Rigid multiplanar deformities of the knees need excess caution in handling them. Fibular head osteotomy could be one of the methods of lateral contracture release during total knee replacement for fixed valgus arthritic knees.
Dr. Mantu Jain, Department of Orthopaedics, India Institute of Medical Sciences, Bhubaneswar, Odisha, India. E-mail: montu_jn@yahoo.com
Introduction: Total knee replacement in valgus knees is more challenging than in varus knees, which needs meticulous handling and decision-making from the surgical approach to the rehabilitation protocol. In this case, we report an iatrogenic fibula head fracture during total knee replacement for a valgus knee with no concomitant common peroneal nerve palsy. This is the first report of this kind in the literature.
Case Report: We report a case of a 67-year-old male with fixed valgus and flexion deformity of the right knee, who underwent total knee arthroplasty by lateral para-patellar approach and sustained an iatrogenic fibula head fracture without common peroneal nerve palsy. The probable cause could be excess pressure exerted by the assistant holding the Hohmann retractor on the posterior aspect of the tibia and/or during the maneuvers to expose the posterolateral part of the tibia through the lateral para-patellar approach. He had no neurovascular defects postoperatively and has followed the regular rehabilitation protocol with good functional recovery and showing signs of radiological union in progress of the fracture at 2-month follow-up.
Conclusion: Gentle handling of rigid multiplanar deformity valgus arthritic knees is mandatory to prevent complications. A fibula head fracture could be one of the methods of lateral contracture release in rigid valgus knees.
Keywords: Valgus knee, lateral para-patellar approach, posterolateral corner injury, fibula head fracture.
The advent of total knee replacement and, more recently, Robotic-assisted total knee replacement has markedly expanded the treatment options for numerous individuals afflicted with chronic conditions. Despite advancements, complications such as intraoperative fractures persist. The occurrence of these iatrogenic fractures is noted at 0.39%, albeit infrequently [1]. A systematic review and meta-analysis indicated an incidence ranging from 0.2% to 4.4%, with a predominance in females [2]. Valgus deformity of the knee accounts for 10% of the population with osteoarthritis. Valgus knees are characterized by cartilage erosion and remodeling of bony structures, such as the lateral condyle of the femur and the tibial plateau. Variations in soft tissue encompass the tightening of the lateral collateral ligament (LCL), the tendons of the popliteus, hamstring, lateral head of the gastrocnemius, and the iliotibial band [3]. Valgus knee arthroplasty presents greater challenges than varus knee arthroplasty [4,5]. Prior research has documented iatrogenic fractures of the femur and tibia occurring during arthroplasty [1,2]. An intraoperative fibula head avulsion fracture during primary knee arthroplasty has not been documented in the literature. We present a case of valgus arthritic knee with an iatrogenic fibula head avulsion fracture detected intraoperatively, which was managed conservatively without subsequent common peroneal nerve palsy postoperatively.
A 67-year-old male presented with pain and deformity of the right knee for the past 5 years. Clinical examination revealed a rigid valgus and flexion deformity of the right knee, with no distal neurovascular deficits observed. Radiological assessment revealed a fixed valgus of 15° and a flexion deformity of 18° (Fig. 1). He underwent assessment and was scheduled for total knee arthroplasty. Pre-operative investigations were conducted, and a pre-anesthetic assessment was completed to ascertain fitness for surgery.
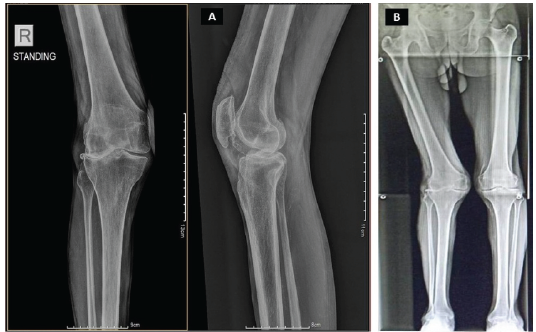
Figure 1: Pre-operative X-ray of right knee (a); Pre-operative scanogram (b).
