Glomus tumors are most commonly found in the nail bed, but very rarely, can also be found in extradigital sites, such as the forearm, and hence, a high index of suspicion of such non-stereotypical manifestations is needed for timely imaging and surgical excision, to achieve improved results.
Dr. Aashiket Sable, Department of Arthroscopy and Sports Medicine, Sportsmed, Mumbai, Maharashtra, India. E-mail: aashiketsable67@gmail.com
Introduction: Glomus tumors are benign vascular tumors that are rare and most usually located in the nail bed. They may go undetected when they are found in unusual places, such as the forearm, and hence, cause a delay in diagnosis and treatment. In this report, we have discussed a 34-year-old man with a history of forearm pain, which was diagnosed as a glomus tumor, thus illustrating the importance of a high index of suspicion about unusual sites of such a tumor in cases of persistent pain to make an early diagnosis and enable faster treatment.
Case Report: A 34-year-old man presented with a history of local forearm pain over a long period, with a tender purplish subcutaneous swelling over the medial aspect of the upper forearm. The pain was chronic and exaggerated even on light touch, with no history of trauma or family history. The clinical observation showed a non-indurated, solitary and non-inflammatory lesion, without any inflammation. Ultrasound and magnetic resonance imaging showed a clearly defined, superficial, subcutaneous lesion, with homogeneous post-contrast enhancement, directly over the basilic vein. The patient was surgically treated by wide local excision with an elliptical incision. In the course of surgery, a well-circumscribed dark red mass was found and excised in its entirety. A histopathological analysis of a well-circumscribed dermal and subcutaneous tumor of glomus cells in the form of a nest confirmed the diagnosis of glomangioma. At 1-year follow-up, the patient had no symptoms. This case illustrates the possibility of extradigital glomus tumors in individuals who present with chronic localized unexplained forearm pain.
Conclusion: The case highlights the importance of diagnosing extradigital glomus tumors as a potential cause of chronic and localized pain in the limbs. Their abnormal location and insidious presentation often lead to neglect of such tumors, and therefore, their diagnosis becomes late and causes the patient undue discomfort. Even though clinical suspicion and appropriate imaging are useful in the early diagnosis, surgical excision is the treatment of choice, which offers complete relief. This report highlights the fact that early diagnosis can enhance the outcome of such cases.
Keywords: Glomus tumor, chronic subcutaneous lesion, glomangioma, chronic forearm pain.
Glomus tumors are rare, benign tumors that comprise <2% of soft tissue neoplasms that are most often located in the subungual region of digits. They have their origin in the glomus body, a specialized arteriovenous anastomosis involved in thermoregulation [1]. Its common symptoms are: Local pain, cold sensitivity, and pinpoint tenderness -which are easily diagnosed when they occur in the normal locations. Presence of these tumors over unusual sites, as in the forearm, is usually missed, leading to late diagnosis and unnecessary investigations leading to a delay in recovery [2]. The unusual location and nonspecific presentation of extradigital glomangiomas can mimic a wide range of differential diagnoses, including neuromas, hemangiomas, and chronic inflammatory conditions, thus resulting in prolonged suffering and misdiagnoses [3]. The modality of choice for preoperative localization is a magnetic resonance imaging (MRI), which typically demonstrates a well-circumscribed, enhancing lesion. Definitive diagnosis is established via histopathology following complete surgical excision, which is also curative in most cases [3]. We report a rare case of a glomangioma located in the medial aspect of the upper forearm, which remained undiagnosed for nearly 8 years. This case emphasizes the need for clinical suspicion and the inclusion of glomus tumors in the differential diagnosis of chronic, unexplained limb pain, especially when accompanied by a localized tender lesion.
A 34-year-old male came to our outpatient department with localized, persistent, dull pain and a gradually progressive visible lesion over the medial aspect of his right upper forearm for 8 years (Fig. 1). The lesion was purplish in color with increased sensitivity to light touch. There was no history of trauma, systemic illness, or significant family history.

Figure 1: Right forearm site of pain.
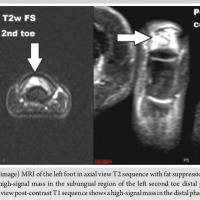
Clinical examination revealed a well-defined, soft, bluish papule over the medial forearm. The lesion was approximately half a centimeter in diameter, with marked local tenderness but no induration, temperature rise, or regional lymphadenopathy. Given the chronicity and focal nature of symptoms, a benign soft tissue tumor was suspected. Initial blood investigations were unremarkable. Ultrasonography showed a well-circumscribed hypoechoic subcutaneous lesion without vascular invasion. MRI of the forearm revealed a small, superficial, subcutaneous lesion with homogeneous post-contrast enhancement (Fig. 2). It was located close to the basilic vein, yet distinct from vascular structures, raising suspicion for a vascular tumor, possibly a glomus tumor.
