Lateralizing the femoral intramedullary entry point is a simple, reproducible option to correct alignment when performing total knee arthroplasty in patients with severe femoral bowing.
Dr. Pedro Rasteiro, Department of Orthopaedic Surgery, Hospital Curry Cabral – Unidade Local de Saúde São José, Lisbon, Portugal. E-mail: pedrorasteiro28@gmail.com
Introduction: Severe knee osteoarthritis associated with anterolateral femoral bowing presents unique challenges for achieving accurate alignment during total knee arthroplasty (TKA). Extra-articular deformity may prevent proper positioning of the femoral cutting block, increasing the risk of malalignment. This case is important because it illustrates a simple and accessible technique to manage substantial femoral bowing without relying on navigation or robotic technology.
Case Report: We report the case of an 84-year-old woman with end-stage left knee osteoarthritis and marked anterolateral femoral bowing, treated with cemented posterior-stabilized TKA. A key technical adaptation was the use of a deliberately lateralized femoral intramedullary (IM) entry point, allowing alignment of the IM guide with the patient’s mechanical axis despite the deformity. The patient recovered uneventfully and demonstrated progressive improvement. At 6 months, she walked independently without walking aids and had full functional recovery.
Conclusion: In cases of significant femoral bowing, intentional lateralization of the femoral entry point is crucial for achieving accurate mechanical alignment using conventional instrumentation. This technique is practical, reproducible, and particularly useful when advanced computer-assisted systems are unavailable.
Keywords: Osteoarthritis, knee, total knee arthroplasty, femoral bowing, intramedullary guide, entry point.
Accurate alignment of the femoral component is a cornerstone of the long-term success of total knee arthroplasty (TKA). In patients with significant femoral bowing, the use of a conventional intramedullary (IM) guide may lead to coronal malalignment and subsequent complications, such as instability, polyethylene wear, and early loosening [1,2]. Navigation and robotic systems have been shown to improve accuracy [3,4]; however, these technologies are not universally available. We present a case of severe anterolateral femoral bowing managed with cemented posterior-stabilized (PS) TKA using conventional instrumentation. The key technical modification was the intentional lateralization of the femoral entry point to restore the mechanical alignment and minimize the risk of malposition.
Patient description
The patient was an 84-year-old woman with a body mass index of 34, who was admitted for surgical management of advanced left knee osteoarthritis. Her medical history included right hemicolectomy for cecal adenocarcinoma (2020), cholecystectomy (7 years prior), left saphenectomy (30 years prior), right wrist fracture with surgical fixation (20 years prior), vertiginous syndrome, cervicalgia, and chronic cough. She was on atorvastatin/ezetimibe, bromazepam, and betahistine, and had no known drug allergies.
Clinical findings
On physical examination, she ambulated with an antalgic gait. The left knee showed mild varus deformity, moderate quadriceps atrophy, and a range of motion from 10° shy of terminal extension to 125° of flexion. No effusion was observed, and the ligaments were stable. The varus deformity was partially reducible.
Diagnostic assessment
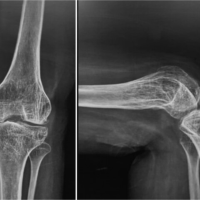
Radiographic evaluation (anteroposterior, lateral, and long-leg standing radiographs) revealed Kellgren–Lawrence Grade IV osteoarthritis with marked anterolateral femoral bowing (Fig. 1a, b, c).
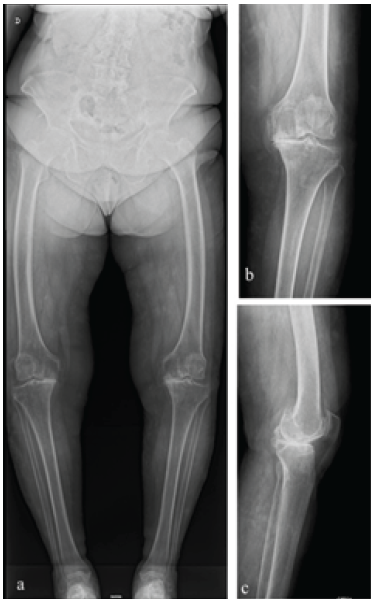
Figure 1: (a) Pre-operative standing long-leg anteroposterior (AP) radiograph showing advanced left knee osteoarthritis with varus deformity and severe anterolateral femoral bowing. (b) Pre-operative standing AP radiograph. (c) Pre-operative standing lateral radiograph.
