Successful treatment of chronic humeral shaft non-union with a combination of proximal tibia cancellous autograft and structural allograft, without the need for free vascularized bone grafts or staged procedures.
Dr. Greco Victor. Allegheny Health Network Department of Upper Extremity Surgery 1307 Federal St, 2nd Floor, Pittsburgh, PA 15212. E-mail: victor.greco@ahn.org
Introduction: Humeral shaft non-unions can pose a difficult challenge to orthopedic surgeons. There are various techniques to approach these injuries, but some require microsurgical techniques or staged procedures.
Case Report: A 41-year-old woman presented with a 5-year-old humeral shaft non-union after previous open reduction and internal fixation complicated by infection. This was successfully treated surgically using a combination of proximal tibia cancellous autograft and structural allograft. Postoperatively, she had pain-free range of motion that was symmetric to her contralateral side.
Conclusion: Chronic humeral shaft non-unions may be successfully treated with a combination of tibial cancellous autograft and structural allograft.
Keywords: Humeral shaft non-union, fibular strut, allograft.
Humeral shaft fractures are a common orthopedic injury accounting for 3–5% of all fractures in adults [1]. Many can be managed conservatively, while others require surgical intervention [2]. Occasionally, treatment of these fractures can be complicated by non-union. Non-union rates range from 2 to 10% for fractures treated conservatively, and 10–15% for those treated surgically [3,4,5]. When encountered, humeral shaft non-unions can be addressed in a multitude of ways, including cortical strut allografts, bone grafting, induced membrane technique, and vascularized bone transfer [6]. Despite a multitude of options, there remains no clear consensus on optimal treatment. To date, there are no reports on the use of tibial autograft and fibula allograft in the setting of humeral shaft non-unions. This report presents a case of a 5-year-old humeral shaft non-union treated successfully with a combination of proximal tibia autograft and cortical strut allograft.
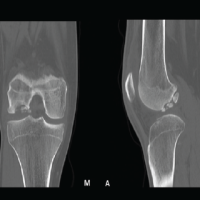
A 41-year-old female presented to the orthopedic clinic with complaints of chronic right arm pain and disability. The patient had a history of previous right humeral shaft fracture treated with an intramedullary nail 5 years prior. This was then complicated by infection. The nail was explanted, the wound irrigated, and the patient was put on IV antibiotics. After nail explanation, the patient did not receive any further orthopedic surgical intervention. Of note, the patient had a medical history significant for bulimia and alcoholism at the time of her initial treatment. On examination, the patient was neurovascularly intact with a well healed surgical incision. The patient had gross motion about her previous fracture site and was unable to extend her arm as a singular unit. Radiographs demonstrated an atrophic non-union about the humeral shaft (Fig. 1).
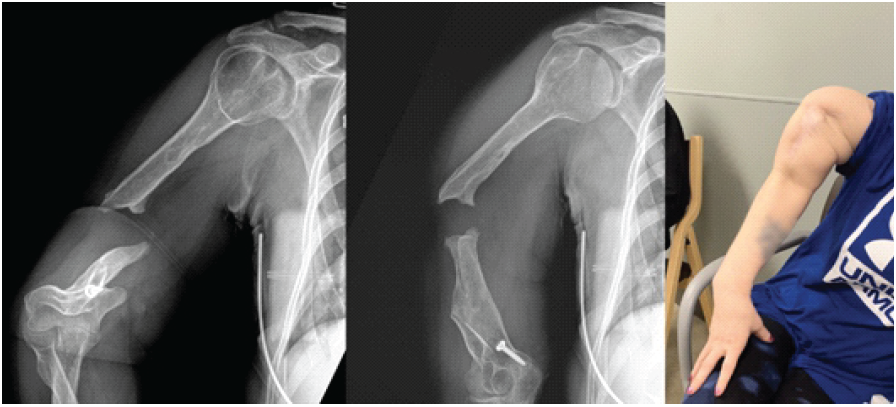
Figure 1: Pre-operative radiographs and clinical photo; pre-operative anteroposterior and attempted lateral radiographs of the right humerus illustrating a humeral shaft non-union. Pre-operative clinical photo demonstrating the instability of the humeral non-union.
Before operative intervention, nutritional laboratories, inflammatory markers, drug test, alcohol, and cotinine levels were evaluated, which all returned normal. The patient was scheduled for revision open reduction and internal fixation with bone grafting.
