Salvage of ray with metatarsal Giant cell tumor using hemifibular autograft with successful incorporation of graft, good functional outcome, and minimal donor site morbidity.
Dr. Cheralathan Senguttuvan, Institute of Orthopaedics and Traumatology, Madras Medical College and Rajiv Gandhi Government General Hospital, Chennai, Tamil Nadu, India. E-mail: cheraid4@gmail.com
Introduction: Giant cell tumor (GCT) arising in the small bones of the feet is a rare entity, often presenting diagnostic and therapeutic challenges due to local aggression and the need to preserve foot architecture. This report details the case of a 27-year-old female diagnosed with a GCT of the left fifth metatarsal.
Case Report: This particular patient was managed with en masse resection of the fifth metatarsal followed by reconstruction using a non-vascularized autologous hemifibular strut graft fixed with K-wire. The patient demonstrated good clinical and radiographic fusion at 6 months and excellent functional recovery at 2-year follow-up.
Conclusion: GCT of the metatarsal has been managed with vascularized bone graft, which is technically difficult. We could achieve good results with a non-vascular hemifibular graft, confirming this as a viable method for managing rare GCTs in critical load-bearing locations.
Keywords: Giant cell tumor, autograft, hemifibular graft
Giant cell tumors (GCTs) are locally aggressive, benign bone neoplasms that primarily affect the metaphysis of long bones, most commonly the distal femur and proximal tibia [1]. However, their presentation in the bones of the foot and ankle is exceedingly rare, constituting <1% of all reported GCT cases [2,3]. This unusual location presents distinct diagnostic and therapeutic challenges, as management must balance effective tumor control with preservation of the foot’s complex weight-bearing and functional anatomy [4]. En masse resection is often the most reliable method for definitive tumor control in these anatomically restrictive sites, while reconstruction using autologous fibular grafts provides both structural support and high osteointegration potential [5]. We report a case of metatarsal GCT managed with non-vascular hemifibular autograft.
A 26-year-old South Indian female presented to the orthopedic outpatient department during June 2023, with localized pain and swelling in the dorsolateral aspect of the left foot, which progressively increased in size over the past 3 months. She was apparently normal before 3 months. Later, she developed pain over the left foot, which was insidious in onset, progressive in nature, dull aching type, non-radiating, intermittent type, aggravated on activities of daily living, relieved on taking analgesics and rest. On examination, a solitary, tender, firm swelling of size 7*3 cm was seen over the dorsum of the left foot in the 5th metatarsal region with well-defined margins, and a smooth surface, arising from the bone itself (Fig. 1).

Figure 1: Clinical image of the lesion
Overlying skin was normal and there was no tethering. There was no distal neurovascular deficit. The range of movements of the metatarsophalangeal joint was normal. No history of trauma was reported. Family history nil relevant.
Radiograph of the left foot showed the presence of a meta-diaphyseal, expansile, osteolytic lesion, involving the entire shaft of the 5th metatarsal with minimal periosteal reaction. The lesion had the characteristic soap-bubble appearance with multiple internal septations. The tumor had a clear margin and the proximal and distal epiphyseal regions were not involved. The features were suggestive of a locally aggressive benign bone tumor (Fig. 2).

Figure 2: Radiograph of left foot anteroposterior (a), oblique (b), and lateral view (c) of left foot
Computed tomography scan showed an expansile lytic lesion with well-defined margins and internal septations involving the shaft of left 5th metatarsal, without involvement of the proximal and distal epiphysis (Fig. 3).

Figure 3: Computed tomography image of lesion in sagittal (a), axial cut (b and c), and 3D-reconstruction (d-f)
Our differential diagnosis based on the clinicoradiologial findings were Aneurysmal bone cyst, GCT and Enchondroma. The lesion also had significant expansion without clear evidence of soft tissue involvement with surrounding edema. Trucut biopsy was done and reported to be suggestive of Aneurysmal bone cyst. Routine blood investigations C-reactive protein, erythrocyte sedimentation rate, liver and renal function tests were within normal and negative serology. Anesthetic assessment was obtained and the patient was planned for surgery.
Surgical technique
The patient underwent surgical intervention on June 22, 2023, under epidural plus spinal anesthesia in the supine position. The patient was planned for en masse resection of the entire metatarsal bone, followed by reconstruction using an autologous non-vascular hemi-fibular strut graft and arthrodesis of the tarsometatarsal joint and metatarsophalangeal joint. Using the dorsal approach to the 5th metatarsal, the entire tumor was exposed (Fig. 4).