Femoral lateral bowing was defined as a coronal plane angle of ≥5°, according to Kim and Lee [5]. The lateral femoral bowing angle was measured using the Yau method, as described by Lee et al. [6], which has been shown to be highly reproducible (inter-rater reliability ≈ 0.98). Pre-operative measurements included a mechanical axis deviation of 16.2° of varus (Fig. 2), a lateral femoral bowing angle of 20.4 degrees (Fig. 3), lateral distal femoral angle of 95.2°, and medial proximal tibial angle of 89.2°.
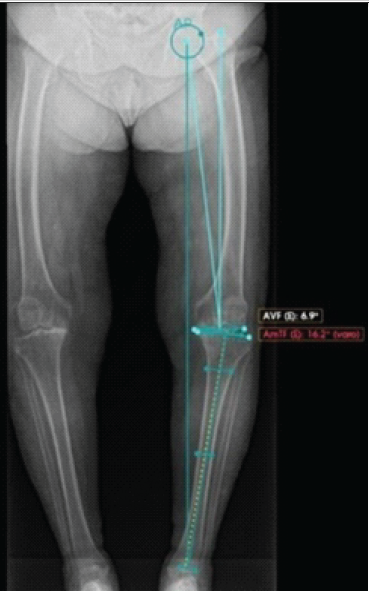
Figure 2: Pre-operative standing long-leg anteroposterior radiograph measurement of 16.2° of varus.
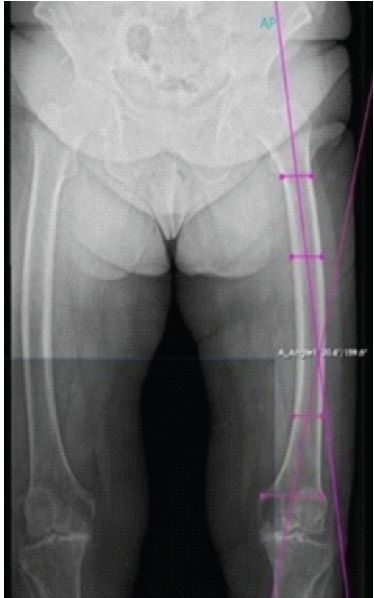
Figure 3: Pre-operative radiographic measurement of femoral bowing angle of 20.4°.
Although no universally accepted classification system exists, according to Park et al. [7], this deformity corresponds to Grade III bowing, in which the reference line passes medial to the femoral cortex. Pre-operative digital templating and measurements were performed using PeekMed® software. This allowed precise quantification of deformity parameters, simulation of mechanical axis correction, and optimization of surgical strategies.
Therapeutic intervention
Under neuroaxial anesthesia and tourniquet, the patient underwent a cemented PS TKA (Triathlon® Stryker; femur size 6 PS, tibia size 5, 9 mm polyethylene insert) via a medial subvastus approach. To accommodate the deformity, the femoral IM entry point was lateralized 12 mm from the intercondylar notch center (Fig. 4a, b, c).
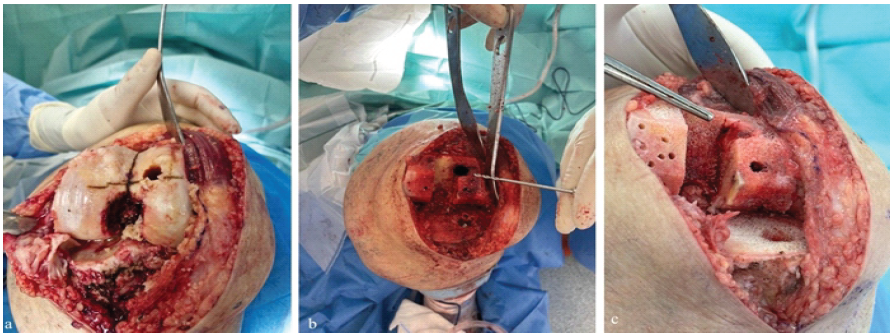
Figure 4: (a, b, c) Intraoperative photographs illustrating the lateralized femoral intramedullary entry point, approximately 12 mm lateral to the intercondylar notch.
