The integrated approach of simultaneously reconstructing ligaments, repairing meniscus, and restoring cartilage contributes to their reciprocal biological and biomechanical healing, thereby decreasing the likelihood of long-term knee arthritis. Although the risk of knee stiffness is elevated, diligent rehabilitation protocols typically lead to favorable post-operative results.
Dr Ankit Chaubey, Department of Orthopedics, Apex Superspeciality Hospital, Varanasi, Uttar Pradesh, India. Email: drankitchaubey@gmail.com
Introduction: The incidence of associated cartilage and meniscal pathology with anterior cruciate ligament (ACL) tears varies widely in the literature. Lateral meniscus posterior root tears (LPRTs) were more likely to occur with an ACL tear than medial meniscus posterior root tears, which were more likely to have concomitant knee chondral defects than LPRTs. The medial femoral condyle is the most common location reported overall; however, lateral femoral condyle defects are also reported in both acute and chronic cases. Repair of meniscal root injuries is the treatment of choice with the aim of restoring joint kinematics, contact pressures, and delaying the development of osteoarthritis. Articular cartilage injury associated with ACL reconstruction possibly has the greatest single effect on long-term subjective outcomes. However, compared with meniscal pathology, the volume of literature focused on treatment of chondral defects in conjunction with ACL reconstruction is significantly inferior.
Case Report: A case of 37-year-old male patient presented with pain and instability of the left knee since past 3 month following twisting injury of knee while slipping off stairs. Clinically, he was having medial joint line tenderness, positive Lachman and anterior drawer test, positive grade 2 pivot shift, and full range of motion (ROM) of knee. He underwent arthroscopic ACL reconstruction with semitendinosus graft, medial meniscus root repair by suture pull out technique, and mosaicplasty (2 plug, 6 mm) for medial femoral condyle cartilage defect of size (1.5 × 1.5 cm, International Cartilage Repair Society grade 4). Post-operative knee ROM was started from day 1 and he was kept on non-weight-bearing walking for 6 weeks. He was followed at 1 month, 3 month, and 6 month. Visual analog scale (VAS) score and International Knee Documentation Committee (IKDC) score were recorded at 3 and 6 months.
Result: His VAS score at 3 and 6 month was 2 and 0, respectively. IKDC score pre-operative was 34.5 which improved to 86.2 at 6-month follow-up.
Conclusion: Single-stage ACL reconstruction along with meniscal and chondral injury repair to be done to achieve good functional outcome. Meniscal root repair also prevents ACL reconstruction failure. Despite these observations, further study is needed to know the complex factors involved in optimizing patient outcomes in the setting of ACL insufficiency with concomitant meniscal or chondral injury.
Keywords: Anterior cruciate ligament reconstruction, medial meniscus root repair, mosaicplasty
Anterior cruciate ligament (ACL) tear is common in sport activities and accidents. High percentages of these injuries are associated with meniscal, ligament, or chondral injuries [1]. Articular cartilage injury in the knee may be found alone, but it is mostly accompanied with injuries to the ligaments and menisci [2]. Articular cartilage does not usually regenerate after injury or disease, leading to loss of tissue and formation of a defect [3]. Repair of meniscal root injuries is the treatment of choice with the aim of restoring joint kinematics, contact pressures, and delaying the development of osteoarthritis. The volume of literature focused on treatment of chondral defects in conjunction with ACL reconstruction is significantly inferior. We did not find any case report of single-stage treatment of medial meniscus root tear (MMRT) and chondral lesion in conjunction with ACL tear in literature.
We present a case of 37-year-old male patient presented with pain and instability of left knee since past 3 month following twisting injury of knee while slipping off stairs
- Clinically
- Medial joint line tenderness
- Positive Lachman
- Anterior drawer test grade II
- Positive pivot shift
- Full range of motion (ROM) of knee with terminal painful.
His magnetic resonance imaging (MRI) left knee revealed complete ACL tear from femoral site with MMRT with infolding of meniscus lying in meniscotibial recess and grade 4 chondral defect at medial femoral condyle of size 1.5 × 1.5 cm (Fig. 1).
