Arthroscopic findings of Gouty arthritis and Chondrocalcinosis may mimic each other, histopathology and synovial fluid analysis are essential to confirm the diagnosis and to start appropriate treatment.
Dr. Vineet Thomas Abraham, Department of Orthopaedics, All India Institute of Medical Sciences, Guntur, Andhra Pradesh, India. E-mail: abrahamvineet@hotmail.com
Introduction: Isolated tophaceous gout of the knee is a rare presentation, requiring a high degree of suspicion to differentiate it from chondrocalcinosis. If left untreated, chronic tophaceous gout can cause internal derangements and cartilage damage to the knee.
Case Report: A 32-year-old male presented with a painful, swollen knee joint with stiffness. Magnetic resonance imaging (MRI) showed Arthrofibrosis with features of synovitis. Arthroscopic evaluation showed synovitis with chalky deposits over the chondral surfaces, menisci, anterior cruciate ligament and over synovium, which was typical of chondrocalcinosis, but histopathological analysis revealed uric acid crystals. Arthroscopic debridement of tophi with arthrolysis and partial synovectomy was done. The patient had a reduction in pain, and his range of movements improved.
Conclusion: Isolated tophaceous gout of the knee is rare; a strong index of suspicion is necessary to come to a diagnosis. MRI and arthroscopy findings can be deceiving; hence, histopathology and synovial fluid analysis are necessary to confirm the diagnosis. The arthroscopic management can yield good clinical outcomes.
Keywords: Knee, gout, chondrocalcinosis, arthroscopy, synovitis.
Gout is a form of inflammatory arthritis caused by the deposition of monosodium urate crystals in the joints and is associated with high levels of uric acid in the blood. It affects men older than 40 years of age, and men are twice as likely to be affected compared to women [1]. Tophaceous gout is a long-term condition marked by the buildup of monosodium urate crystals in the joints and surrounding tissues, which results in the development of tophi [1]. Chondrocalcinosis refers to the deposition of various types of crystals in cartilage, with the most common crystals representing calcium pyrophosphate dihydrate (CPPD) caused by an imbalance between the production of pyrophosphate and the levels of pyrophosphatases in diseased cartilage [2]. Whereas tophaceous deposits may be found in the subcutaneous tissues and the various joints, particularly the first metatarsophalangeal joint, the hand, wrist, or elbow, while chondrocalcinosis affects larger joints, such as knee, shoulder, wrist, and ankle [3]. Both tophaceous gout and chondrocalcinosis presents with features of synovitis, such as severe pain, swelling, erythema, warmth along with restricted mobility. Like gout, CPPD can be associated with fever, leucocytosis, raised C-reactive protein and erythrocyte sedimentation rate [4]. However, isolated tophaceous gout of the knee is relatively rare, with few cases reported in the literature [5]. Magnetic resonance imaging (MRI) findings are not specific because tophi have a wide spectrum of signal intensity characteristics, mimicking conditions, such as chondrocalcinosis, pigmented villonodular synovitis, inflammatory arthritis, amyloidosis, and soft tissue tumor [6]. The management of acute gouty arthritis is primarily medical, whereas in cases of chronic gout, when significant tophus formation occurs, surgical intervention, such as arthroscopic debridement may be necessary to effectively alleviate mechanical symptoms and decreases the risk of acute gout flares by removing tophi deposits [7]. In this case report, we present the management of a 32-year-old male presenting with features of synovitis with a diagnostic suspicion of tophaceous gout and chondrocalcinosis.
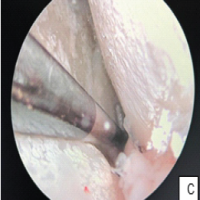
A 32-year-old male presented with pain in the left knee with stiffness for 1 year following a history of twisting injury to the knee while walking. He gave a history of locking episodes and difficulty in squatting and sitting cross-legged. He was a known case of chronic gout for 3 years on irregular medication. His father was a known case of Gout and was on treatment for 25 years. On examination, the patient had ichthyosis over both legs since childhood and mild effusion over the knee, with lateral joint line tenderness and a flexion deformity of 20°. The knee was stable without laxity, with a range of motion (ROM) from 20° to 70°, which was painful. (Fig. 1).
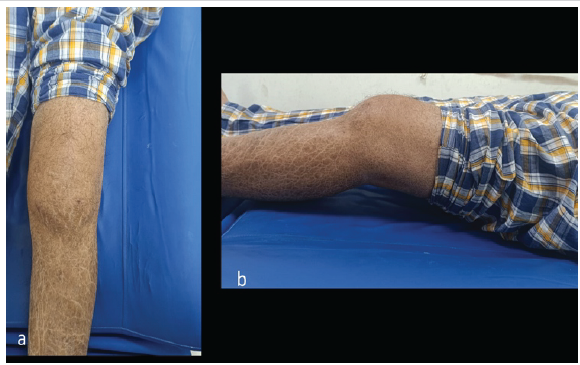
Figure 1: (a and b) Pre-operative clinical picture of left knee with ichthyosis showing fixed flexion deformity of around 20°.