This adjustment allowed the IM rod to align with the mechanical axis despite bowing. To decrease hidden blood loss, a bone plug was used to close the IM canal. Surgery and hospitalization were uneventful, and the patient was discharged on day 3.
Follow-up and outcomes
Tromboembolic prophylaxis was performed using subcutaneous enoxaparin for 28 days. On the 1st post-operative day, the patient began rehabilitation and full weight-bearing according to tolerance with two crutches. At 15 days postoperatively, the patient walked with two crutches, with extension to 0° and flexion to 100°. At 3 months, she ambulated with a single crutch, achieving full extension, 130° of flexion, and the surgical wound healed uneventfully. At 6 months of follow-up, she walked independently without crutches, maintaining a full range of motion and performing activities of daily living without limitations. Control radiographs confirmed satisfactory prosthetic alignment and restoration of the mechanical axis with 1.8° of valgus (Fig. 5a, b, c), a lateral distal femoral angle of 89.4°, and a medial proximal tibial angle of 90.7°.
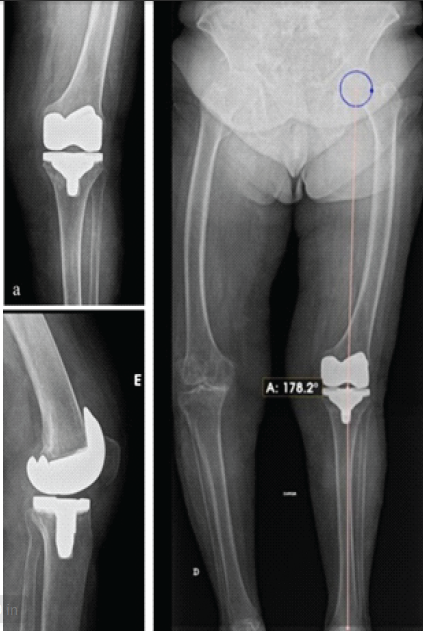
Figure 5: (a) Six-month post-operative anteroposterior (AP) radiograph showing prosthesis in satisfactory coronal alignment. (b) Six-month post-operative lateral radiograph showing prosthesis in satisfactory sagittal position. (c) Six-month post-operative long-leg AP radiograph demonstrating restoration of mechanical axis to 1.8° of valgus.
The restoration of coronal alignment is one of the strongest predictors of implant survival after TKA. Multiple long-term studies have shown that deviations >3° in the coronal plane are associated with higher rates of loosening, polyethylene wear, and revision surgery [1,2]. In particular, residual varus alignment has been associated with limited soft tissue remodeling, worse clinical outcomes, and a higher risk of implant failure in several series [1,8,9]. Jia et al. demonstrated that patients with residual varus after PS TKA exhibited impaired medial soft tissue remodeling [8], whereas Meneghini et al. reported worse clinical outcomes and satisfaction in patients left in residual varus alignment [9]. Patients with femoral bowing face unique challenges. Although no universally accepted classification system exists, Park et al. [7] proposed a grading method based on the relationship between the reference line and femoral cortex. According to this system, our case corresponded to a Grade III deformity. Such severe cases are particularly prone to IM guide malalignment and subsequent component malposition. The successful correction in our patient, despite the severity, underscores the value of intentional entry point lateralization as a pragmatic and reproducible solution in resource-limited settings. The IM rod, when introduced through a conventional central notch entry point, may not follow the mechanical axis because of diaphyseal curvature. This discrepancy can result in an inaccurate distal femoral resection, leading to malalignment. Zeng et al. demonstrated a direct correlation between the degree of femoral bowing and the optimal IM entry point [10]. Similarly, Thippanna and Kumar showed that intentional lateralization of the femoral entry point improved coronal alignment in bowed femora compared with the standard central entry [11]. Alternative strategies include extramedullary guides [12], patient-specific instrumentation (PSI) [13], computer navigation, and robotic assistance [3,4]. Navigation and robotic systems consistently improve accuracy, particularly in patients with severe deformities [3,4]. However, their widespread adoption is limited by their cost, availability, and learning curve. PSI has produced mixed results, with some studies showing improved alignment and others reporting no significant advantage [13]. Extramedullary systems bypass femoral bowing but are less commonly used and are technically demanding [12]. In this context, lateralization of the femoral entry point during conventional IM-guided TKA represents a simple, low-cost, reproducible alternative. Our case demonstrates that substantial lateralization (12 mm) of the femoral entry point is required to align the IM rod with the mechanical axis, successfully correcting the severe deformity and minimizing the risk of varus malposition. Clinically, the benefits of proper alignment extend beyond implant survival to include improved kinematics, reduced instability, and more durable polyethylene wear [1,2]. Nevertheless, surgeons should remain cautious of this approach. Excessive lateralization may affect sagittal alignment, resulting in a flexion–extension mismatch or patellofemoral maltracking [1]. While case reports and small series support this modification, high-quality prospective studies are required to standardize the technique, define the optimal lateralization distance, and validate long-term outcomes. In summary, the intentional lateralization of the femoral entry point can be an effective strategy to optimize alignment in bowed femora, bridging the gap between conventional guides and advanced technologies. Our case adds practical evidence to support its applicability in daily practice.
