Organic foreign bodies such as thorns should always be suspected in atypical pediatric hand masses with bony changes.
Dr. Maradona Mncedisi Mashigo, Department of Orthopaedic Surgery, University of the Witwatersrand, 7 York Road, Parktown, Johannesburg, 2193, South Africa. E-mail: mashigo.gab1@gmail.com
Introduction: Retained foreign bodies in pediatric hand injuries are rare but can lead to significant complications if undiagnosed. Organic foreign bodies, such as tree thorns, are often radiolucent and may not be detected on plain radiographs, making diagnosis challenging. This case highlights the importance of considering a retained foreign body in a child presenting with a persistent hand mass and associated bony changes.
Case Report: A 3-year-old male presented with a painless, slow-growing mass over the dorsal ulnar aspect of his left hand for 8 weeks. Clinical examination revealed a fluctuant, non-tender mass without overlying skin changes. Radiographs showed a periosteal reaction with a lytic lesion on the metacarpal bone, and ultrasonography revealed a hyperechoic foreign structure within a cystic collection. The patient underwent surgical removal of the foreign body and debridement. Intraoperatively, a conical tree thorn measuring 1.0 cm was identified and removed. Post-operative recovery was uneventful, and the patient showed complete resolution of symptoms. Histopathology confirmed a foreign body granulomatous reaction.
Conclusion: Organic foreign bodies should be considered in pediatric hand masses with associated bony changes. Ultrasonography plays a crucial role in diagnosis, particularly when radiographs are inconclusive. A multidisciplinary approach, including imaging, surgical intervention, and postoperative care, ensures optimal outcomes.
Keywords: Organic foreign body, thorn injury, hand mass, pediatric.
Penetrating injuries from thorns and other organic materials are frequently encountered in children but are often underdiagnosed due to their radiolucent nature. Plain radiographs typically fail to show the retained object, and the resulting osseous or soft tissue reactions can mimic neoplastic or infective processes such as a bone cyst, tuberculosis, or chronic osteomyelitis [1,2]. The delayed presentation is further complicated by the fact that patients and families frequently fail to remember the inciting trauma or event [3]. The biological response to retained organic material involves a granulomatous foreign body reaction that may cause periosteal reaction, osteolysis, or chronic inflammatory masses [4]. Ultrasonography has emerged as the most reliable first-line modality for detecting these radiolucent objects, while computed tomography (CT) and magnetic resonance imaging (MRI) can further delineate the associated soft-tissue changes [3,5]. Recent innovations such as dark-field radiography have also shown promise in detecting wooden splinters otherwise invisible on conventional imaging [6]. With this background, we present a pediatric case of a retained tree thorn in the hand manifesting as a cystic lesion, highlighting the diagnostic challenges and value of ultrasound in guiding successful surgical management.
A 3-year-old male presented to our orthopedic outpatient clinic, referred from a local clinic, with a painless slow slow-growing mass over the dorsum ulna aspect of his left hand for the past 8 weeks. The was no report of decline in hand function. The were no associated symptoms such as fever, night sweats, and/or recent significant weight loss. His mother gave a history that 2 months ago the child had fallen on a tree with thorns while playing at home, and he presented to a local clinic complaining of left-hand pain after the incident. He was treated with analgesia and put on a 10-day course of flucloxacillin. On examination, there was a well-defined soft-tissue swelling over the dorsal ulnar aspect of the hand overlying the 5th and 4th metacarpal bones without any changes of the overlying skin. The mass was fluctuant and non-tender (Fig. 1). There was no hyperthermia over the mass, and it was not pulsatile to the touch.

Figure 1: Pre-operative image of the left hand. Showing dorsal mass.
A radiograph of the hand showed periosteal reaction with a lytic lesion with well-defined borders over the ulna cortex of the metacarpal bone of the left ring finger (Fig. 2).
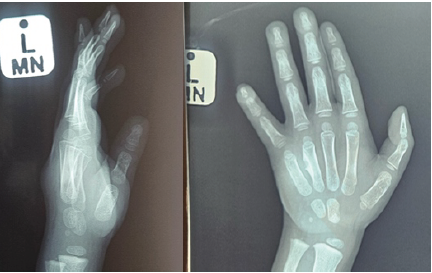
Figure 2: Left hand anteroposterior (AP) and lateral radiographs. Showing 4th metacarpal bony changes. AP X-ray shows the “crab claw” sign.
On ultrasonography of the hand of the hand an elongated linear hyperechoic foreign structure measuring 1.07 cm long lying within a cystic collection that measured 2.02 cm × 1.31 cm with no vascularity changes (Fig. 3). Hematological studies were all within normal limits except anemia of hemoglobin = 10.1 of note C-reactive protein was normal.
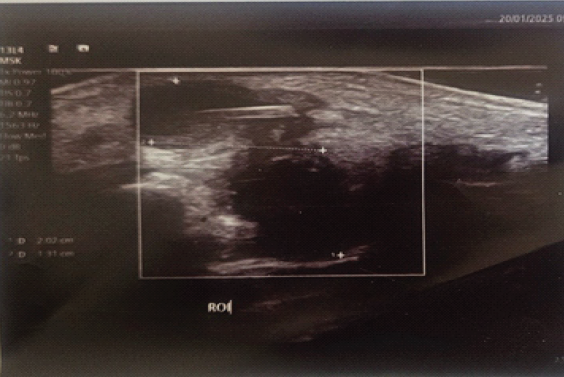
Figure 3: Ultrasonography of the hand of the hand an elongated linear hyperechoic foreign structure measuring 1.07 cm long lying within a cystic collection that measured 2.02 cm × 1.31 cm with no vascularity changes.