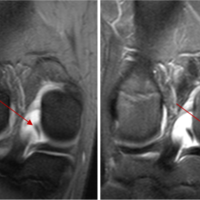
He had no other palpable gouty lesion in the body. He had an elevated serum uric acid of 13.4, with other normal blood parameters. The patient had a pre-operative Lysholm knee score of 35/100. MRI revealed Arthrofibrosis with lateral meniscal tear with mucoid degeneration of anterior cruciate ligament (ACL) with synovitis. The report did not mention any evidence of chondrocalcinosis. Due to the patient’s chronicity of mechanical symptoms and meniscal tear, the patient was taken up for diagnostic arthroscopy. The arthroscopic examination revealed synovitis with widespread chalky deposits over the chondral surfaces, menisci, fat pad, ACL and synovium in the suprapatellar pouch and intra-articularly. (Fig. 2).
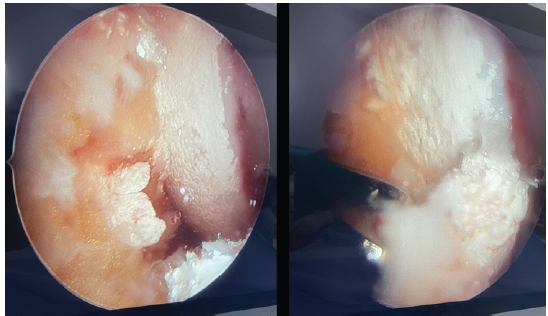
Figure 2: (a) Intraoperative arthroscopy images showing chalky white calcium deposits over articular surfaces. (b) Calcium deposits over articular cartilage and anterior cruciate ligament.
The synovial fluid was turbid and there was gross synovial hypertrophy. Samples of the synovium and synovial fluid were collected for histopathological analysis. Arthroscopic debridement of tophi with arthrolysis was done. Partial synovectomy and ACL debulking for mucoid degeneration were done. There was a 3 cm horizontal tear of the anterior horn of the lateral meniscus, which was repaired with outside-in sutures. Post-operatively, pain had decreased, and the patient was kept non-weight bearing for 4 weeks. Quadriceps strengthening exercises were started immediately, and ROM exercises started at 10 days post-operatively. Based on the arthroscopic findings, a provisional diagnosis of chondrocalcinosis was made. The histopathology reported, within the nodular aggregates, which is consistent with tophaceous gout. (Fig. 3). Synovial fluid analysis showed needle shaped crystals suggestive of gout. (Fig. 4). The patient was started on medical management with febuxostat. Post-operative serum uric acid was 7.5. At 6 months follow-up, the patient had a Lysholm score of 80/100. His range of movement had improved was 5° to 120°. The patient was able to carry out his daily activities and had no pain.
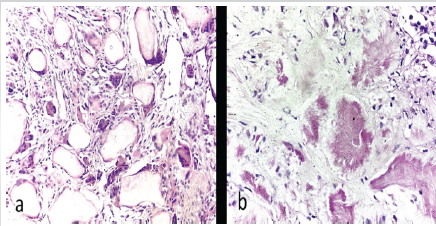
Figure 3: (a and b) Histopathology of synovium showing nodular aggregates surrounded by multinucleate giant cells.
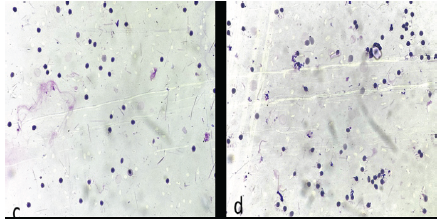
Figure 4: Synovial fluid cytology showing needle shaped crystals.