Surgical technique
The patient was positioned supine on a flat Jackson table with the operative arm and contralateral leg prepped and draped. We began by harvesting proximal tibial autograft. Under fluoroscopy, a 2 cm incision was centered over the anterolateral aspect of the tibia. Skin and subcutaneous tissues were dissected down to the tibia and an opening cortectomy was made. The AVITUS harvesting suction device was then used under fluoroscopic guidance to retrieved approximately 20 cc of cancellous graft, which was separated from the marrow. The defect was then back filled with 10 cc of tricalcium phosphate bone cement (Fig. 2).
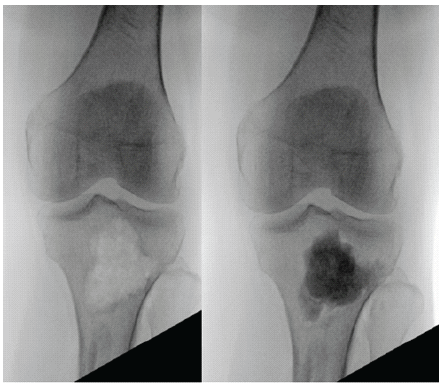
Figure 2: Proximal tibia after graft harvest and after cement backfilling; intraoperative anteroposterior fluoroscopy of the proximal tibia after allograft harvest and after backfilling with bone cement.
Hemostasis was achieved and the wound was then closed. The humeral shaft non-union was then addressed. A sterile tourniquet was placed and the humerus was approached through the previous anterolateral scar. Dissection was taken down to the humerus and no gross purulence or signs of active infection were present. Both ends of the humeral shaft non-union appeared to be necrotic. These ends were resected to healthy, bleeding bone, and sent for biopsy and culture. A fibular strut was then cut to fit into the canal of the humerus. The fibular strut was then placed and the two ends of the humeral non-union were aligned (Fig. 3).
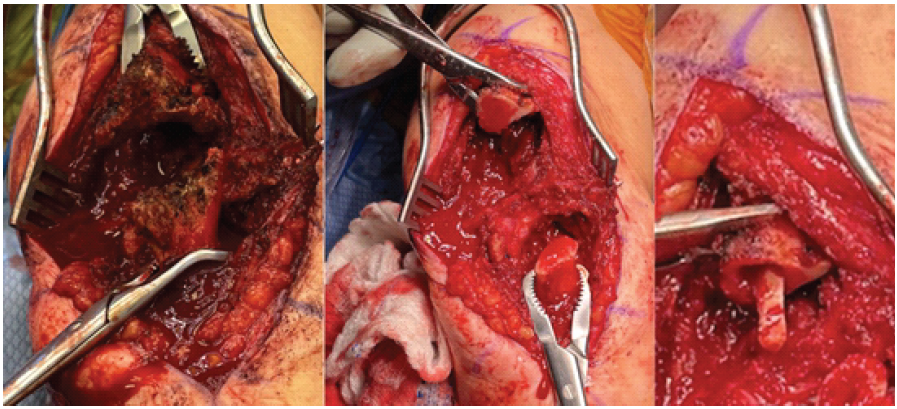
Figure 3: Intraoperative photographs of humeral non-union and allograft insertion; intraoperative photograph demonstrating the humeral shaft non-union before (left) and after (middle) resection to healthy bone. Intraoperative photograph demonstrating fibular strut allograft inside of the humeral canal (right).
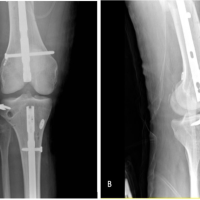
The shaft was then preliminarily fixed with a 2.7 mm plate and arm rotation was checked. A second, 3.5 mm plate was then added for further stability (Fig. 4).
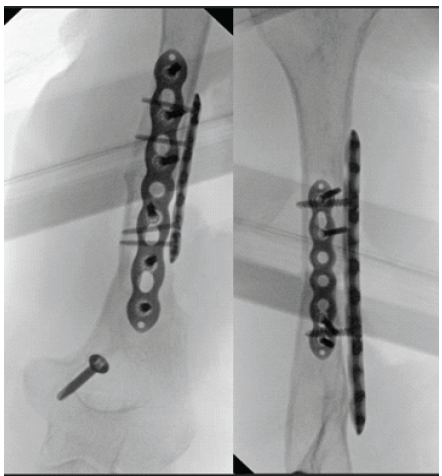
Figure 4: Intraoperative anteroposterior and lateral fluoroscopy of the humeral non-union fixation; intraoperative anteroposterior and lateral fluoroscopic images of the humeral non-union after fixation and grafting.