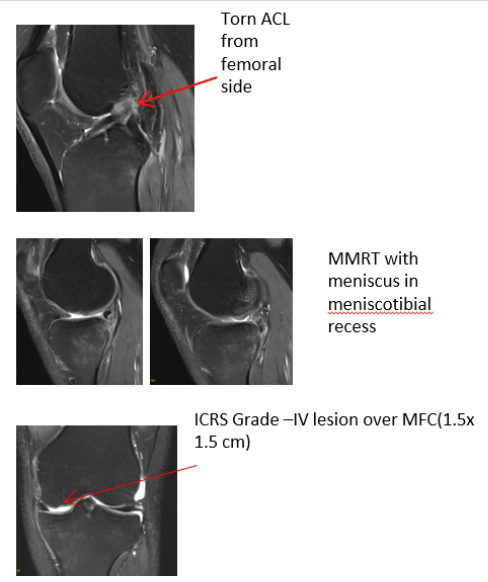
Figure 1: Anterior cruciate ligament tear, medial meniscus root tear, and cartilage defect over medial femur condyle.
Under spinal anesthesia standard anterolateral and anteromedial (AM) portal made in left knee, medial meniscus which was lying meniscotibial recess liberated with labral elevator and then after by transtibial pullout technique root repair done. ACL reconstruction done with quadrupled semitendinosus graft by transportal technique. Anterolateral portal incision extended by 1 cm and from lateral femoral condyle 6 mm two osteochondral plug harvested and then after we extended AM portal incision by 1 cm and recipient medial femoral condyle cartilage deficit area prepared and osteochondral plug implanted (Fig. 2).
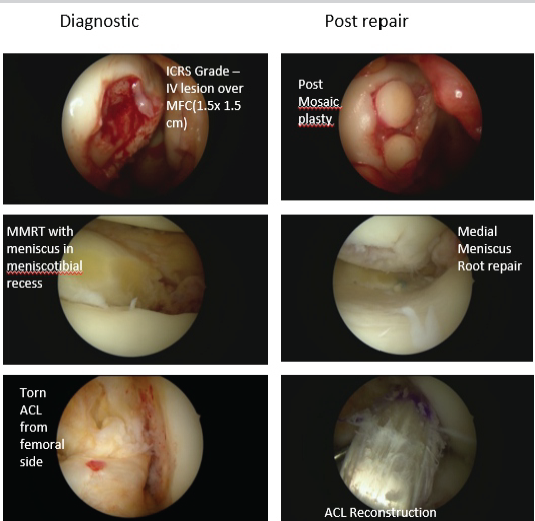
Figure 2: Co-existing lesion pre- and post-repair.
Knee ROM started after 3 week post-operative and full-weight-bearing walking allowed after 2 months. No squatting and crossed leg sitting allowed for 6 months. At 6 month, his visual analog scale score was 0 and International Knee Documentation Committee (IKDC) score 86.2 (Fig. 3).
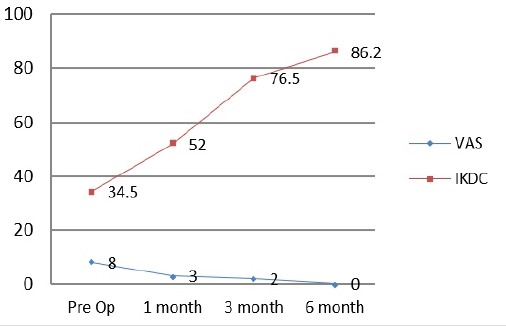
Figure 3: Visual analog scale score and International Knee Documentation Committee score during follow-up.
At 1 year follow-up, we did MRI of knee and found good incorporation of ACL graft with meniscus root healing and cartilage restoration with magnetic resonance observation of cartilage repair tissue score 90/100 (Fig. 4).
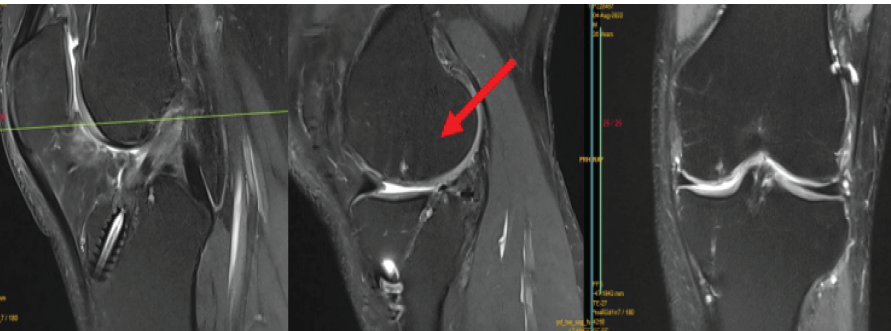
Figure 4: Magnetic resonance imaging at 12-month follow-up showing healing and cartilage restoration.