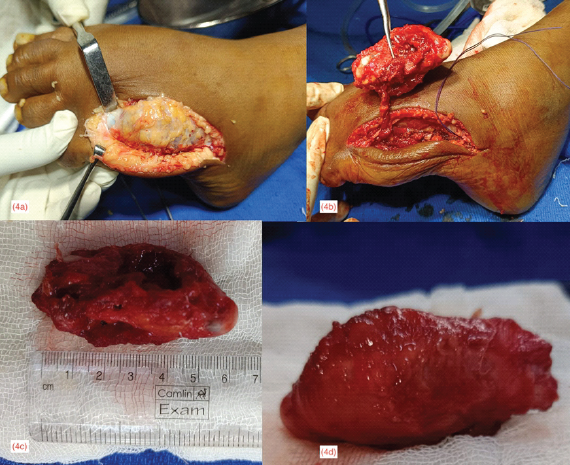
Figure 4: Surgical exposure of tumor (a), en masse excision (b), dimensions of the tumor mass (c), and gross pathological appearance (d)
Gross inspection revealed a soft tissue mass spanning the entire metatarsal. En masse resection of the affected fifth metatarsal bone in its entirety was performed with articular surface as the clearance margin, followed by application of hydrogen peroxide to ensure, no residual tumor cells were left in the surgical field. The excised tumor mass measured approximately 6.5 cm. The excised mass was promptly sent for histopathological analysis. A non-vascularized hemifibular strut graft (approximately 8 cm long) was harvested from the mid-third anterior part of the shaft of the fibula from the ipsilateral leg. The autologous fibular graft was appropriately shaped and placed to reconstruct the resected fifth metatarsal (Fig. 5).
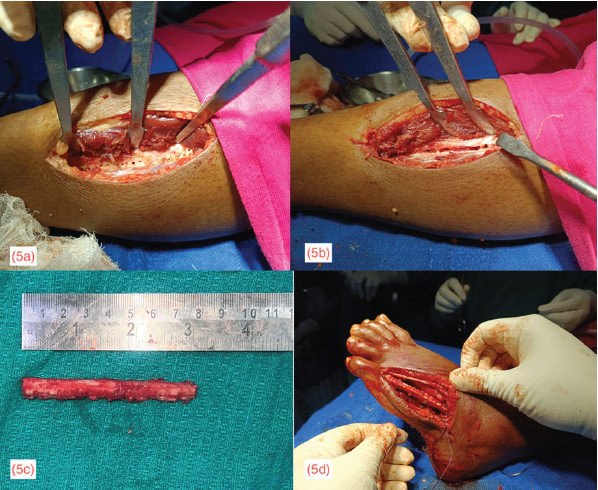
Figure 5: Multiple drill holes made longitudinally in the exposed shaft of fibula for marking of hemifibula (a); Drill holes connected to harvest hemifibula from the anterior half of the mid third shaft of fibula (b); 8 cm of hemifibula harvested (c); Reconstruction of 5th metatarsal using the non-vascular autogenous hemifibular strut graft
A central trough was created in the base of proximal phalanx of 5th toe and a similar trough was fashioned in the lateral aspect of the cuboid. The graft was wedged into the proximal and distal troughs created and stabilized using K-wires and further protected with below-knee cast. Fig. 6
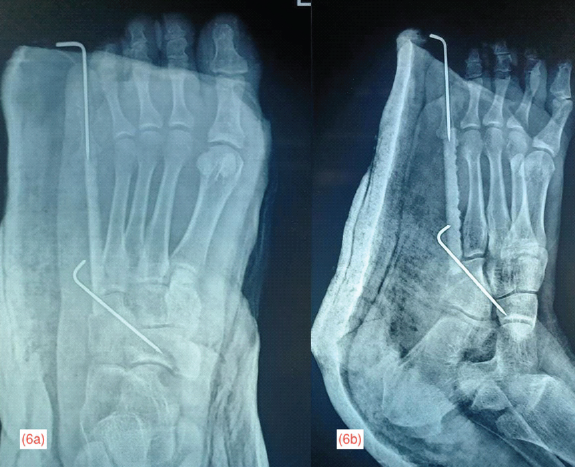
Figure 6: Immediate post-operative radiograph of left foot in anteroposterior (a) and oblique (b) projection showing the autogenous fibula strut graft secured to the cuboid proximally and to the proximal phalanx of the 5th toe distally using K-wire
shows the immediate post-operative radiograph of the foot protected with below knee cast. Fig. 7 shows the radiograph of the graft donor site in anteroposterior and lateral projection.
