Complex volar carpometacarpal dislocations, particularly when associated with thumb interphalangeal injuries, require thorough clinical evaluation, precise imaging, and early multidisciplinary management to achieve optimal functional recovery.
Dr. Touré Layes, Bocar Sidi Sall Teaching Hospital, Kati, Mali. E-mail: layestoure854@gmail.com
Introduction: Carpometacarpal (CMC) dislocations are rare and usually result from high-energy trauma. The most frequent direction of dislocation is dorsal, even if the dorsal ligaments are stronger than the volar ones. We report a case of volar CMC dislocation with concomitant thumb interphalangeal injury.
Case Report: We report the case of a 30-year-old right-handed male who sustained a left volar CMC dislocation with an associated posterolateral interphalangeal dislocation of the thumb following a motorcycle accident. Clinical examination revealed dorsal concavity of the hand and a thumb deformity with a 2-cm open wound, while finger mobility and sensation were preserved. Standard radiographs confirmed the dislocations. The patient underwent wound debridement and closed reduction under general anesthesia, followed by immobilization with an anterior splint including the thumb. Complete wound healing was achieved by day 12, and the splint was removed at 45 days. Progressive active mobilization started in the 3rd post-operative week. At 3 months follow-up, the patient had full recovery of wrist and finger motion and returned to work at 8 weeks.
Conclusion: Early diagnosis, careful reduction, and structured rehabilitation are key in managing complex volar CMC dislocations with concomitant thumb injuries. Multidisciplinary management ensures optimal functional outcomes and prevents long-term disability.
Keywords: Carpometacarpal joint, hand injuries, finger phalanges.
Carpometacarpal (CMC) dislocations are uncommon, particularly in the four long fingers, and account for approximately 1% of all hand and wrist injuries [1]. They typically result from high-energy trauma in young adult males [1,2]. Complete dorsal dislocations are more frequent than volar dislocations and are often associated with metacarpal fractures, likely due to the greater strength of the dorsal ligaments compared to the volar ligaments [3]. We report the case of a 30-year-old patient who sustained a volar CMC dislocation of the hand associated with an open interphalangeal injury of the thumb.
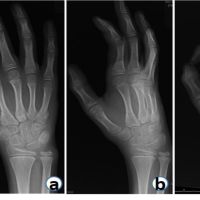
The patient was a 30-year-old right-handed male hotel worker with no significant medical history. He presented to the emergency department of a tertiary care hospital following an open injury to his left hand sustained in a motorcycle accident. According to reports, the patient was struck by a vehicle, and the wheel reportedly ran over his left hand. He experienced severe pain and complete functional impairment of the affected hand. On arrival, approximately 2 h after the injury, he was hemodynamically stable. Clinical examination revealed a dorsal concavity of the left hand, associated with a posterolateral deformity of the thumb at the interphalangeal joint, with exposure of the base of the distal phalanx through a 2-cm wound (Fig. 1). In addition, a superficial volar wound measuring approximately 7 cm, concave in shape, extended from the base of the third finger to the thumb, forming a conjoined palmar flap (Fig. 1). Finger mobility and sensation were preserved.
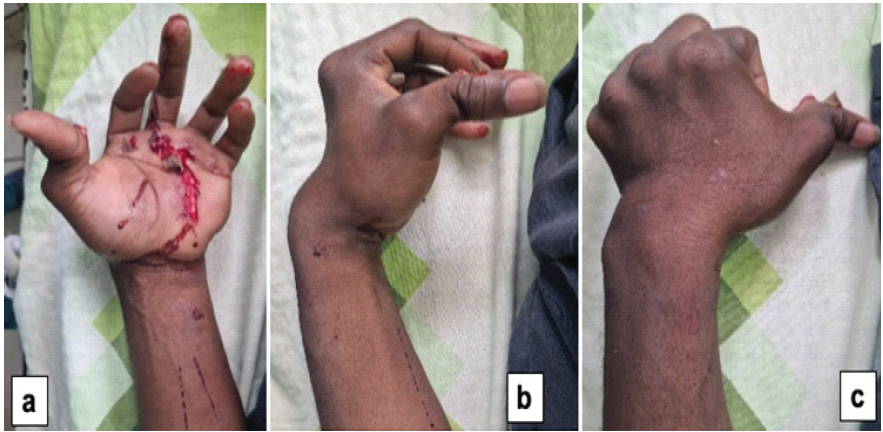
Figure 1: Clinical presentation of the left hand (a) Palmar side of the left hand showed a superficial volar wound measuring approximately 7 cm, concave in shape, extended from the base of the third finger to the thumb, forming a conjoined palmar flap. (b and c) lateral and dorsal side of the left hand showed dorsal concavity deformity of the left hand and posterolateral deformity of the thumb at the interphalangeal joint, with a 2-cm open wound at the base of the distal phalanx
Standard radiographs (anteroposterior and lateral views) of the left hand demonstrated a volar convergent, spatulate CMC dislocation with an associated posterolateral dislocation of the thumb at the interphalangeal joint (Fig. 2).
