A custom 3D-printed intercalary humeral prosthesis offers an effective solution for humeral shaft nonunion with extensive bone loss allowing immediate stability and early mobilization in a single-stage procedure.
Dr. Rahul Chandran, Department of Orthopedics, MOSC Medical Collage and Hospital, Ernakulam, Kerala, India. E-mail: rahulchandrannair55@gmail.com
Introduction: Non-union of the humeral shaft with segmental bone loss is a challenging clinical problem, especially in elderly patients, where conventional reconstruction with cortical fibular graft carries significant donor site morbidity. The advent of 3D printing technology offers novel solutions for patient-specific reconstruction.
Case Report: We report the case of a 70-year-old female with atrophic non-union of the right humeral shaft and 13.68 cm segmental bone loss, 6 years after locking compression plate fixation. Clinically, she had painless abnormal mobility at the fracture site and restricted shoulder motion, without signs of infection. Imaging revealed extensive osteolysis and bone loss. A patient-specific intercalary humerus prosthesis was designed using 3D printing technology. The prosthesis featured a porous lattice structure to facilitate osteointegration and was secured with a customized titanium plate and locking screws for optimal stability. Reconstruction achieved stable fixation with restoration of alignment. The patient had improved limb stability and function with early mobilization.
Conclusion: Custom 3D-printed intercalary humerus prosthesis can be a viable alternative to traditional bone grafting in selected cases of humeral shaft non-union with extensive segmental bone loss, offering stable fixation, early functional recovery, and reduced morbidity.
Keywords: Humerus nonunion, 3D printing, intercalary prosthesis, bone loss.
Nonunion of the humeral shaft can occur in 2–10% of nonsurgically treated fractures and in up to 15% of fractures treated by primary open reduction and internal fixation [1]. The risk of nonunion increases in the presence of open fractures, high-energy trauma, bone loss or fracture gap, soft-tissue interposition, unstable or segmental fracture patterns, compromised vascularity, infection, and initial management with traction or hanging casts. In addition, patient-related factors such as obesity, osteoporosis, chronic alcoholism, malnutrition, and poor compliance further contribute to nonunion [2]. When a humeral shaft nonunion occurs, the salient symptom is functional loss; nonunion typically is not as painful as in the lower extremity. However, the lack of mechanical stability precludes repetitive motion or lifting weights with the involved upper extremity [3]. Nonunion of humeral shaft fractures following failed osteosynthesis presents a significant treatment challenge, particularly in the setting of disuse osteoporosis, implant-related osteolysis, or when associated with substantial bone loss and fracture gap [4]. Various surgical strategies have been reported, including open reduction and internal fixation with dynamic compression plating, locking compression plating, interlocking nailing, and distraction osteogenesis (Ilizarov technique) [5]. Among these, autologous fibular grafting has been employed as an adjunct to plating to enhance biological and mechanical stability [6]. Advances in 3D printing have enabled the design of patient-specific implants, allowing precise restoration of bone continuity, maintenance of limb alignment, and facilitation of early functional recovery [7].
We report the case of a 70-year-old healthy, active female who was treated for a right humerus fracture with locking compression plate fixation 6 years back from an outside hospital presented to us with nonunion of the shaft of the humerus with bone loss and severe functional disability of the right upper limb. Clinically she had painless abnormal mobility at fracture site. Her shoulder joint movements were restricted, with abnormal mobility occurring at the fracture site each time she tried lifting her shoulder. There were no signs of local infection, skin breakage. She had no other comorbidities, and was not taking any medications. Radiological evaluation showed atrophic Non-union of the humeral shaft with significant bone loss. Computed tomography scans with 3D reconstruction showed osteolysis of the humerus shaft with 13.68 cm of bone loss(Fig.1). Routine blood investigations, erythrocyte sedimentation rate, and C-reactive protein were done to rule out infections.
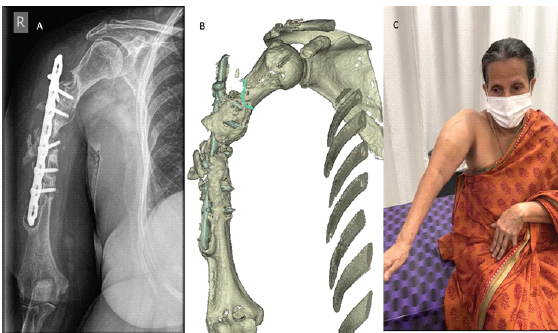
Figure 1: (a) Pre-operative radiograph showing humeral shaft nonunion with implant in situ. (b) 3D computed tomography reconstruction demonstrating the extent of bone loss and fracture gap. (c) Pre-operative clinical photograph demonstrating abnormal movement at the nonunion site of the humerus.
