases of tilting, mechanical failure, component migration, loosening, or progressive radiolucent lines were observed across all DeLee and Charnley zones at any follow-up interval (n = 29 at final follow-up). All acetabular components demonstrated stable fixation.
Femoral component (Gruen zones)
For each patient, radiolucent lines were recorded across zones 1–3 and zones 4–7, along with stem subsidence and any varus or valgus alignment change. All patients demonstrated a complete absence of lucency in all Gruen zones. Stem subsidence remained between 0 and 1 mm across the cohort, and no varus or valgus shifts were detected.
Acetabular inclination over time
Mean acetabular inclination remained stable throughout all follow-up intervals, with no measurable migration or positional change on serial radiographs. Inter-observer reproducibility for inclination measurement was excellent, with an ICC of 0.94. Agreement for the presence or absence of acetabular radiolucent lines was perfect, with a Cohen’s kappa value of 1.0.4.4 Polar Gaps.
Polar gaps
Initial polar gaps noted in some immediate post-operative radiographs showed sequential reduction over follow-up visits, indicating progressive osseointegration. No progression or new gaps were observed.
Complications
No cases of dislocation, infection, thromboembolic events, nerve injury, mechanical failure, component migration, or progressive radiolucency were identified during the study period. All patients were mobilized with full weight-bearing from post-operative day 2 with no adverse effect on component stability.
Subgroup Analysis
Comparison of functional outcome between AVN versus post-traumatic arthritis
No statistically significant difference was found between groups in HHS improvement. No patient in either subgroup demonstrated radiolucency, migration, or loosening (Table 2).
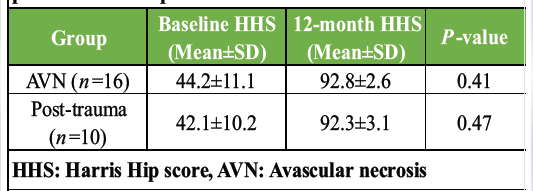
Table 2: Subgroup comparison of HHS between AVN and post-traumatic hip disease
Radiographic stability (AVN vs. post-trauma)
No patient in either subgroup exhibited radiolucency, component migration, or signs of loosening at any follow-up interval. Radiographic outcomes were therefore comparable between groups, with no detectable difference in stability. The comparative P-value (Fisher’s exact test) was P ≤ 1.0, indicating no statistically significant difference between the AVN and post-trauma cohorts.
This review synthesizes available evidence supporting the use of screwless press-fit acetabular cups in uncemented THA, contextualized with the outcomes of our clinical study. The findings reaffirm that modern press-fit designs, when properly implanted, offer excellent stability, functional outcomes, and complication profiles comparable to traditional screw-assisted fixation. In our study, the distribution of 30 patients based on age groups showed that the majority were between 31 and 40 years (30.0%) and 41–50 years (30.0%). In a study by Tian et al. involving 452 hips, the most commonly affected age group had an average age of 54 years. [15]. The age demographic of our study leaned more toward the younger population. We found that the majority of patients were male, comprising 24 patients (80.0%), whereas females accounted for 6 patients (20.0%) in our study. Similar findings were seen in a study done by Kumar et al., where the male-to-female ratio was 3.2:1 [16]. In our study, the average surgery duration was 87.23 min (range: 60–135 min), and the mean intraoperative blood loss was 388.67 mL (range: 220–820 mL). Zhu and Shen did a randomized study and observed that the mean operation time and blood loss during operation in the non-screw fixation group were less than those in the screw fixation group [5]. In our prospective study, the mean pre-operative HHS was 43.33 ± 10.8. Postoperatively, among the 29 patients, the mean scores significantly improved to 92.59 ± 2.7 at 12 months follow-up (Table 3).