A midline incision and lateral para-patellar approach were employed, followed by coronal Z-plasty of the capsule retinacular complex. A gradual, titrated sequential release of the laterally constricted structures was executed, including the iliotibial band from Gerdy’s tubercle, lateral osteophytectomy, and lateral capsular detachment from the lateral tibial condyle, succeeded by pie-crusting of the posterior segment of the iliotibial band (Fig. 2a).

Figure 2: Pie-crusting of posterior part of Iliotibial band (a); Trialing of implants (b); and final cementing of prosthesis (c).
In addition, a posterolateral capsular release from the femur was performed. Perpendicular tibial osteotomy, with a 3° valgus correction angle for the distal femoral cut, was performed. Trapezoidal space in extension exhibited lateral tightness. Femoral cuts were made parallel to the trans epicondylar axis. A trapezoidal space observed in flexion, which is relatively diminished compared to extension. To create a rectangular space, posterolateral tibial capsular release is performed by subluxating the tibia anterior to the femur through knee hyperflexion and internal leg rotation, while positioning a Hohmann lever just posterior to the tibial intercondylar area. During this maneuver to expose the posterolateral aspect of the tibia, a faint audible indication occurred. We identified rectangular and symmetrical flexion and extension gaps. The trial implantation with a minimum-size spacer demonstrated stability in both flexion and extension (Fig. 2b). The original prosthesis was affixed with cement (Fig. 2c). Fluoroscopy revealed an iatrogenic fracture of the fibula head (Fig. 3). The knee exhibited stability throughout the range of motion. The post-operative radiographs exhibited no asymmetry (Fig. 4). No common peroneal nerve palsy was present (Fig. 5). He has undergone a standard physiotherapy regimen consisting of weight-bearing and range of motion exercises. Fracture union was evident at 3 months post-operation. He resumed his activities of daily living 3 months post-operation. The Knee Society Score has increased from 34 preoperatively to 90 postoperatively.
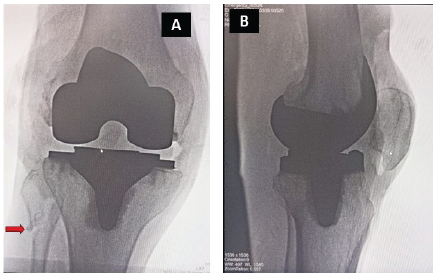
Figure 3: Intraoperative fluoroscopy images showing fibular fracture (red arrow).
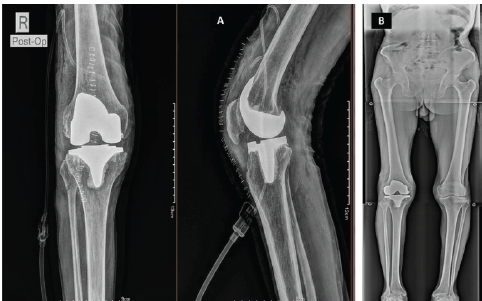
Figure 4: Immediate post-operative X-ray of right knee (a); 2-month follow-up scanogram (b).
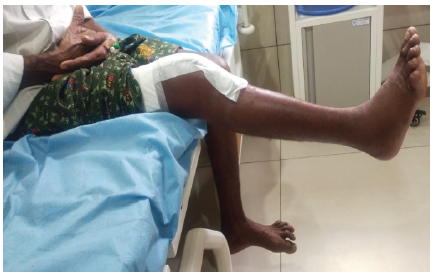
Figure 5: Immediate post-operative ankle dorsiflexion of right ankle (No palsy)
Valgus knees are categorized according to the systems delineated by Ranawat et al. and Mullaji et al [6,7]. The preferred method for addressing rigid valgus deformity is the lateral para-patellar approach [8]. In cases of concomitant flexion deformity, it has been recommended to perform a release of the common peroneal nerve through subperiosteal elevation, along with fibula head osteotomy and excision [6]. Phadnis et al. previously reported a varus knee associated with a fibula head fracture and common peroneal nerve palsy, which resolved spontaneously with conservative treatment [9]. The patient presented with a rigid valgus deformity, and postoperatively, there was no occurrence of nerve palsy. According to Barnett’s classification of the proximal tibiofibular joint, our case is categorized as type III, characterized by a steep inclination and a relatively immobile fibula, along with a minor inclination of the ankle’s dorsiflexion axis. Consequently, excessive dorsiflexion beyond the normal range during the surgery would have transmitted partial load through the distal tibiofibular syndesmosis and interosseous membrane to the proximal tibiofibular joint, likely contributing to increased torsional stress in the fibula, thereby rendering it more susceptible to fracture [10]. Fibular head osteotomy is a challenging procedure because of the vicinity of the common peroneal nerve, which needs prior release [11]. Diverse techniques have been documented to alleviate contracture on the lateral side of rigid multiplanar deformed knees, including Iliotibial band (ITB) release from Gerdy’s tubercle, lateral capsule release, posterolateral capsule release, ITB pie-crusting, LCL and popliteus release, and medial epicondylar osteotomy, contingent upon the patient’s deformity and the condition of the soft tissues [12].