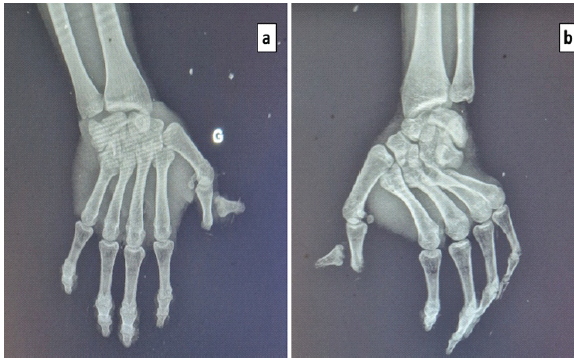
Figure 2: Pre-operative radiographs. Anteroposterior and lateral views showing a volar convergent spatulate carpometacarpal dislocation with an associated posterolateral dislocation of the thumb at the interphalangeal joint.
The patient was taken to the operating room under general anesthesia. Surgical debridement of the wounds was performed, followed by closed reduction using external maneuvers. Traction was applied along the axis of the fingers, combined with direct manual pressure on the bases of the metacarpals, while additional traction on the thumb achieved reduction of all dislocations. The reductions were stable. The wounds were then sutured, and immobilization was applied using an anterior splint encompassing the thumb column (Fig. 3).
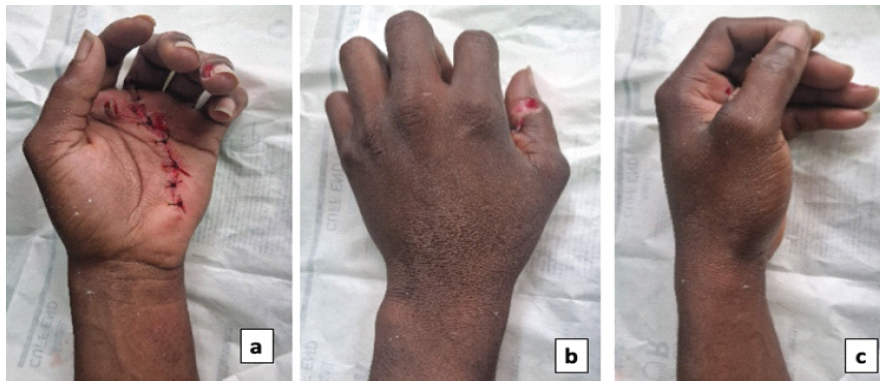
Figure 3: Clinical presentation after reduction. Closed reduction achieved using axial traction on the fingers and direct manual pressure on the metacarpal bases, followed by traction on the thumb. (a) palmar view of the left hand (b) dorsal view of the left hand (c) lateral view of the left hand.
Immediate post-operative radiographs were satisfactory (Fig. 4). Complete wound healing was achieved by day 12, and the anterior plaster cast was removed 45 days post-injury.
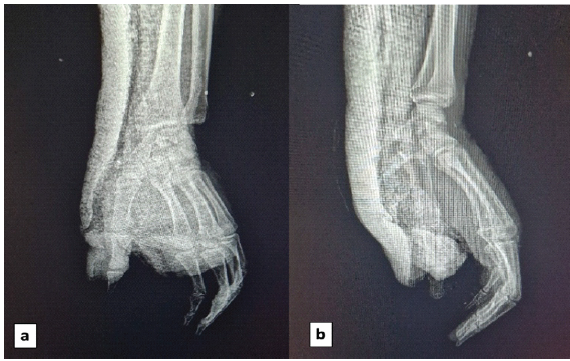
Figure 4: immediate post-operative radiographs. (a) Anteroposterior and lateral (b) views confirming stable reduction of the carpometacarpal and interphalangeal dislocations after closed reduction and immobilization with an anterior splint including the thumb column.
Progressive active mobilization of the fingers commenced during the 3rd post-operative week. At 3 months of follow-up, the functional outcome was satisfactory, with good muscle strength comparing to the opposite hand and full recovery of wrist and finger motion (Fig. 5). The patient returned to work 8 weeks after the injury.
