Lateral extra-articular tenodesis, when combined with ACL reconstruction, improves rotational stability and functional outcomes without increasing complications, especially in high-risk athletic patients.
Dr. Yashodhan Bhatt, Bios Health, Mumbai, Maharashtra, India. E-mail: dryashodhanbhatt@gmail.com
Introduction: Residual rotational instability may persist after isolated anterior cruciate ligament reconstruction (ACLR). Lateral extra-articular tenodesis (LET) has re-emerged as an adjunct procedure to improve rotational stability. We present a comparative case series evaluating functional outcomes of ACLR performed with and without LET.
Materials and Methods: Forty patients with ACL injury were treated surgically between 2022 and 2024. Twenty patients underwent isolated ACLR (Group B) and 20 underwent ACLR combined with LET (Group A). Functional outcomes were assessed using the Knee Society Score (KSS), clinical stability tests, return-to-sport status, and complication profiles over an 18-month follow-up period.
Results: Both groups demonstrated significant functional improvement. Group A achieved higher KSS at all follow-up intervals. A negative pivot-shift test was observed in 95% of Group A compared with 70% of Group B. Return to pre-injury sports was higher in Group A (75% vs. 50%). Complication rates and range of motion recovery were comparable.
Conclusion: The addition of LET to ACLR improves rotational stability and functional recovery without increasing complications. Combined reconstruction may be advantageous in patients at risk of persistent instability.
Keywords: Anterior cruciate ligament, lateral extra-articular tenodesis, pivot shift, knee instability, case series.
The anterior cruciate ligament (ACL) plays a critical role in maintaining knee stability by resisting anterior tibial translation and rotational forces during functional activities. ACL injuries are common in young and physically active individuals and are associated with instability, reduced functional capacity, and increased risk of secondary meniscal and cartilage damage [1,2]. Arthroscopic ACL reconstruction (ACLR) is the standard treatment for symptomatic ACL deficiency. Despite advances in surgical techniques and rehabilitation protocols, a proportion of patients continue to demonstrate residual rotational instability and persistent pivot-shift phenomenon following isolated reconstruction [3]. Such instability may compromise return to sports and increase the risk of graft failure. Recent anatomical and biomechanical studies have emphasized the contribution of the anterolateral complex of the knee in controlling internal tibial rotation [4,5]. Failure to address this structure may explain persistent rotational laxity after isolated ACLR. Consequently, lateral extra-articular tenodesis (LET) has gained renewed interest as an adjunct to ACLR. Evidence suggests that LET reduces graft strain, improves rotational control, and decreases failure rates, particularly in high-risk populations, such as young athletes and patients participating in pivoting sports [6,7,8]. This study aims to compare functional outcomes and knee stability between isolated ACLR and ACLR combined with LET. Research question: In patients with anterior cruciate ligament injury, does arthroscopic ACLR combined with LET, compared with isolated ACLR, result in better functional outcomes, improved knee stability, and higher return-to-sport rates over an 18-month follow-up period? Hypothesis: Patients undergoing arthroscopic ACLR combined with LET (ACLR + LET) will demonstrate significantly better functional outcomes, improved rotational knee stability, and higher return-to-sport rates compared with patients undergoing isolated ACLR over an 18-month follow-up period.
Study design and setting
This prospective comparative longitudinal study was conducted at the Department of Orthopaedics, Pravara Rural Hospital, Loni, over an 18-month period after IEC approval (No. PIMS/DR/RMC/IEC-UG-PG/2025/313). Purposive sampling was used (Fig. 1).