Our study shows that out of 29 patients, none of the patients (0.0%) exhibited component migration or loosening of the acetabular or femoral component at 1 month, 3 months, 6 months, or 12 months. Wolf et al. in his study on the effect of full versus partial post-operative weight bearing on the stability of press-fit cups over 5 years, observed that there is a difference in the inclination of cups (rotation around the Z-axis) between the weight bearing regimes at 1 month and at 2 years, but not after 5 years and also found no difference in micromotion of the stem between the groups at 5 years [19]. Tian et al. [15] did a meta-analysis aimed to investigate the efficacy and safety of partial versus early full weight bearing after uncemented THA and showed no significant difference in HHS between the two groups during the 1st and 2nd year follow-up. However, one study demonstrated that during the first 3 months after uncemented THA, the Harris score of the hip joints in the full weight-bearing group was higher than that of the partial weight-bearing group. Early weight-bearing was not associated with any increase in migration, loosening, or complications in our study. This aligns with biomechanical data from Tabata et al. and Goldman et al., both of whom demonstrated that well-fitted press-fit cups alone provide adequate torsional stability, particularly when using roughened or porous surfaces [3,4]. Our study reported no evidence of component migration, and initial polar gaps resolved over time, suggesting successful bone ingrowth. This finding mirrors the outcomes in the case series by Agarwala et al., who demonstrated progressive disappearance of polar gaps in screwless cups within 12 months [6]. Further radiographic stability was noted in the work by Chiapale et al., who studied highly porous cups in elderly trauma patients, confirming radiological integration without screw fixation [7]. In our study, we observed that early full weight bearing over a press fit cup is safe and has not caused any component migration, periacetabular lucency, or any other functional limitations. Thien et al. [20] mentioned that by partial weight bearing, functional recovery may be inhibited, and muscle atrophy and loss of bone mineral density increased. Load on the contralateral hip and upper extremities is significantly higher when less weight is put on the operated lower limb [21]. Immediate weight bearing after uncemented THA shortens the length of stay in hospital, reduces the risk of deep venous thrombosis, and promotes functional recovery with less usage of ambulatory devices [22,23]. The strengths of this study include its prospective design with a standardized surgical protocol, comprehensive assessment combining clinical, functional, and radiographic outcomes, and the implementation of an early mobilization regimen that supports the mechanical reliability of screwless press-fit fixation. However, several important limitations must be acknowledged. The sample size was relatively small (n = 30, with 29 completing a 12-month follow-up), which limits the statistical power and generalizability of the findings. The study was conducted at a single center by a single surgeon, which may reduce external validity and introduce operator-dependent effects. The cohort had a relatively young mean age, limiting applicability to older patients with osteoporotic bone. The follow-up duration of 12 months is short and precludes evaluation of long-term outcomes such as aseptic loosening, revision rates, and late complications. In addition, radiographic assessment relied on standard X-rays rather than more sensitive modalities such as radiostereometric analysis or computed tomography, introducing potential measurement bias. Subgroup analyses (AVN vs. post-traumatic hips) are exploratory and underpowered, warranting cautious interpretation. These limitations highlight the need for larger, multicenter studies with extended follow-up to confirm the durability and generalizability of screwless press-fit acetabular fixation.
Screwless fixation in porous press-fit acetabular cups has evolved into a clinically validated alternative to screw-assisted techniques in uncemented THA. Based on current biomechanical insights and clinical studies, including our prospective observational experience, screwless designs provide excellent primary stability, promote osseointegration, and deliver functional outcomes comparable to screw-assisted implants. Our findings support that early full weight-bearing from day 2 postoperatively can be safely implemented in patients with adequate bone quality and proper cup positioning. The absence of migration, loosening, or significant complications reinforces the mechanical reliability of modern screwless press-fit designs. While the current evidence is compelling, larger multicenter studies with longer follow-up periods are needed to validate these findings across varied patient populations and implant types. Until then, screwless fixation remains a strong, evidence-based option in appropriately selected cases, minimizing hardware-related risks while preserving clinical outcomes.
A properly implanted press-fit acetabular cup can achieve secure fixation without screws. Early full weight-bearing does not compromise stability or lead to loosening. This approach supports smooth recovery while avoiding complications related to screw insertion.
References
- 1. Ni SH, Guo L, Jiang TL, Zhao J, Zhao YG. Press-fit cementless acetabular fixation with and without screws. Int Orthop. 2014 Jan;38(1):7-12. doi: 10.1007/s00264-013-2075-2. Epub 2013 Aug 28. PMID: 23982638; PMCID: PMC3890122 [Google Scholar] [PubMed] [CrossRef]