The previously harvested tibial bone graft was then mixed with cancellous chips and placed around the non-union site. The skin and subcutaneous tissues were closed and the patient was placed into a sling. The patient was admitted postoperatively and discharged in stable condition. The bone biopsy was read as benign bone and final bone cultures remained negative. The patient was initially made partial weight-bearing to graft donor site leg with plans to keep this limitation for 6 weeks postoperatively. However, the patient returned on her first clinic visit 2 weeks postoperatively ambulating without assistive device. The patient was seen in clinic routinely with radiographs at each visit and by her 9-month post-operative clinic visit, the cortical graft incorporated, and bony callus was apparent on radiographs (Fig. 5). The patient regained pain free range of motion that was symmetric to the contralateral side (Fig. 6.)
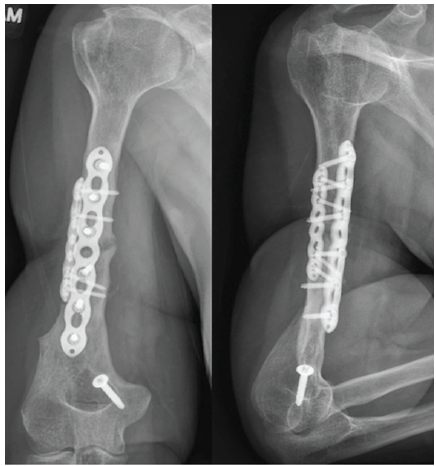
Figure 5: Post-operative anteroposterior and lateral radiographs at 9 months post-operative clinic visit; post-operative anteroposterior and lateral radiographs 9 months after humeral shaft non-union takedown and open reduction and internal fixation.

Figure 6: Patient’s range of motion at in office follow-up; post-operative photographs demonstrating patient’s abduction and forward flexion of the operative extremity at a follow-up clinic appointment.
Humeral shaft non-unions can pose a difficult challenge for orthopedic surgeons. Surgical scarring, patient biology, and bone loss can all contribute to the complexity of these cases. There is no consensus on the optimal treatment of humeral shaft non-unions; however, many techniques have been described. Fisher and Vanpoulle both describe successful treatment of humeral shaft non-unions with the induced membrane technique [7,8]. This is an enticing option in the setting of infection; however, the need for a second procedure may be viewed as a potential disadvantage. The use of a vascularized fibula graft is an alternative option that eliminates the need for a second procedure, but requires microsurgical instrumentation and surgical expertise [9,10]. Alternatively, the use of non-vascularized grafts offers a potential treatment option that does not require microsurgical technique. There are reports of successful treatment of humeral shaft non-unions using a variety of non-vascularized methods, including fibula allograft, iliac crest autograft, and femoral canal autograft through the reamer irrigator aspirator system [11,12,13]. However, to our knowledge, there are no reports of the use of proximal tibial autograft for humeral shaft non-unions. Proximal tibial autograft has been shown to be effective in treating non-unions in other orthopedic injuries [14,15,16]. It offers an alternative source of autograft that may provide large graft amounts with decreased early post-operative pain compared to iliac crest [17,18]. Our case demonstrates successful use of proximal tibial autograft, in combination with fibular strut allograft, to treat a humeral shaft non-union. It is the author’s preference to utilize proximal tibial autograft over the other alternatives. Potential advantages of this technique include ease of positioning, ease of access through a smaller incision, large graft volume, preservation of the hip abductors, and decreased post-operative pain at the harvest site compared to other techniques. Potential disadvantages are gait disturbances, need to limit weight bearing to the graft donor leg, and risk of tibial fracture.
This case report highlights a chronic humeral shaft non-union treated successfully with tibial cancellous autograft and fibular strut allograft. This highlights a biologically and biomechanically effective solution to a complex problem. Potential advantages of this technique include a single stage procedure without the need for microsurgical anastomoses, and a combination of osteogenic, osteoinductive, and osteoconductive properties at the non-union site.
Humeral shaft non-unions can be successfully treated with tibial cancellous autograft and fibular strut allograft, providing an alternative to other lengthy and surgically demanding procedures.