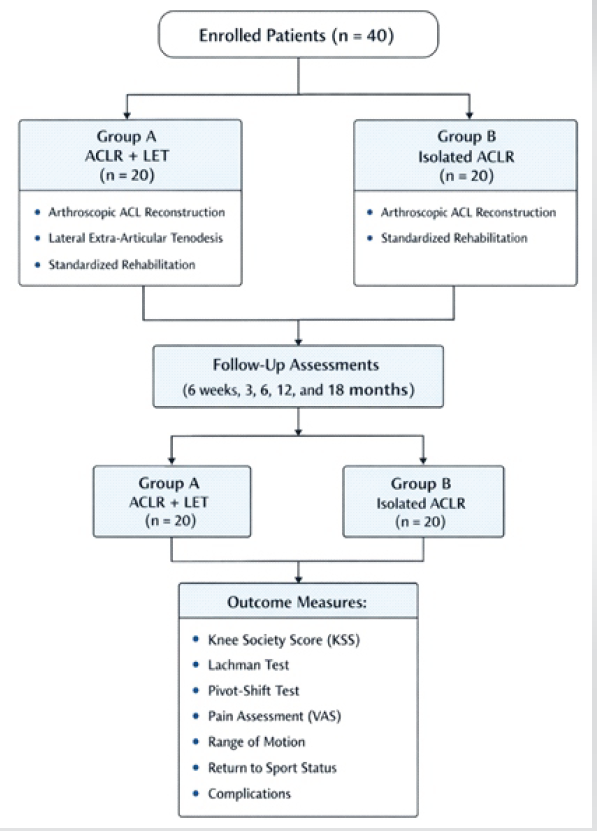
Figure 1: Study design.
Study population
Patients aged ≥18 years with clinically and MRI-confirmed ACL rupture were included. Inclusion criteria consisted of positive Lachman and anterior drawer tests and MRI evidence of ACL tear. Exclusion criteria included previous ACL surgery, associated realignment procedures, and two or more additional ipsilateral ligament injuries.
Sample size was calculated based on the primary outcome measure, the Knee Society Score (KSS). Based on previously published literature, a minimum clinically important difference of 8 points between the two groups was considered significant, with an estimated standard deviation of 10 points. To detect this difference with a power of 80% and a two-sided alpha error of 0.05, a minimum of 18 patients per group was required. To compensate for potential loss to follow-up and dropouts, the sample size was increased to 20 patients per group, giving a total sample size of 40 patients.
Pre-operative assessment
All patients underwent standardized clinical examination and radiological evaluation. Baseline functional status was assessed using the KSS. Demographic data, injury mechanism, and time from injury to surgery were recorded.
Surgical technique
All patients underwent arthroscopic ACLR using either hamstring tendon or peroneus longus tendon autograft. Standard anterolateral and anteromedial portals were established, the ACL remnants were debrided, and anatomic femoral and tibial tunnels were created under arthroscopic visualization. The prepared graft was passed through the tunnels and fixed using suspensory femoral fixation with appropriate tibial fixation after cycling and tensioning of the graft [2,9].
Group A patients additionally underwent LET using a modified Lemaire technique. A longitudinal strip of the iliotibial band was harvested while maintaining its distal attachment at Gerdy’s tubercle. The graft was passed deep to the lateral collateral ligament and routed proximally, then fixed to the femur at the isometric point with the knee held in approximately 30° of flexion and neutral rotation, ensuring appropriate tension without overconstraint.
Group B patients underwent isolated arthroscopic ACLR following the same intra-articular technique without any additional extra-articular stabilization procedure.
Rehabilitation protocol
Both groups followed an identical standardized rehabilitation protocol emphasizing early mobilization, quadriceps strengthening, progressive weight bearing, and gradual return to sports.
Outcome measures
Patients were evaluated at 6 weeks, 3 months, 6 months, 12 months, and 18 months. Outcomes included KSS, Lachman, and pivot-shift tests, pain assessment using the visual analog scale, return-to-sport status, range of motion, and postoperative complications.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation and categorical variables as percentages. Intergroup comparisons were performed using independent t-tests or Mann–Whitney U tests and Chi-square or Fisher’s exact tests as appropriate. A P < 0.05 was considered statistically significant.
Forty patients were included, with comparable baseline demographic and injury characteristics between groups. Most patients were aged 26–35 years, with male predominance. Sports-related trauma was the most common mechanism of injury. Mean operative time was longer in Group A (95 ± 12 min) than in Group B (75 ± 10 min). Post-operative complications were infrequent and comparable between groups. Functional outcomes improved significantly in both groups. Group A demonstrated significantly higher KSS at 6, 12, and 18 months (P < 0.05) (Fig. 2, Table 1). At final follow-up, pivot-shift testing was negative in 95% of Group A compared with 70% of Group B (P = 0.04). Lachman test outcomes favored Group A but were not statistically significant (Table 2).