The diversity of meniscal tear patterns encountered in the ACL-deficient knee adds complexity to the treatment decision-making process, and questions still exist regarding the optimal strategies for maximizing outcomes. Approximately 50% of primary ACL ruptures and over 90% of failed reconstructions will have coexisting cartilage and/or meniscal pathology [4]. In terms of location, 95% and 77% of medial and lateral menisci, respectively, involve the posterior horn. Association of posterolateral meniscus root in conjunction with ACL tears is approximately 8–14%. Conversely, posteromedial meniscal root avulsions are uncommonly observed with isolated ACL injury, although they have increased association with multiligament injuries [5,6]. The effects of peripheral longitudinal posterior horn medial meniscal tears (mean 28 mm length tear) in the setting of ACL deficiency were evaluated by Ahn et al. [7] and findings included significant increases in anterior translation with simulated Lachman maneuvers at flexion angles up to 60 (P = 0.05) but no differences with pivot shift. Furthermore, the peripheral tear resulted in the same degree of instability as a total medial meniscectomy. After meniscal repair, however, stability was restored to the isolated ACL-deficient state. High-level clinical evidence on the effect of meniscal integrity on post-operative stability is also lacking. One level III review of 482 patients at mean 7.6 years postoperatively found significantly higher KT-1000 side-to-side differences in patients with any medial meniscal resection compared with intact medial menisci (2.6 6 1.7 vs. 2.0 6 1.5 mm; P = 0.0065), but no differences in graft failures were reported [8]. In a recent level III study with median follow-up 26 months, 118 patients were evaluated after anatomic single bundle hamstring tendon autograft ACL reconstruction. The investigators found that medial and lateral meniscal deficiency were the highest risk factors for graft failure (medial: Hazard ratio, 15.1; Confidence interval (CI), 4.7–48.5; P = 0.001, lateral: Hazard ratio, 9.9, CI, 3–33; P = 0.001) [9]. A large level II cohort of 4,691 patients with 2-year follow-up found that only medial meniscal repairs had significantly worse knee injury and osteoarthritis outcome score subscales compared with isolated ACL reconstructions (Symptoms: b = 22.5; CI, 24.6–20.5; P = 0.023, Quality of Life: b = 23.8; CI, 26.8–21; P = 0.009) [10]. However, all other treatments had no effect, including any lateral meniscal intervention. Røtterud et al. [11] in nationwide cohort study from Norway and Sweden of 8476 patients with 2-year follow-up found no stastically significant difference in outcome with patient with medial meniscus tear. Two level I prospective investigations [12,13], both reporting on data from the same pool of patients with 6-year follow-up, found, compared with uninjured menisci, worse patient-reported outcomes with medial meniscal repairs and improved outcomes with non-treatment of lateral meniscal tears. Articular cartilage injury associated with ACL reconstruction possibly has the greatest single effect on long-term subjective outcomes. In a large, level-III review of 2,770 patients, 4.5% were found to have an isolated high-grade chondral defect (treated with benign neglect, mean size 1.7 cm2) in the absence of meniscal pathology. Compared with a cohort without meniscal or chondral pathology, at mean follow-up 8.7 years, IKDC scores were statistically lower but differences were likely not clinically significant (medial: 1.2; P = 0.0451, lateral: 3.1; P = 0.0047) [14]. Contradictory to it level-III review with longer mean follow-up of 8.6 years found that both meniscal resections and chondral defects were associated with worse subjective outcomes [8]. High-level studies evaluating ACL reconstruction with concurrent cartilage repair are lacking. Techniques described include chondroplasty, microfracture, autologous chondrocyte implantation, and osteochondral autograft/allograft transplantation. A prospective, randomized level II (non-blinded) study comparing osteochondral autograft transplantation, microfracture, and debridement of high-grade defects (mean, 2.6 cm2) in conjunction with ACL reconstruction found at mean 36-month follow-up superior results with osteochondral autograft transplantation compared with microfracture [15].
Optimizing long-term outcomes in treating ACL tears with associated chondral and meniscal pathology requires an understanding of both the natural history of specific pathology and the results of various treatment modalities. Meniscal tears and previous partial meniscectomies have higher associations with corresponding compartmental chondral defects in both primary and revision ACL reconstructions. Benign neglect of stable meniscal tears in association with ACL reconstruction leads to generally acceptable outcomes; however, medial meniscal tears left in situ are associated with higher revision surgery rates than lateral tears. The presence of chondral defects consistently results in lower intermediate-to-long-term patient-reported outcomes. Despite these observations, further study is needed to elucidate the complex factors involved in optimizing patient outcomes in the setting of ACL insufficiency with concomitant meniscal or chondral injury.