References
- 1. Carroll EA, Schweppe M, Langfitt M, Miller AN, Halvorson JJ. Management of humeral shaft fractures. J Am Acad Orthop Surg 2012;20:423-33. [Google Scholar] [PubMed]
- 2. Court-Brown CM, McQueen MM. Nonunions of the proximal humerus: Their prevalence and functional outcome. J Trauma 2008;64:1517-21. [Google Scholar] [PubMed]
- 3. Ring D, Chin K, Taghinia AH, Jupiter JB. Nonunion after functional brace treatment of diaphyseal humerus fractures. J Trauma 2007;62:1157-8. [Google Scholar] [PubMed]
- 4. Rutgers M, Ring D. Treatment of diaphyseal fractures of the humerus using a functional brace. J Orthop Trauma 2006;20:597-601. [Google Scholar] [PubMed]
- 5. Heim D, Herkert F, Hess P, Regazzoni P. Surgical treatment of humeral shaft fractures–the Basel experience. J Trauma 1993;35:226-32. [Google Scholar] [PubMed]
- 6. Naclerio EH, McKee MD. Approach to humeral shaft nonunion: Evaluation and surgical techniques. J Am Acad Orthop Surg 2022;30:50-9. [Google Scholar] [PubMed]
- 7. Fisher ND, Konda SR. Infected humeral shaft nonunion treatment with the induced membrane technique and a novel fixation construct: A case report: OTA Int 2023;7:285. [Google Scholar] [PubMed]
- 8. Vanpoulle G, Jalaguier T, Druel T, Walch A, Gazarian A, Mathieu L. Treatment of infected humeral shaft nonunion and presumed aseptic nonunion with positive intraoperative cultures: A retrospective single-center study. Eur J Trauma Emerg Surg 2024;50:2947-54. [Google Scholar] [PubMed]
- 9. Kerfant N, Valenti P, Kilinc AS, Falcone MO. Free vascularised fibular graft in multi-operated patients for an aseptic non-union of the humerus with segmental defect: Surgical technique and results. Orthop Traumatol Surg Res 2012;98:603-7. [Google Scholar] [PubMed]
- 10. Chhabra AB, Golish SR, Pannunzio ME, Butler TE Jr., Bolano LE, Pederson WC. Treatment of chronic nonunions of the humerus with free vascularized fibula transfer: A report of thirteen cases. J Reconstr Microsurg 2009;25:117-24. [Google Scholar] [PubMed]
- 11. Fink Barnes LA, Ruig DF, Freibott CE, Rajfer R, Rosenwasser MP. Treatment of nonunions of the humeral shaft with nonvascularized fibular strut allograft: Postoperative outcomes and review of a surgical technique. JSES Int 2020;4:739-44. [Google Scholar] [PubMed]
- 12. Stevens NM, Schultz BJ, Lowe DT, Egol KA. Repair of humeral shaft nonunion with plate and screw fixation and iliac crest bone graft. J Orthop Trauma 2021;35:S7-8. [Google Scholar] [PubMed]
- 13. De Carolis O, Mori CM, Vicenti G, Carrozzo M, Abate A, Caiaffa V. A lifelong story: Case report of a humeral shaft nonunion successfully treated after 30 years. Injury 2018;49 Suppl 4:S43-7. [Google Scholar] [PubMed]
- 14. Jia TY, Gurmeet S, Asni A, Ramanathan R. Proximal tibia bone graft: An alternative donor source especially for foot and ankle procedures. Malays Orthop J 2015;9:14-7. [Google Scholar] [PubMed]
- 15. Greco VE, Hammarstedt JE, O’Connor S, Regal S. Management of a 5-cm distal radius bone defect using the Masquelet technique with autograft harvested from the proximal tibia. J Orthop Case Rep 2022;12:50-4. [Google Scholar] [PubMed]
- 16. Jenkins S, Daji A, Fomunung C, Grunhut J, Sabesan V. Managing Recurrent Clavicle Nonunion and Construct Failure: A Case Report. Journal of Orthopaedic Experience & Innovation. 2023;4(1)1-8. [Google Scholar] [PubMed]
- 17. Salawu ON, Babalola OM, Ahmed BA, Ibraheem GH, Kadir DM. Comparative study of proximal tibia and iliac crest bone graft donor sites in treatment of orthopaedic pathologies. Malays Orthop J 2017;11:15-9. [Google Scholar] [PubMed]
- 18. Villarreal-Villarreal GA, Simental-Mendía M, Alonso AA, Vilchez-Cavazos F, Acosta-Olivo CA, Peña-Martínez VM. Comparison of anterior iliac crest versus proximal tibia autologous bone graft harvesting: A systematic review and meta-analysis. J Foot Ankle Surg 2023;62:388-97. [Google Scholar] [PubMed]