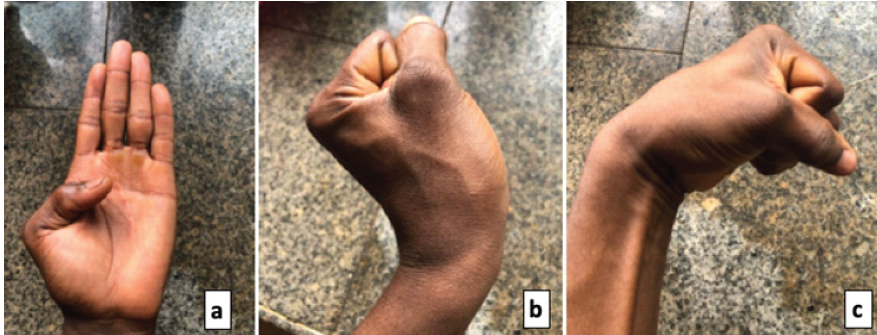
Figure 5: Functional outcomes at 3 months. Full recovery of wrist and finger motion, with preserved muscle strength, allowing the patient to resume work 8 weeks after the injury. (a) Full extension of long fingers and flexion of thumb (b) extension of wrist and full flexion of fingers (c) flexion of wrist and fingers.
The CMC joints are highly stable due to their bony architecture and a strong capsuloligamentous system reinforced by tendon insertions, which limits their mobility [4]. Dislocation of these joints typically requires high-energy trauma, as in our patient who sustained a motorcycle accident. Direct impact on the bases of the metacarpals was responsible for both the dislocations and the associated skin lesions. Clinical diagnosis was straightforward due to the short interval between injury and admission, and the patient being hemodynamically stable. Examination revealed dorsal concavity of the left hand and a posterolateral deformity of the thumb at the interphalangeal joint. Diagnosis can be more challenging when edema develops rapidly, masking deformities, or in the context of polytrauma [5]. Standard anteroposterior radiographs can reveal disappearance of the CMC joint spaces, reduction in the height of the medial carpus, and disruption of Gilula’s arc III. Lateral or oblique views show an increased palmodorsal diameter of the carpus [6]. Given the mechanism of injury and observed deformities, careful assessment of the radiographs is essential to detect frequently associated injuries in the second carpal row. Such combined injury patterns involving simultaneous dislocations of multiple thumb joints have been reported rarely in case reports in the literature [6], our patient presented a complete posterolateral spatulate CMC dislocation with an associated posterolateral interphalangeal dislocation of the thumb. In some cases, computed tomography is necessary for detailed evaluation. Most authors recommend reduction followed by stabilization through the dorsal approach. Stabilization can be achieved with intramedullary, oblique, or cross-pin fixation, securing the dislocated metacarpal(s) to the carpal bones and/or adjacent healthy metacarpals [7]. Immobilization in an intrinsic splint or cast for 5–6 weeks is generally advised [8]. Associated injuries can lead to residual pain, reduced grip strength, and limited finger mobility [9]. In our case, closed reduction and immobilization with an anterior splint, including the thumb column, were sufficient. Recent dislocations (<10 days old) that are stable after reduction can often be managed conservatively [10]. At 3 months follow-up, the patient demonstrated good muscle strength and full recovery of wrist and finger motion, allowing a return to work at 8 weeks.
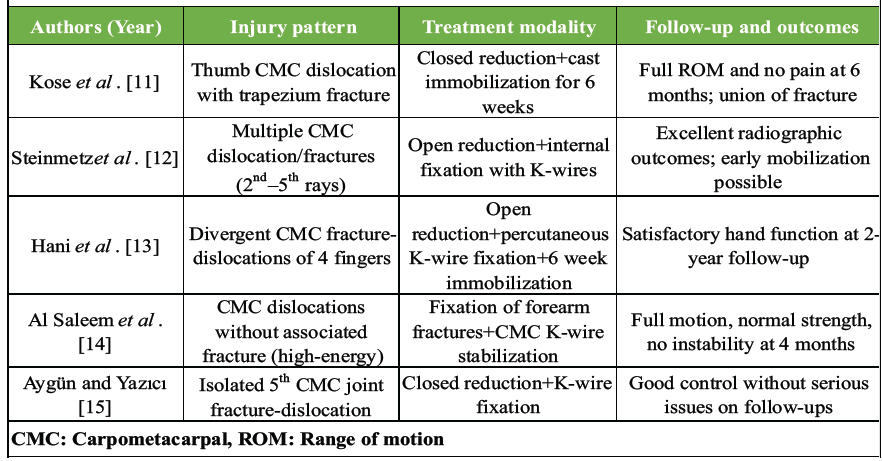
Table 1: Review of literature on carpometacarpal dislocations: Treatment modalities and outcomes
As shown in Table 1, recent literature supports management of CMC dislocations, with treatment choice primarily guided by post-reduction stability and associated injuries.