Various treatment options were discussed with the patient. We had the option of reconstructing bone loss with a bone graft that could require a separate incision on the leg to harvest the cortical fibular graft of large size, which may lead to graft site morbidity. Another option was to use mega prosthesis, but that would require resection of a larger length of humerus, which would include normal bone. We opted for creating a patient-specific humerus prosthesis utilizing innovative 3D printing technology. Intercalary prosthesis was used to secure the proximal and distal fragments of the humerus. The shaft was designed with a porous lattice structure to facilitate osteo-integration(Fig.2).

Figure 2: Design and structure of 3D-printed prosthesis.
The printed prosthesis was designed to retain and integrate the existing viable spikes of bone in the proximal and distal segments while recreating the lost mid-segment. This feature ensured that the implant would integrate with the patient’s existing bone structure, promoting long-term stability and functionality. To provide additional stability, a long, customized titanium plate was designed and printed. This plate played a crucial role in holding the distal fragment in place, allowing for proper bone healing and alignment. Six locking screws were employed on the humerus head to maximize bone purchase and ensure secure fixation. Locking screw fixation given on the distal humerus was performed from lateral to medial on the condyles. Post-operative radiographs obtained at the 3-month follow-up showed the 3D-printed humeral prosthesis and plate in situ with maintained alignment and no evidence of implant loosening or failure (Fig.3).
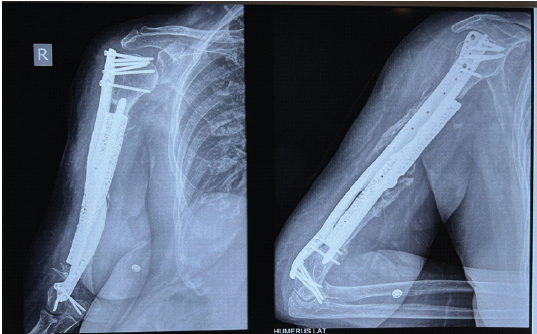
Figure 3: Post-operative radiograph showing prosthesis and plate.
After physiotherapy and strengthening exercises, she was able to use her right limb for her routine activities. Post-operative range of movements at the shoulder joint was found to be 120° of passive forward flexion and 100° of active forward flexion, internal and external rotations were comparable with the normal side(Fig.4).

Figure 4: (a, b, c) Post-operative range of movements.
It was found out that Constant Shoulder Score improved from of 38 preoperatively to post-operative 64, the American Shoulder and Elbow Surgeons score improved from 33.3 to 63.3 postoperatively, Disabilities of the Arm, Shoulder and Hand score had pre-operative average of 65.8 and post-operative average of 35.8 and Mayo Elbow Performance Score had pre-operative average of 50 and post-operative average of 80 measured at 12 months post-operative (Fig.5).
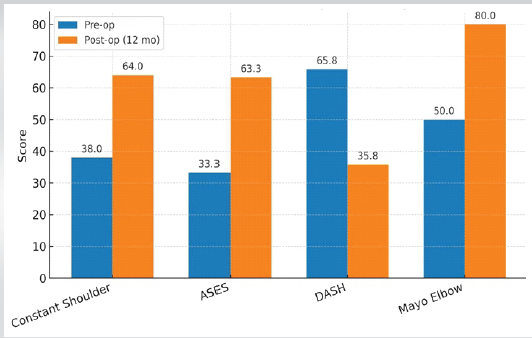
Figure 5: Pre-operative and post-operative functional outcome scores.
At 2 year follow-up, encouraging clinical outcomes were observed. The prosthesis remained stable in the original implantation area, and callus formation was found at the contact end of the prosthesis and the bone stump. The upper limb functions returned to normal with a satisfactory functional score.