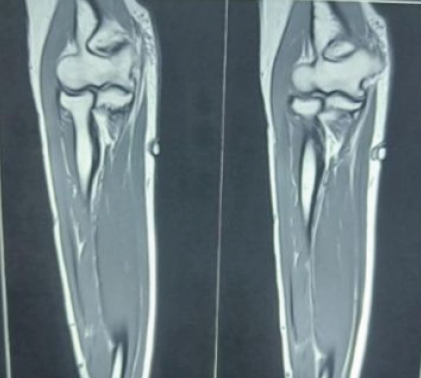
Figure 2: Magnetic resonance imaging of right forearm showing a small, superficial, subcutaneous lesion with homogeneous post-contrast enhancement.
Based on clinical and radiological findings, the patient was scheduled for surgical management. Under general anesthesia, an elliptical incision was made directly over the lesion. Intraoperatively, a well-encapsulated, dark red nodule was visualized within the subcutaneous plane and excised completely (Fig. 3). The mass appeared firm but not infiltrative and was sent for histopathological evaluation.
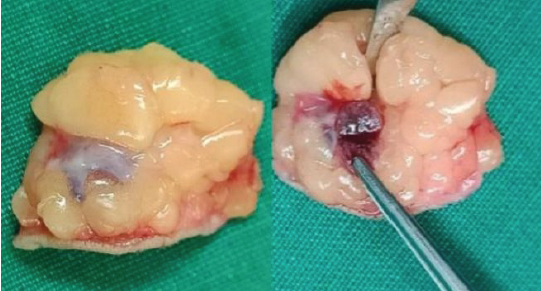
Figure 3: Excised glomus tumor mass.
Microscopy showed a well-circumscribed dermal and subcutaneous tumor composed of uniform round cells with eosinophilic cytoplasm and centrally located round nuclei, arranged in nests and trabeculae. The tumor was richly vascular, consistent with a diagnosis of glomangioma, a variant of glomus tumor (Fig. 4). There was no evidence of malignancy or atypia.
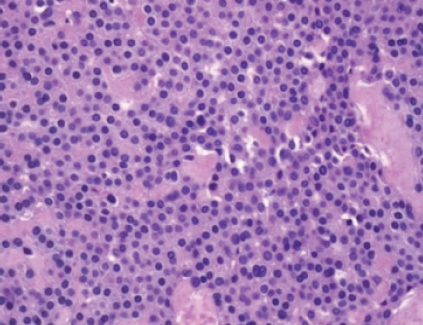
Figure 4: Microscopy examination findings of excised mass (low power ×20 magnification).
The post-operative period was uneventful. The surgical site healed well with no signs of infection, hematoma, or delayed wound healing. Analgesics were prescribed for mild discomfort, and sutures were removed on day 10. At 1-week follow-up, the patient reported complete relief from preoperative pain and hypersensitivity. No recurrence or new symptoms were noted at 1 and 3-month follow-ups. The patient was advised to perform routine self-monitoring and to report any new symptoms. Overall, the surgical outcome was excellent, with full functional and symptomatic recovery. At 1 year of follow-up, the patient was relieved of the pain with no recurrence observed.
Wood, in 1812, first described glomus tumors as painful subcutaneous nodules of vascular origin4, while Masson in 1924, provided a detailed histological description. He identified their origin from the glomus body, that is, an arteriovenous structure involved in thermoregulation [1,5]. Although these tumors are classically associated with the subungual region of the fingers, extradigital locations remain rare and unrecognized, accounting for approximately 11–20% of all glomus tumors [1]. The classic symptom triad – paroxysmal pain, localized tenderness, and cold hypersensitivity is well established in subungual glomus tumors but may not always be present in extradigital forms [6]. Consequently, extradigital glomus tumors often present a diagnostic dilemma. Patients may endure years of unbearable, focal pain and undergo multiple consultations before the true diagnosis is reached. Our case is a prime example, where the patient suffered for 8 years before identification and definitive treatment. Schiefer et al. reported an average diagnostic delay of 7 years in extradigital glomus tumor cases, highlighting the frequency of such a clinical condition [2]. Glomus tumors may clinically present as small, moderately firm nodules, at times with bluish discoloration. However, deeper lesions, especially in the forearm, lack cutaneous signs, which make clinical diagnosis more difficult [2]. This makes localized tenderness the only reliable clinical sign. As far as imaging goes, ultrasound may detect a hypoechoic lesion with vascularity; it has high sensitivity but lacks specificity. MRI remains the gold standard, offering superior sensitivity and specificity. Glomus tumors typically appear as well-demarcated, T1-isointense and T2-hyperintense lesions with enhancement on post-contrast sequences [3]. In our patient, MRI effectively delineated the lesion’s proximity to the basilic vein, guiding surgical planning. Histologically, glomangiomas are a subtype of glomus tumor characterized by dilated vascular channels surrounded by uniform, round glomus cells with eosinophilic cytoplasm. They are well-circumscribed, located within the dermis or subcutaneous tissue, and lack features of malignancy [7]. While malignant glomus tumors have been described, they are extremely rare and usually present as large, deep-seated masses with nuclear atypia and mitotic activity [9]. In our case, there was no evidence of malignancy or atypia. Complete surgical excision remains the definitive treatment, typically resulting in immediate symptom relief and low recurrence rates. Incomplete excision is the primary cause of recurrence [3]. Our patient underwent complete removal with an uneventful recovery and was symptom-free at follow-up. Recent literature shows that glomus tumors represent a diverse group of perivascular soft-tissue neoplasms, with unusual locations increasingly recognized in present clinical practice [9]. As per the recent WHO classifications, the recent taxonomy of vascular and perivascular tumors have been revised owing to these unusual presentations [10]. Improved radiologic resolution and advanced histopathologic techniques have enhanced detection of atypical forms, thereby being a great help in reducing diagnostic delays in rare or deep-seated lesions [11,12]. This case reinforces the importance of considering extradigital glomus tumors in patients with focal, persistent limb pain, particularly when initial workup is inconclusive. Early diagnosis can prevent delays in effective treatment. A systematic treatment approach can enhance diagnostic accuracy and surgical outcomes. Recent reports also highlight the psychological toll of delayed diagnosis, which makes early intervention and clear communication with such patients very important [13,14].