This case highlights the importance of early diagnosis, careful reduction, and structured rehabilitation in complex volar CMC dislocations with concomitant thumb interphalangeal injuries. Thorough clinical evaluation and appropriate imaging are essential to guide treatment. Early and coordinated multidisciplinary management is key to restoring hand function and preventing long-term disability.
Early recognition, careful reduction, and structured rehabilitation are essential in complex carpometacarpal and thumb interphalangeal injuries to restore hand function and prevent long-term disability.
References
- 1. Ebelin M, Soubeyrand M, Idrissi R. Carpo-metacarpal dislocations. In: Musculoskeletal System. Paris: EMC Elsevier Masson SAS; 2010. [Google Scholar] [PubMed]
- 2. Guimaraes RM, Benaissa S, Moughabghab M, Dunaud JL. Carpometacarpal dislocations of the long fingers. Apropos of 26 cases with review of 20 cases. Rev Chir Orthop Reparatrice Appar Mot 1996;82:598-607. [Google Scholar] [PubMed]
- 3. O’Rourke PJ, Quinlan W. Fracture dislocation of the fifth metacarpal resulting in compression of the deep branch of the ulnar nerve. J Hand Surg Br 1993;18:190-1. [Google Scholar] [PubMed]
- 4. Kirkham SG, Gray RJ. Multiple carpometacarpal dislocations and an ipsilateral scapho-trapezium-trapezoid fracture-dislocation: A rare pattern of injury. J Orthop Surg (Hong Kong) 2004;12:267-9. [Google Scholar] [PubMed]
- 5. Dabire MN, Zeba AA, Kafando H, Hien J, Segda S, Tall M. Luxation spatulaire complete dorsale carpo metacarpienne: A propos d’un cas. Moroccan J Orthop Traumatol Surg 2020;84:11-3. [Google Scholar] [PubMed]
- 6. Li X, Leung F, Fang C, Wong TM. Floating thumb with simultaneous carpometacarpal and metacarpo-phalangeal dislocation: a case report. J Surg. 2019;7(1):24–27. doi:10.11648/j.js.20190701.15. [Google Scholar] [PubMed] [CrossRef]
- 7. Ameziane L. Total carpometacarpal dislocations. Two case reports. Chir Main 2002;21:309-12. [Google Scholar] [PubMed]
- 8. Diez E, Marti D, Aramburo F, Mendez JM. Multiple carpometacarpal dislocations. Five cases. Ann Chir Main Memb Super 1997;16:300-4. [Google Scholar] [PubMed]
- 9. Waugh RL, Yancey AG. Carpometacarpal dislocations with particular reference to simultaneous dislocation of the bases of the fourth and fifth metacarpals. J Bone Joint Surg Am 1948;30A:397-404. [Google Scholar] [PubMed]
- 10. Gerard F, Garbulo P, Tropet Y, Vichard P. Traumatic dorsal carpometacarpal dislocations of long fingers. About 30 cases. Hand 1998;3:23-32. [Google Scholar] [PubMed]
- 11. Kose O, Keskinbora M, Guler F. Carpometacarpal dislocation of the thumb associated with fracture of the trapezium. J Orthop Traumatol 2015;16:161 5. [Google Scholar] [PubMed]
- 12. Steinmetz G, Corning E, Hulse T, Fitzgerald C, Holy F, Boydstun S, et al. Carpometacarpal fracture-dislocations: A retrospective review of injury characteristics and radiographic outcomes. Hand (N Y) 2021;16:362 7. [Google Scholar] [PubMed]
- 13. Hani R, Jeddi I, Berrada MS. Divergent dislocation of the carpometacarpal joints: A case report. J Med Case Rep 2018;12:157. [Google Scholar] [PubMed]
- 14. Al Saleem MS, ALthabit F, AlOnayzan AH, Alruwaili K, Almutairi A. Isolated carpometacarpal dislocation without associated fracture: A case report of high-energy wrist trauma. Cureus 2025;17:e92461. [Google Scholar] [PubMed]
- 15. Aygün Ü, Yazıcı A. Isolated dorsal dislocation of the 5th carpometacarpal joint; a missed injury. J Emerg Med Case Rep/Acil Tıp Uzmanları Derneği 2022;13:74 5. [Google Scholar] [PubMed]