The reported case highlights the use of custom 3D-printed intercalary humerus prosthesis for extensive segmental bone loss and non-union of the humeral shaft in an elderly patient, offering an alternative to conventional approaches to segmental bone loss in a long bone, such as cortical fibular grafting. For large defects exceeding 5 cm, bone grafts are prone to resorption, and the availability of grafting material remains limited [8]. In our case, the patient was 70 years old, where the risk of nonunion following grafting is further increased by the poor quality of the autologous bone graft secondary to osteoporosis. In addition, successful reconstruction strategies must account for both proper alignment and the anatomic characteristics of the native limb. The defect in this patient was located in the middle and distal thirds of the humerus. While the mid-humerus is cylindrical, the distal humerus is relatively broad and flat, creating a morphological mismatch that poses additional challenges in achieving anatomic union at both ends of the defect. Previous studies have validated the efficacy of intercalary prostheses in reconstructing humeral shaft defects through biomechanical analyses. Zhang et al used an intercalary prosthesis to reconstruct humeral shaft defects following tumor resection, and the prosthesis was designed and manufactured without microporous structures and 3D printing technology [9]. Luenam et al., used 3D printing technology to repair severe distal humerus fractures with complete loss of the lateral column; however, this was structural rather than segmental repair [10]. The present case involved the largest documented humeral defect (13.68 cm) in an elderly patient, further highlighting the versatility of 3D printing technology. While previous studies have employed two-stage procedures incorporating induced membrane formation, our report demonstrates a single-stage reconstruction using a patient-specific prosthesis, potentially minimizing operative morbidity and reducing the duration of hospitalization.
Our case demonstrates that a custom 3D-printed intercalary humerus prosthesis can serve as an effective and practical solution for massive segmental humeral bone loss associated with atrophic non-union, especially in elderly patients where traditional graft-based reconstruction is limited by poor bone quality and high donor-site morbidity. The successful single-stage reconstruction of a 13.68-cm humeral defect, the largest reported to date, highlights the potential of patient-specific 3D printing technology in restoring limb stability, alignment, and function while reducing surgical morbidity. This case is of particular relevance to the fields of orthopedic trauma and limb salvage surgery, offering evidence that personalized 3D-printed implants can address long-bone defects that are otherwise not amenable to conventional techniques.
Custom 3D-printed intercalary humeral prostheses offer a viable solution for managing extensive humeral shaft bone loss with atrophic non-union, particularly in elderly patients where conventional bone grafting is limited by poor bone quality and donor-site morbidity. This case illustrates how patient-specific implant design can restore alignment, stability, and function in a single-stage procedure, providing an effective solution for complex long-bone defects. This technique broadens the reconstructive possibilities for orthopedic surgeons and highlights the expanding role of 3D printing.
References
- 1. Ward EF, Savoie FH 3rd, Hughes JL Jr. Fractures of the diaphyseal humerus. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal Trauma: Fractures, Dislocations, Ligamentous Injuries. Vol. 2. Philadelphia, PA: WB Saunders; 1998. p. 1523-47. [Google Scholar] [PubMed]
- 2. Jupiter JB, Von Deck M. Ununited humeral diaphyses. J Shoulder Elbow Surg 1998;7:644-53. [Google Scholar] [PubMed]
- 3. Pugh DM, McKee MD. Advances in the management of humeral nonunion. J Am Acad Orthop Surg 2003;11:48-59. [Google Scholar] [PubMed]
- 4. Peters RM, Claessen FM, Doornberg JN, Kolovich GP, Diercks RL, Van Den Bekerom MP. Union rate after operative treatment of humeral shaft nonunion–A systematic review. Injury 2015;46:2314-24. [Google Scholar] [PubMed]
- 5. Kiran M, Jee R. Ilizarov’s method for treatment of nonunion of diaphyseal fractures of the humerus. Indian J Orthop 2010;44:444-7. [Google Scholar] [PubMed]
- 6. Bigoni M, Turati M, Arnoldi M, Omeljaniuk RJ, Peri Di Caprio A, Del Bene M, et al. Distal humeral septic non-union treated with debridement and vascularized fibular transfer: Case report and review of the literature. Eur Rev Med Pharmacol Sci 2019;23:12-8. [Google Scholar] [PubMed]
- 7. Qiu W, Liu B, Li X, Tian Y. Novel application of 3D printed microporous prosthesis to repair humeral nonunion with segmental bone defects: A case report. Ann Transl Med 2022;10:840. [Google Scholar] [PubMed]
- 8. Mauffrey C, Barlow BT, Smith W. Management of segmental bone defects. J Am Acad Orthop Surg 2015;23:143-53. [Google Scholar] [PubMed]
- 9. Zhang JF, Wang F, Hu YC. Reconstruction of humeral shaft defect with an intercalary endoprosthesis following resection of tumor. Orthop Surg 2018;10:281-4. [Google Scholar] [PubMed]
- 10. Luenam S, Kosiyatrakul A, Phakdeewisetkul K, Puncreobutr C. The patient-specific implant created with 3D printing technology in treatment of a severe open distal humerus fracture with complete loss of the lateral column. J Orthop Surg (Hong Kong). 2020 Sep-Dec;28(3):2309499020960251. doi: 10.1177/2309499020960251. PMID: 33021150 . [Google Scholar] [PubMed] [CrossRef]