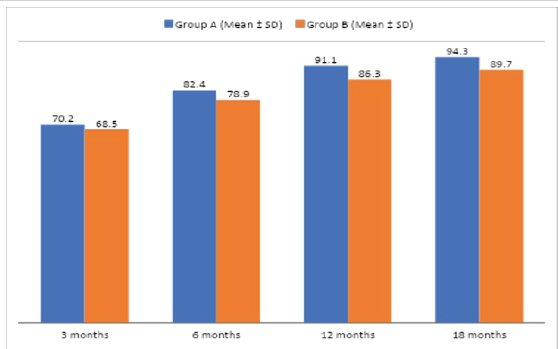
Figure 2: Mean knee society score over time.
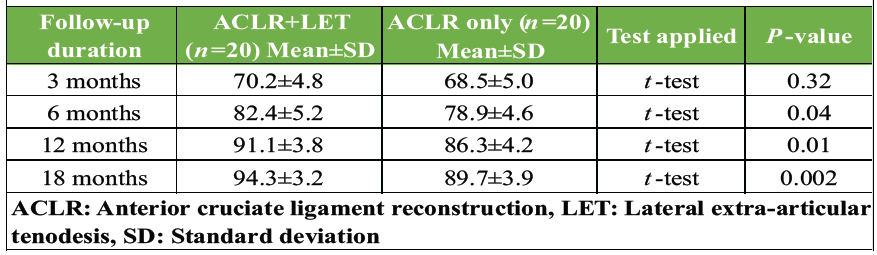
Table 1: Comparison of knee society score between groups
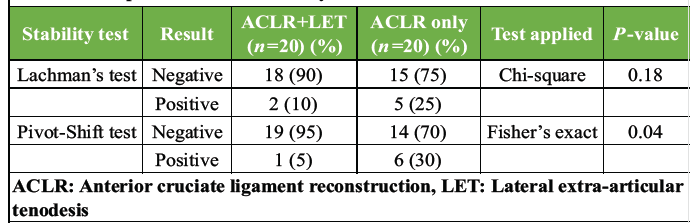
Table 2: Comparison of knee stability at 18 months
Return to pre-injury sports activity was achieved by 75% of Group A and 50% of Group B. Range of motion recovery, hospital stay, and early post-operative pain were comparable between groups.
The present study demonstrates that arthroscopic ACLR combined with LET provides superior rotational stability and improved functional outcomes compared with isolated ACLR. While both groups showed significant improvement in anterior stability, residual rotational laxity was significantly lower in patients who underwent the combined procedure, as evidenced by a higher proportion of negative pivot-shift tests and superior functional scores. These findings directly address the primary objective of the study, confirming that the addition of LET enhances clinical stability and functional recovery following ACLR. The improved control of pivot shift observed in the combined group supports the biomechanical role of LET in limiting excessive internal tibial rotation and reducing strain on the intra-articular graft, thereby improving overall knee kinematics and stability [7,8]. This improved rotational control is clinically relevant, as persistent pivot shift has been associated with subjective instability, delayed return to sport, and increased risk of graft failure. Higher return-to-sport rates in the ACLR + LET group further emphasize the functional benefits of addressing rotational instability, particularly in physically active individuals. Importantly, the addition of LET did not result in an increased incidence of complications, postoperative stiffness, or delayed rehabilitation, indicating that the combined procedure can be performed safely without compromising early recovery. The results of this study are consistent with several national and international reports demonstrating improved rotational stability and lower graft failure rates with combined procedures [6,7,8]. Notably, the findings align closely with the STABILITY trial, which reported significantly reduced graft rupture rates and improved rotational control when LET was added to ACLR in high-risk patients [10]. Minor variations in outcome magnitude compared with other studies may be attributed to differences in patient selection, activity level, graft choice, surgical technique, rehabilitation protocols, and duration of follow-up. Despite these encouraging findings, certain limitations must be acknowledged. The sample size was modest, which may limit the statistical power and generalizability of the results. In addition, the follow-up duration was relatively short and does not allow assessment of long-term graft survivorship, development of osteoarthritic changes, or late complications. The study was not blinded and relied partly on clinical examination scores, which may introduce observer bias. Future studies with larger multicenter cohorts, longer follow-up periods, and objective biomechanical assessments are recommended to further validate these findings and to identify patient subgroups that may benefit most from the addition of LET. Randomized controlled trials comparing different LET techniques and fixation methods would also help optimize surgical strategies.