Extreme caution is required when managing patients with valgus knees during clinical examination, throughout the surgical procedure, and during post-operative physiotherapy following total knee replacement. Careful and gentle maneuvers throughout the surgical procedure will aid in preventing complications. Among the various procedures outlined for lateral contracture release, fibula head osteotomy presents a distinct set of advantages and disadvantages.
Iatrogenic fibula head fracture is associated with common peroneal nerve palsy, which needs to be addressed immediately post-operative by placing the knee in flexion, which can recover spontaneously. However, being meticulous while dealing with it and exercising a good caution to prevent it from happening is always the best.
References
- 1. Alden KJ, Duncan WH, Trousdale RT, Pagnano MW, Haidukewych GJ. Intraoperative fracture during primary total knee arthroplasty. Clin Orthop Relat Res 2010;468:90-5. [Google Scholar] [PubMed]
- 2. Purudappa PP, Ramanan SP, Tripathy SK, Varatharaj S, Mounasamy V, Sambandam SN. Intra-operative fractures in primary total knee arthroplasty – a systematic review. Knee Surg Relat Res 2020;32:40. [Google Scholar] [PubMed]
- 3. Rossi R, Rosso F, Cottino U, Dettoni F, Bonasia DE, Bruzzone M. Total knee arthroplasty in the valgus knee. Int Orthop 2014;38:273-83. [Google Scholar] [PubMed]
- 4. Stern SH, Moeckel BH, Insall JN. Total knee arthroplasty in valgus knees. Clin Orthop Relat Res 1991;273:5-8. [Google Scholar] [PubMed]
- 5. Elkus M, Ranawat CS, Rasquinha VJ, Babhulkar S, Rossi R, Ranawat AS. Total knee arthroplasty for severe valgus deformity: Five to fourteen-year follow-up. J Bone Joint Surg Am 2004;86:2671-6. [Google Scholar] [PubMed]
- 6. Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am 2005;87:271-84. [Google Scholar] [PubMed]
- 7. Mullaji AB, Shetty GM. Valgus deformity. In: Deformity Correction in Total Knee. Germany: Springer; 2014. p. 59-71. [Google Scholar] [PubMed]
- 8. Keblish PA. The lateral approach. In: Surgical Techniques in Total Knee Arthroplasty. New York: Springer; 2002. p. 137-48. [Google Scholar] [PubMed]
- 9. Phadnis A, Johnston P, Glasgow M. Avulsion of the fibular head post-total knee replacement. Knee Surg Sports Traumatol Arthrosc 2007;15:1340-2. [Google Scholar] [PubMed]
- 10. Ogden JA. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res 1974;101:186-91. [Google Scholar] [PubMed]
- 11. Xu J, Liu H, Luo F, Lin Y. Common peroneal nerve ‘pre-release’ in total knee arthroplasty for severe valgus deformities. Knee 2020;27:980-6. [Google Scholar] [PubMed]
- 12. LaPrade RF, Ly TV, Wentorf FA, Engebretsen L. The posterolateral attachments of the knee: A qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. Am J Sports Med 2003;31:854-60. [Google Scholar] [PubMed]