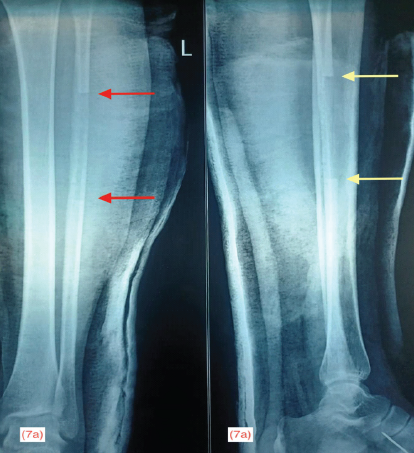
Figure 7: Immediate post-operative radiograph of the hemifibula bone graft donor site in anteroposterior projection with red arrows marking the length of graft (a) and lateral projection with yellow arrows marking the length of graft (b)
The definitive histopathological report was GCT with secondary Aneurysmal Bone Cyst changes. The specimen showed classic features: Osteoclast-like giant cells uniformly distributed in a background of mononuclear stromal cells with no nuclear atypia. Based on the above clinical, radiological and histopathological findings, the Enneking staging for this lesion is Stage 2 (Active). The post-operative period was uneventful and the patient was discharged on the 10th post-operative day. A below-knee cast was applied for 2 months to protect the graft and fixation and she was mobilized non-weight bearing. The distal K-wire was removed due to loosening at the end of the 2nd month. Below-knee cast continued for another 1 month and the proximal K-wire was removed at the end of the 3rd month. Fig. 8 shows the follow-up radiograph taken at the 2nd and 5th post-operative months.

Figure 8: Second month follow-up anteroposterior (a) and oblique view (b) radiograph of left foot showing K-wire in situ with disuse osteoporosis; 5th month follow-up anteroposterior (c) and oblique view (d) radiograph of left foot showing improvement in bone density following mobilization exercises
She was allowed partial weight bearing after 3 months and full weight bearing after 5 months. At the final follow-up of 2 years, the patient was walking with full-weight bearing without pain. Ankle movements were from 20° of plantar flexion to 10° of dorsiflexion, which was pain-free, but there was restriction of inversion and eversion. Fig. 9 shows the radiograph and Fig. 10 shows the clinical function of the patient at final follow-up. The patient was able to perform activities of daily living without significant pain or major functional deficit, demonstrating a successful outcome of the limb salvage procedure.

Figure 9: Final follow-up at the end of 2 years, showing radiograph of left foot in anteroposterior (a) and oblique (b) view, showing good incorporation of the hemifibula autograft

Figure 10: Clinical images at final follow-up at the end of 2 years showing appearance of left foot with similar morphology to right foot in frontal view (a); patient walking with full weight bearing on the left foot (b); active ankle plantar flexion (c) and dorsiflexion (d)
The Musculoskeletal Tumor Society (MSTS) score for this patient is calculated as 27/30 (90%) (Pain: 5 points, Function: 4 points, Emotional Acceptance: 5 points, Supports: 5 points, Walking Ability: 4 points, Gait: 4 points). This represents an excellent functional outcome following limb-salvage surgery for giant cell tumor of the fifth metatarsal bone. This score falls firmly within the excellent category (77–100%) and reflects successful surgical management with strong functional restoration.
GCTs of the metatarsal bones represent a rare subset of bone tumors with unique challenges in management due to their locally aggressive nature and propensity for recurrence when inadequately treated [2,3]. The anatomical constraints of the foot, including limited soft tissue coverage and the critical biomechanical role of metatarsals in weight-bearing, make surgical management particularly challenging [6]. In this case, the decision to perform wide en masse resection was appropriate given the extensive nature of the lesion and the high recurrence rates associated with intralesional procedures in foot bones, which can reach up to 50% compared to 10–15% in long bones [2]. En masse resection and wide local resection, while being more radical procedures, provides superior local control by removing the tumor with an adequate margin of uninvolved tissue, thereby minimizing the risk of local recurrence that could necessitate amputation [2]. The reconstruction using hemifibular autograft represents an excellent choice for restoring structural integrity and function following segmental metatarsal resection. Fibular autografts offer several advantages, including excellent structural properties that match the cortical strength requirements of metatarsal reconstruction, reliable biological incorporation due to the autologous nature of the graft, and acceptable donor site morbidity [7]. Our technique of hemifibular technique specifically allows for preservation of fibular length while providing adequate cortical bone for reconstruction, maintaining both structural support and cosmetic appearance of the lower leg. The specific advantage of a hemifibular graft being the maintenance of the continuity of the fibula, which gradually remodels and attains its shape and strength. Studies have demonstrated successful union rates of 85–95% with fibular autografts in metatarsal reconstruction, with most patients achieving solid union within 12–24 months post-operatively [8]. The excellent functional outcome at 2-year follow-up in this case aligns with reported literature on medium to long-term results of fibular reconstruction for foot tumors. Toma et al. reported a series of six patients who underwent metatarsal reconstruction with free vascularized fibular grafts following malignant tumor resection, achieving a mean MSTS functional score of 82% at an average follow-up of 4.2 years [9]. The good functional result observed at 2 years is particularly encouraging as it suggests successful graft integration, restoration of foot biomechanics to near normal, and return to weight-bearing activities. The absence of local recurrence at this timepoint is also significant, as most GCT recurrences occur within the first 2–3 years following surgical treatment [2,6].