The occurrence of concomitant cruciate, meniscus, and cartilage injuries is not rare, and a comprehensive clinical assessment along with a thorough pre-operative MRI evaluation is essential to identify these complex injuries and tailor the surgical approach accordingly.
References
- 1. Magosch A, Mouton C, Nührenbörger C, Seil R. Medial meniscus ramp and lateral meniscus posterior root lesions are present in more than a third of primary and revision ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 2021;29:3059-67. [Google Scholar] [PubMed]
- 2. Brophy RH, Zeltser D, Wright RW, Flanigan D. Anterior cruciate ligament reconstruction and concomitant articular cartilage injury: Incidence and treatment. Arthroscopy 2010;26:112-20. [Google Scholar] [PubMed]
- 3. Shekhar AP, Tapasvi SR. Management of chondral defects of the knee. In: Hardikar SM, editor. Hardikar’s Operations: Text and Atlas. New Delhi: Jaypee Brothers Medical Pvt. Ltd.; 2019. p. 91-105. [Google Scholar] [PubMed]
- 4. Kluczynski MA, Marzo JM, Bisson LJ. Factors associated with meniscal tears and chondral lesions in patients undergoing anterior cruciate ligament reconstruction: A prospective study. Am J Sports Med 2013;41:2759-65. [Google Scholar] [PubMed]
- 5. Frank JM, Moatshe G, Brady AW, Dornan GJ, Coggins A, Muckenhirn KJ, et al. Lateral meniscus posterior root and meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: A biomechanical study. Orthop J Sports Med 2017;5:2325967117695756. [Google Scholar] [PubMed]
- 6. Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: Significance, diagnosis, and treatment. Am J Sports Med 2014;42:3016-30. [Google Scholar] [PubMed]
- 7. Ahn JH, Bae TS, Kang KS, Kang SY, Lee SH. Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am J Sports Med 2011;39:2187-93. [Google Scholar] [PubMed]
- 8. Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. Five- to fifteen-year evaluations. Am J Sports Med 2000;28:446-52. [Google Scholar] [PubMed]
- 9. Parkinson B, Robb C, Thomas M, Thompson P, Spalding T. Factors that predict failure in anatomic single-bundle anterior cruciate ligament reconstruction. Am J Sports Med 2017;45:1529-36. [Google Scholar] [PubMed]
- 10. LaPrade CM, Dornan GJ, Granan LP, LaPrade RF, Engebretsen L. Outcomes after anterior cruciate ligament reconstruction using the Norwegian knee ligament registry of 4691 patients: How does meniscal repair or resection affect short-term outcomes? Am J Sports Med 2015;43:1591-7. [Google Scholar] [PubMed]
- 11. Røtterud JH, Sivertsen EA, Forssblad M, Engebretsen L, Arøen A. Effect of meniscal and focal cartilage lesions on patient-reported outcome after anterior cruciate ligament reconstruction: A nationwide cohort study from Norway and Sweden of 8476 patients with 2-year follow-up. Am J Sports Med 2013;41:535-43. [Google Scholar] [PubMed]
- 12. Cox CL, Huston LJ, Dunn WR, Reinke EK, Nwosu SK, Parker RD, et al. Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? A 6-year multicenter cohort study. Am J Sports Med 2014;42:1058-67. [Google Scholar] [PubMed]
- 13. Dunn WR, Wolf BR, Harrell FE Jr., Reinke EK, Huston LJ, MOON Knee Group, et al. Baseline predictors of health-related quality of life after anterior cruciate ligament reconstruction: A longitudinal analysis of a multicenter cohort at two and six years. J Bone Joint Surg Am 2015;97:551-7. [Google Scholar] [PubMed]
- 14. Shelbourne KD, Jari S, Gray T. Outcome of untreated traumatic articular cartilage defects of the knee: A natural history study. J Bone Joint Surg Am 2003;85-A Suppl 2:8-16. [Google Scholar] [PubMed]
- 15. Gudas R, Gudaite A, Mickevicius T, Masiulis N, Simonaitytė R, Cekanauskas E, et al. Comparison of osteochondral autologous transplantation, microfracture, or debridement techniques in articular cartilage lesions associated with anterior cruciate ligament injury: A prospective study with a 3-year follow-up. Arthroscopy 2013;29:89-97. [Google Scholar] [PubMed]