ACLR combined with LET provides superior rotational stability, improved functional outcomes, and higher return-to-sport rates compared with isolated ACLR, without increasing complications. This combined approach may be particularly beneficial in high-risk or athletic populations.
Adding lateral extra-articular tenodesis to arthroscopic ACL reconstruction significantly improves rotational stability and functional outcomes without increasing complications in appropriately selected patients.
References
- 1. Yu X, Hu J, Li Y, Wen Y, Li B. ACL injury management: a comprehensive review of novel biotherapeutics. Front Bioeng Biotechnol. 2024 Nov 22;12:1455225. doi: 10.3389/fbioe.2024.1455225. PMID: 39650235; PMCID: PMC11620901. [Google Scholar] [PubMed] [CrossRef]
- 2. Jin T, Huang Y, Zhang Q. Analysis of risk factors for knee cartilage damage in patients with anterior cruciate ligament rupture. Medicine (Baltimore). 2025 Dec 19;104(51):e46103. doi: 10.1097/MD.0000000000046103. PMID: 41431029; PMCID: PMC12727413. [Google Scholar] [PubMed] [CrossRef]
- 3. Musahl V, Rahnemai-Azar AA, Costello J, Arner JW, Fu FH. The pivot shift: A global user guide. Knee Surg Sports Traumatol Arthrosc 2017;25:1077-89. [Google Scholar] [PubMed]
- 4. Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat 2013;223:321-8. [Google Scholar] [PubMed]
- 5. Inderhaug E, Stephen JM, Williams A, Amis AA. Biomechanical comparison of anterolateral procedures combined with ACL reconstruction. Am J Sports Med. 2017;45:347-54. [Google Scholar] [PubMed]
- 6. Getgood AM, Bryant D, Litchfield RB, McCormack RG, Heard M, MacDonald PB, et al. Lateral Extra-Articular Tenodesis Reduces Failure of Hamstring Tendon Autograft ACL Reconstruction -Two Year Outcomes from the STABILITY Study Randomized Clinical Trial. Orthop J Sports Med. 2019 Jul 29;7(7 suppl5):2325967119S00280. doi: 10.1177/2325967119S00280. PMCID: PMC6668002. [Google Scholar] [PubMed] [CrossRef]
- 7. Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, et al. Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: A prospective comparative study of 502 patients from the santi study group. Am J Sports Med 2017;45:1547-57. [Google Scholar] [PubMed]
- 8. Zaffagnini S, Grassi A, Lucidi GA, Dal Fabbro G, Ambrosini L. Combined Anterior Cruciate Ligament Reconstruction and Lateral Extra-Articular Tenodesis: The “Over-the-Top” Technique. Video J Sports Med. 2023 Sep 11;3(5):26350254231177378. doi: 10.1177/26350254231177378. PMID: 40308443; PMCID: PMC11962631. [Google Scholar] [PubMed] [CrossRef]
- 9. Noyes FR, Barber-Westin SD. Revision anterior cruciate ligament surgery: Experience from Cincinnati. Clin Orthop Relat Res 1996;325:116-29. [Google Scholar] [PubMed]
- 10. Getgood AMJ, Bryant DM, Litchfield R, Heard M, McCormack RG, Rezansoff A, et al. Lateral Extra-articular Tenodesis Reduces Failure of Hamstring Tendon Autograft Anterior Cruciate Ligament Reconstruction: 2-Year Outcomes From the STABILITY Study Randomized Clinical Trial. Am J Sports Med. 2020 Feb;48(2):285-297. doi: 10.1177/0363546519896333. Epub 2020 Jan 15. PMID: 31940222. [Google Scholar] [PubMed] [CrossRef]