Knee pathology due to gout is difficult to diagnose as it mimics other intra-articular conditions, such as rheumatoid arthritis, loose body, ligamentous instability, meniscal pathology, or a tumor-like condition. The diagnosis of tophaceous gout was not straightforward, as there was no evidence of gouty tophi present anywhere in the body but only a history of recurrent gouty attacks [8]. MRI findings were not consistent with gout or chondrocalcinosis. Ko et al. showed that MRI findings of gouty tophi can be non-specific, but T1-weighted images can show low intermediate signal intensities and low intermediate heterogeneous signal intensities on the T2-weighted images [6]. Li et al. reported a unique case of intra-articular gouty tophi that was misdiagnosed for 8 years based on the clinical picture and MRI appearance and they concluded that gouty tophi is a great mimic, resembling several different intra-articular pathologies [9]. Isolated tophaceous gout of the knee is a rare occurrence, with only few cases reported in the literature which were managed by arthroscopy. Aoki et al. performed a partial meniscectomy and synovectomy for intra meniscal gouty tophi that resulted in resolution of pain and mechanical symptoms at follow-up [10]. Pan et al. reviewed 41 patients with gouty deposits who underwent arthroscopic debridement and irrigation, which resulted in significant improvement in pain and ROM [11]. Histopathological analysis and crystal visualization under light microscopy are necessary for confirmatory diagnosis of gout or chondrocalcinosis [12]. Chondrocalcinosis should be differentiated from gout, and appropriate treatment should be started for gout [13]. Post-operatively, the patient needs to begin medical management with anti-urate medications and monitoring serum uric acid levels, and immediate, aggressive physical therapy to regain the knee ROM. This case highlights the importance of histopathological examination to come to a diagnosis and the importance of the treatment of coexisting lesions for a better patient outcome.
Isolated tophaceous gout of the knee is rare. MRI and arthroscopy findings can be deceiving; hence, histopathology and synovial fluid analysis are necessary to confirm the diagnosis. The combination of surgical intervention, medical, and physical therapy is highly effective in managing advanced cases of tophaceous gout affecting the knee.
Synovitis and stiffness of the knee can have multiple etiologies. Proper clinical evaluation is essential. MRI may not reveal findings suggestive of Gout or Chondrocalcinosis. Arthroscopy can be both diagnostic and therapeutic in such cases. The follow-up treatment should be based on the histopathological diagnosis.
References
- 1. Choi HK, Mount DB, Reginato AM, American College of Physicians, American Physiological Society. Pathogenesis of gout. Ann Intern Med 2005;143:499-516. [Google Scholar] [PubMed]
- 2. Zamora EA, Naik R. Calcium Pyrophosphate Deposition Disease. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2025. Available from: http://www.ncbi.nlm.nih.gov/books/nbk540151 [Last accessed on 2025 Apr 28]. [Google Scholar] [PubMed]
- 3. Ozkan FU, Bilsel K, Turkmen I, Erdil M, Söylemez M, Ozkan K. Tophi gout around the knee joint: An unusual presentation with a soft tissue mass. Int J Case Rep Images 2013;4:593-6. [Google Scholar] [PubMed]
- 4. Schlee S, Bollheimer LC, Bertsch T, Sieber CC, Härle P. Crystal arthritides – gout and calcium pyrophosphate arthritis: Part 2: Clinical features, diagnosis and differential diagnostics. Z Gerontol Geriatr 2018;51:579-84. [Google Scholar] [PubMed]
- 5. Epidemiology of Gout. ResearchGate; 2024. Available from: https://www.researchgate.net/publication/23285338_epidemiology_of_gout [Last accessed on 2025 Apr 01]. [Google Scholar] [PubMed]
- 6. Ko KH, Hsu YC, Lee HS, Lee CH, Huang GS. Tophaceous gout of the knee: Revisiting MRI patterns in 30 patients. J Clin Rheumatol 2010;16:209-14. [Google Scholar] [PubMed]
- 7. Espejo-Baena A, Coretti SM, Fernandez JM, Garcia-Herrera JM, Del Pino JR. Knee locking due to a single gouty tophus. J Rheumatol 2006;33:193-5. [Google Scholar] [PubMed]
- 8. Su CH, Hung JK. Intraosseous gouty tophus in the talus: A case report. J Foot Ankle Surg 2016;55:288-90. [Google Scholar] [PubMed]
- 9. Li TJ, Lue KH, Lin ZI, Lu KH. Arthroscopic treatment for gouty tophi mimicking an intra-articular synovial tumor of the knee. Arthroscopy 2006;22:910.e1-3. [Google Scholar] [PubMed]
- 10. Aoki T, Tensho K, Shimodaira H, Akaoka Y, Takanashi S, Shimojo H, et al. Intrameniscal gouty tophi in the knee: A case report. JBJS Case Connect 2015;5:e74. [Google Scholar] [PubMed]
- 11. Pan F, Li Q, Tang X, Xue J, Li J. Method and effectiveness of arthroscopic debridement for treating gouty arthritis of the knee. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2011;25:937-40. [Google Scholar] [PubMed]
- 12. Kravchenko D, Bergner R, Behning C, Schäfer VS. How to differentiate gout, calcium pyrophosphate deposition disease, and osteoarthritis using just four clinical parameters. Diagnostics (Basel) 2021;11:924. [Google Scholar] [PubMed]
- 13. Sidari A, Hill E. Diagnosis and treatment of gout and pseudogout for everyday practice. Prim Care 2018;45:213-36. [Google Scholar] [PubMed]