- 2. Koutserimpas C, Kotzias D, Argyrou A, Veizi E, Alpantaki K, Karamitros A, Piagkou M. Press-fit vs threaded acetabulum components for total hip arthroplasty – A systematic review with metanalysis. J Clin Orthop Trauma. 2024 Jul 4; 54:102488. doi: 10.1016/j.jcot.2024.102488. PMID: 39071857; PMCID: PMC11277367. [Google Scholar] [PubMed] [CrossRef]
- 3. Stefanini N, Pederiva D, Brunello M, Geraci G, Pilla F, Capozzi E, Di Martino A, Faldini C. Acetabular screws placement in primary and revision total hip arthroplasty: a narrative review. Arch Orthop Trauma Surg. 2025 Jun 25;145(1):354. doi: 10.1007/s00402-025-05961-2. PMID: 40560254. [Google Scholar] [PubMed] [CrossRef]
- 4. Soliman MM, Islam MT, Chowdhury MEH, Alqahtani A, Musharavati F, Alam T, Alshammari AS, Misran N, Soliman MS, Mahmud S, Khandakar A. Advancement in total hip implant: a comprehensive review of mechanics and performance parameters across diverse novelties. J Mater Chem B. 2023 Nov 15;11(44):10507-10537. doi: 10.1039/d3tb01469j. PMID: 37873807. [Google Scholar] [PubMed] [CrossRef]
- 5. Finch DJ, Martin BI, Franklin PD, Magder LS, Pellegrini VD Jr; PEPPER Investigators. Patient-Reported Outcomes Following Total Hip Arthroplasty: A Multicenter Comparison Based on Surgical Approaches. J Arthroplasty. 2020 Apr;35(4):1029-1035.e3. doi: 10.1016/j.arth.2019.10.017. Epub 2019 Oct 17. PMID: 31926776; PMCID: PMC8218222. [Google Scholar] [PubMed] [CrossRef]
- 6. Agarwala S, Jadia C, Vijayvargiya M. Incorporation of screwless press-fit acetabular cups and disappearance of polar gaps. J Clin Orthop Trauma. 2020 Jan-Feb;11(1):85-90. doi: 10.1016/j.jcot.2018.11.012. Epub 2018 Nov 30. PMID: 32001991; PMCID: PMC6985010. [Google Scholar] [PubMed] [CrossRef]
- 7. Chiapale D, Vitali F, Rubino F, Colombo M, Formica M. Acute total hip arthroplasty with a highly-porous multi-holes cup in elderly patients after traumatic acetabular fracture: A case series and literature review. Trauma Case Rep 2024; 52:101070. [Google Scholar] [PubMed]
- 8. Punnoose DJ, George P, Wakure A, Kandathil JC, Theruvil B. “External Iliac Artery Injury After Total Hip Arthroplasty in an Infected Intrapelvic Hemiarthroplasty”: A Case Report. JBJS Case Connect. 2023 Aug 9;13(3). doi: 10.2106/JBJS.CC.23.00070. PMID: 37556580. [Google Scholar] [PubMed] [CrossRef]
- 9. Klutzny M, Singh G, Hameister R, Goldau G, Awiszus F, Feuerstein B, Stärke C, Lohmann CH. Screw Track Osteolysis in the Cementless Total Knee Replacement Design. J Arthroplasty. 2019 May;34(5):965-973. doi: 10.1016/j.arth.2018.12.040. Epub 2019 Jan 6. PMID: 30777624. [Google Scholar] [PubMed] [CrossRef]
- 10. Zhao Y, Chen H, Ran K, Zhang Y, Pan H, Shangguan J, Tong M, Yang J, Yao Q, Xu H. Porous hydroxyapatite scaffold orchestrated with bioactive coatings for rapid bone repair. Biomater Adv. 2023 Jan; 144:213202. doi: 10.1016/j.bioadv.2022.213202. Epub 2022 Nov 17. PMID: 36434928. [Google Scholar] [PubMed] [CrossRef]
- 11. Stambough JB, Nunley RM. The cementless acetabulum. In: The Hip: Preservation, Replacement, and Revision. Netherlands: Elsevier; 2015. p. 217-28. [Google Scholar] [PubMed]
- 12. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 1976; 121:20-32. [Google Scholar] [PubMed]
- 13. Siwach R, Kadyan VS, Sangwan S, Gupta R. A retrospective study of total hip arthroplasty. Indian J Orthop. 2007;41(1):62-66. doi:10.4103/0019-5413.30528 [Google Scholar] [PubMed] [CrossRef]
- 14. Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: A radiographic analysis of loosening. Clin Orthop Relat Res 1979; 141:17-27. [Google Scholar] [PubMed]
- 15. Tian P, Li ZJ, Xu GJ, Sun XL, Ma XL. Partial versus early full weight bearing after uncemented total hip arthroplasty: A meta-analysis. J Orthop Surg Res 2017; 12:31. [Google Scholar] [PubMed]
- 16. Kumar P, Sen RK, Aggarwal S, Jindal K. Common hip conditions requiring primary total hip arthroplasty and comparison of their post-operative functional outcomes. J Clin Orthop Trauma 2020;11: S192-5. [Google Scholar] [PubMed]
- 17. Schmalzried TP, Wessinger SJ, Hill GE, Harris WH. The Harris-Galante porous acetabular component press-fit without screw fixation. Five-year radiographic analysis of primary cases. J Arthroplasty 1994; 9:235-42. [Google Scholar] [PubMed]
- 18. Pepe M, Kocadal O, Erener T, Ceritoglu K, Aksahin E, Aktekin CN. Acetabular components with or without screws in total hip arthroplasty. World J Orthop 2017; 8:705-9. [Google Scholar] [PubMed]
- 19. Wolf O, Mattsson P, Milbrink J, Larsson S, Mallmin H. The effects of different weight-bearing regimes on press-fit cup stability: A randomised study with five years of follow-up using radiostereometry. Int Orthop 2012; 36:735-40. [Google Scholar] [PubMed]
- 20. Thien TM, Ahnfelt L, Eriksson M, Strömberg C, Kärrholm J. Immediate weight bearing after uncemented total hip arthroplasty with an anteverted stem: A prospective randomized comparison using radiostereometry. Acta Orthop 2007; 78:730-8. [Google Scholar] [PubMed]
- 21. Rao RR, Sharkey PF, Hozack WJ, Eng K, Rothman RH. Immediate weightbearing after uncemented total hip arthroplasty. Clin Orthop 1998; 349:156-62. [Google Scholar] [PubMed]
- 22. Leali A, Fetto J, Moroz A. Prevention of thromboembolic disease after non-cemented hip arthroplasty. A multimodal approach. Acta Orthop Belg 2002; 68:128-34. [Google Scholar] [PubMed]
- 23. Kishida Y, Sugano N, Sakai T, Nishii T, Haraguchi K, Ohzono K, et al. Full weight-bearing after cementless total hip arthroplasty. Int Orthop 2001; 25:25-8. [Google Scholar] [PubMed]