This case highlights the diagnostic challenge one may face while treating extradigital glomus tumors, especially when they present with minimal clinical findings. In the absence of trauma or any other pathology, the diagnosis becomes difficult. Peculiar features, such as localized tenderness, discoloration, and cold sensitivity should raise clinical suspicion. A systematic treatment approach combining clinical examination and imaging should be advocated to guide early diagnosis. Surgical excision is the mainstay treatment option and typically results in complete resolution of symptoms, as proved in this case. The unusual location and delayed diagnosis in this case highlight the need for broader clinical awareness to prevent prolonged patient suffering and avoid unnecessary interventions.
There should be a high index of suspicion to identify extradigital glomus tumors for timely imaging and surgical excision, to achieve improved results.
References
- 1. Schiefer TK, Parker WL, Anakwenze OA, Amadio PC, Inwards CY, Spinner RJ. Extradigital glomus tumors: A 20-year experience. Mayo Clin Proc 2006;81:1337-44. [Google Scholar] [PubMed]
- 2. Lee DW, Yang JH, Chang S, Won CH, Lee MW, Choi JH, Moon KC. Clinical and pathological characteristics of extradigital and digital glomus tumours: a retrospective comparative study. J Eur Acad Dermatol Venereol. 2011 Dec;25(12):1392-7. doi: 10.1111/j.1468-3083.2011.03979.x. Epub 2011 Mar 4. PMID: 21371130. [Google Scholar] [PubMed] [CrossRef]
- 3. Drapé JL, Feydy A, Guerini H, Desmarais E, Godefroy D, Le Viet D, Chevrot A. Vascular lesions of the hand. Eur J Radiol. 2005 Dec;56(3):331-43. doi: 10.1016/j.ejrad.2005.03.013. PMID: 16298677. [Google Scholar] [PubMed] [CrossRef]
- 4. Wood W. On painful subcutaneous tubercle. Edinburgh Med Surg J. 1812;8:283-291.Edinburgh Med Surg J. 1812;8:283-291 [Google Scholar] [PubMed]
- 5. Masson P. Le glomus neuromyoarterial des régions tactiles et ses tumeurs. Lyon Chir 1924;21:257-80. [Google Scholar] [PubMed]
- 6. Bhaskaranand K, Navadgi BC. Glomus tumour of the hand. J Hand Surg Br 2002;27:229-31. [Google Scholar] [PubMed]
- 7. Gould EW, Manivel JC, Albores-Saavedra J. Glomus tumor: A clinicopathologic and immunohistochemical study of 20 cases. Hum Pathol 1990;21:931-6. [Google Scholar] [PubMed]
- 8. Folpe AL, Fanburg-Smith JC, Miettinen M, Weiss SW. Atypical and malignant glomus tumors: Analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol 2001;25:1-12. [Google Scholar] [PubMed]
- 9. Kransdorf MJ, Larsen BT, Fox MG, Murphey MD, Long JR. Musculoskeletal glomus tumor: A review of 218 lesions in 176 patients. Skeletal Radiol 2025;54:457-79. [Google Scholar] [PubMed]
- 10. Sbaraglia M, Bellan E, Dei Tos AP. The 2020 WHO classification of soft tissue tumours: News and perspectives. Pathologica 2021;113:70-84. [Google Scholar] [PubMed]
- 11. Gombos Z, Zhang PJ. Glomus tumor. Arch Pathol Lab Med 2008;132:1448-52. [Google Scholar] [PubMed]
- 12. Temiz G, Şirinoğlu H, Demirel H, Yeşiloğlu N, Sarıcı M, Filinte GT. Extradigital glomus tumor revisited: Painful subcutaneous nodules located in various parts of the body. Indian J Dermatol 2019;61:118. [Google Scholar] [PubMed]
- 13. Vasisht B, Watson HK, Joseph E, Lionelli GT. Glomus tumor of the hand: A review of 51 cases. J Hand Surg Am 2004;29:405-8. [Google Scholar] [PubMed]
- 14. Morey VM, Garg B, Kotwal PP. Glomus tumours of the hand: Review of literature. J Clin Orthop Trauma 2016;7:286-91. [Google Scholar] [PubMed]