Compared to alternative reconstruction methods, such as allografts, prosthetic implants, or primary amputation, the hemifibular autograft approach offers superior long-term durability and functional outcomes both at the donor and recipient sites. Vascularized fibular grafts may offer faster incorporation and better remodeling potential for very large defects [10]. While non-vascularized fibular technique provides excellent results with reduced operative complexity and shorter surgical time [7,8]. The successful outcome in this case supports the use of en masse resection combined with hemifibular autograft reconstruction as an effective limb-salvage procedure for GCT of the metatarsal bones, offering patients excellent local control with preservation of foot function and avoiding the functional limitations associated with ray amputation. This being a single case report, the findings would be too pre-mature to generalize the treatment method and more such reports are needed to substantiate it. Another limitation for this study is the short duration of follow-up of 2 years and no comparative arm, since this is only a case report.
This case illustrates the aggressive GCT of the metacarpal bone managed by excision and reconstruction of the bone defect with hemi-fibular grafting. Hence, hemi-fibular grafting can be considered as an innovative technical substitute to the traditional methods of autograft harvesting, with good regenerative potential at the donor site and better incorporation rates at the recipient site, providing good functional results. This case is being reported for the rarity of its occurrence and the success of the non-vascular hemifibular autograft.
The use of hemifibular autograft for reconstruction of metatarsal bone has the clear advantage of minimal donor site morbidity, successful autograft incorporation, and salvage of the 5th ray with good functional outcome
References
- 1. Raskin KA, Schwab JH, Mankin HJ, Springfield DS, Hornicek FJ. Giant cell tumor of bone. J Am Acad Orthop Surg 2013;21:118-26. [Google Scholar] [PubMed]
- 2. Rajani R, Schaefer L, Scarborough MT, Gibbs CP. Giant cell tumors of the foot and ankle bones: High recurrence rates after surgical treatment. J Foot Ankle Surg 2015;54:1141-5. [Google Scholar] [PubMed]
- 3. Abed Alharbi W, Mohammed Alshareef H, Hennawi YB, Munshi AA, Khalid Alzahrani A. Giant cell tumor in tarsal midfoot bones: A case report. Cureus 2024;16:e56215. [Google Scholar] [PubMed]
- 4. Chaudhary SD, Agrawal PS, Sakharkar NS. Giant cell tumor of talus: A case report. J Orthop Case Rep 2022;12:92-4. [Google Scholar] [PubMed]
- 5. Fan QH, Long S, Wu XK, Fang Q. Management of a rare giant cell tumor of the distal fibula: A case report. World J Clin Cases 2023;11:394-400. [Google Scholar] [PubMed]
- 6. Prashant K, Bhattacharyya TD, Frank HC, Ram P. An unusual case of giant cell tumor of first metatarsal: a rare case report and review of literature. J Orthop Case Rep. 2016;6(3):91-4. [Google Scholar] [PubMed]
- 7. Rengsen P, Tiong KL, Teo YM, Goh TC, Sivapathasundram N. Reconstruction of the Second Metatarsal with Non-vascularised Fibular Graft following En-bloc Resection for Giant Cell Tumour: A Case Report. Malays Orthop J. 2013;7(3):47-50 [Google Scholar] [PubMed]
- 8. Hara H, Akiyama T, Takemura Y, Imura S. Reconstruction of the Midfoot Using a Free Vascularized Fibular Graft After En Bloc Excision for Giant Cell Tumor of the Tarsal Bones: A Case Report. J Foot Ankle Surg. 2016;55(4):867-71. [Google Scholar] [PubMed]
- 9. Toma CD, Dominkus M, Pfeiffer M, Giovanoli P, Assadian O, Kotz R. Metatarsal reconstruction with use of free vascularized osteomyocutaneous fibular grafts following resection of malignant tumors of the midfoot: a series of six cases. J Bone Joint Surg Am. 2007;89(7):1553-64. [Google Scholar] [PubMed]
- 10. Bumbasirevic M, Stevanovic M, Bumbasirevic V, Lesic A, Atkinson HD. Free vascularised fibular grafts in orthopaedics. Int Orthop. 2014 Jun;38(6):1277-82. doi: 10.1007/s00264-014-2281-6. Epub 2014 Feb 22. PMID: 24562850; PMCID: PMC4037521. [Google Scholar] [PubMed] [CrossRef]