Based on the above, a diagnosis of a retained foreign body of the left hand was made, and the patient was booked on the emergency theater list and was taken for removal of the foreign body and debridement. A coned-shaped thorn measuring 1.0 cm was removed from the dorsum aspect of the hand intraoperatively (Fig. 4). At 2-week follow-up, the surgical wound had healed completely. Histological results confirmed a granulomatous foreign body reaction. The child had an excellent clinical outcome with resolution of swelling, full function of the hand, and no complications to report.

Figure 4: A conned-shaped thorn measuring 1.0 cm was removed from the dorsum aspect of the hand intraoperatively.
Retained organic foreign bodies in the hand are diagnostically challenging due to their radiolucency on plain radiographs and their ability to mimic tumors or infective lesions. Our case presented with both periosteal reaction and a lytic lesion, consistent with previously described variable osseous responses. Benzarti et al. described the characteristic “crab claw” periosteal reaction to thorns [7], while Regmi et al. highlighted that palm or plant thorns can cause pseudotumoral bone changes and chronic osteomyelitis [8]. In our case, the history of a fall onto a thorn aided suspicion, but as other authors note, such antecedent trauma history is often forgotten or not volunteered, leading to misdiagnosis and inappropriate initial management [8,9]. Imaging remains central in identifying these lesions. While CT and MRI imaging can delineate foreign bodies and associated reactions, their use is limited in children due to cost and radiation exposure risk [6]. Ultrasonography has emerged as the most practical tool, with reported sensitivities between 50 and 90% [10]. In our case, ultrasound clearly demonstrated a linear hyperechoic structure within a cystic collection, providing decisive confirmation when radiographs were inconclusive. This supports findings from Kawalec et al., who showed ultrasound to be highly valuable for detecting non-radiopaque foreign bodies in children [10]. Hwang et al. further caution that migration of foreign bodies is possible, underscoring the importance of careful pre-operative imaging and exploration [11]. Management principles emphasize the timely surgical exploration and removal of foreign bodies to prevent granulomatous inflammation, osteomyelitis, or sequestrum formation. Argarwal’s series of 24 cases showed uneventful recovery after removal across diverse materials [9], and Liaw’s case in a diabetic patient showed the risks of delayed recognition, including septic arthritis and osteomyelitis [12]. Our patient underwent prompt exploration with complete recovery, and histology confirmed a granulomatous reaction, consistent with literature reports. Taken together, our findings reinforce that organic foreign bodies should always be considered in atypical pediatric hand masses with bony changes, and that ultrasound-guided diagnosis coupled with early exploration and removal offers optimal outcomes.
Organic foreign bodies should be considered in pediatric hand masses with associated radiological bony changes. The role of ultrasonography remains crucial in the diagnosis of retained foreign bodies, guiding surgical management. A multidisciplinary approach that involves imaging, surgical intervention, and post-operative treatment is crucial for optimal outcomes.
Early suspicion, ultrasound diagnosis, and prompt exploration and removal of retained thorns in pediatric hands can prevent misdiagnosis and long-term complications.
References
- 1. Gupta M, Kumar D, Jain VK, Naik AK, Arya RK. Neglected thorn injury mimicking soft tissue mass in a child: A case report. J Clin Diagn Res 2015;9:RD03-4. [Google Scholar] [PubMed]
- 2. El Bouchti I, Ait Essi F, Abkari I, Latifi M, El Hassani S. Foreign body granuloma: A diagnosis not to forget. Case Rep Orthop 2012;2012:439836. [Google Scholar] [PubMed]
- 3. Ipaktchi K, DeMars A, Park J, Ciarallo C, Livermore M, Banegas R. Retained palmar foreign body presenting as a late hand infection: Proposed diagnostic algorithm to detect radiolucent objects. Patient Saf Surg 2013;7:25. [Google Scholar] [PubMed]
- 4. Chandorkar Y, Ravikumar K, Basu B. The Foreign body response demystified. ACS Biomater Sci Eng 2019;5:19-44. [Google Scholar] [PubMed]
- 5. Badran S, Mohammed M, Wani I, Hammouda A, Al-lahham S. Date palm thorn injury: A literature review and a case study of extensive hand haematoma. Cureus 2021;13:e13252. [Google Scholar] [PubMed]
- 6. Braig EM, Birnbacher L, Schaff F, Gromann L, Fingerle A, Herzen J, et al. Simultaneous wood and metal particle detection on dark-field radiography. Eur Radiol Exp 2018;2:1. [Google Scholar] [PubMed]
- 7. Benzarti S, Kaziz H, Triki MA, Mouelhi T, Ayeche ML Ben, Naouar N. An unusual bone reaction to a retained organic foreign body in the hand. Int J Orthop Sci 2018;4:948-50. [Google Scholar] [PubMed]
- 8. Regmi M, Desai S, Patwardhan S, Deshmukh W, Kapoor T, Patil N. Foreign body induced osteomyelitis in the hand – commonly missed clinical and radiological diagnosis. J Orthop Case Rep 2021;11:80-3. [Google Scholar] [PubMed]
- 9. Agarwal A. Foreign body-related extremity trauma in children: A single-center experience. Indian J Orthop 2018;52:481-8. [Google Scholar] [PubMed]
- 10. Kawalec AM. Use of ultrasound in differential diagnosis of soft tissue foreign bodies in children – a case series. Pediatr Pol 2023;98:180-4. [Google Scholar] [PubMed]
- 11. Hwang JH, Lee DG, Kim KS, Lee SY. Proximal migration of retained pencil lead along a flexor tendon in the hand: A case report. Medicine (Baltimore) 2019;98:E13876. [Google Scholar] [PubMed]
- 12. Liaw F, Murray O, Tan YY, Hems T. Retained Foreign body in a diabetic patient’s hand. Open Orthop J 2018;12:203-7. [Google Scholar] [PubMed]