In elderly patients with severe deformity and femoral bowing, cemented TKA can be successfully performed using a lateralized femoral IM entry point. This practical technical modification improves alignment and reduces the risk of complications associated with malposition, offering a cost-effective alternative when navigation or robotic assistance is unavailable.
In patients with bowed femora, adjusting the femoral entry point can prevent malalignment and improve clinical outcomes during conventional total knee arthroplasty.
References
- 1. Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am 2011;93:1588-96. [Google Scholar] [PubMed]
- 2. Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: Just how important is it? J Arthroplasty 2009;24:39-43. [Google Scholar] [PubMed]
- 3. Nam JH, Jung SH, Bae JW, Bae DJ, Choi WK. Navigation makes more accurate femur resection compared to conventional total knee arthroplasty in lateral femoral bowing greater than 5º. Medicine (Baltimore) 2023;102:e36223. [Google Scholar] [PubMed]
- 4. Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res 2013;471:118-26. [Google Scholar] [PubMed]
- 5. Kim CW, Lee CR. Effects of femoral lateral bowing on coronal alignment and component position after total knee arthroplasty: A comparison of conventional and navigation-assisted surgery. Knee Surg Relat Res 2018;30:64-73. [Google Scholar] [PubMed]
- 6. Lee YK, Yeom J, Jang BW, Nho JH, Suh YS, Koo KH. Reliability of measuring lateral bowing angle of the femur in patients with atypical femur fractures. J Orthop Surg (Hong Kong) 2019;27:2309499019881475. [Google Scholar] [PubMed]
- 7. Park YC, Song HK, Zheng XL, Yang KH. Intramedullary nailing for atypical femoral fracture with excessive anterolateral bowing. J Bone Joint Surg Am 2017;99:726-35. [Google Scholar] [PubMed]
- 8. Jia Y, Zhai L, Qin S, Xu J, Gao W, Zhang B, et al. Residual varus alignment after posterior-stabilized total knee arthroplasty limits medial soft tissue remodeling. BMC Musculoskelet Disord 2023;24:918. [Google Scholar] [PubMed]
- 9. Meneghini RM, Grant TW, Ishmael MK, Ziemba-Davis M. Leaving residual varus alignment after total knee arthroplasty: Does it affect outcomes? J Arthroplasty 2017;32:3641-6. [Google Scholar] [PubMed]
- 10. Zeng X, Yang Y, Jia Z, Chen J, Shen H, Jin Y, et al. The position of entry point in total knee arthroplasty is associate with femoral bowing both in coronal and sagittal planes. Front Surg 2022;9:935840. [Google Scholar] [PubMed]
- 11. Thippanna RK, Kumar MN. Lateralization of femoral entry point to improve the coronal alignment during total knee arthroplasty in patients with bowed femur. J Arthroplasty 2016;31:1943-8. [Google Scholar] [PubMed]
- 12. Wang Q, Zhang X, Shi T, Bao Z, Wang B, Yao Y, et al. The accuracy of an extramedullary femoral cutting system in total knee arthroplasty: Addressing femoral bowing. J Orthop Surg Res 2022;17:221. [Google Scholar] [PubMed]
- 13. AlShammari SA, Choi KY, Koh IJ, Kim MS, In Y. Does patient-specific instrumentation improve accuracy of femoral component alignment in bowed femora? BMC Musculoskelet Disord 2021;22:819. [Google Scholar] [PubMed]