The pre-operative distinction between pediatric modified Gartland Type III and Type IV supracondylar fractures of the humerus is important as it can drastically change the orthopedic surgeon approach and impact surgical outcome, especially when avoiding an open reduction and pinning is the goal. At present, there is a lack of pre-operative gold standard objective clinical and radiographic diagnostic parameters for modified Gartland Type IV supracondylar fractures in children. This pre-operative diagnostic dilemma of Type IV fracture is due to the fact that diagnosis is mostly intraoperative under fluoroscopy, subjective and depends upon the operating surgeon’s clinical experience and expertise rather than evidence, which is scarce and inconclusive. This diagnostic ambiguity leads to inefficient operative planning and can potentially compromise surgical goals. The purpose of this editorial is to resolve the diagnostic dilemma by identifying the pre-operative radiographic signs that accurately and reliably predict modified Gartland Type IV supracondylar fractures of the humerus in children. Since modified Gartland Type IV fractures require open reduction and pinning more frequently than Type III fractures, these radiographic parameters will forecast failure of closed reduction and ensured smooth shift from closed reduction to open reduction and pinning. The operating surgeon would be in position to better plan and prepared for open reduction and counsel the parents about the outcome and prognosis of surgery.
Dr. Muhammad Inam, Orthopaedics and Traumatology Division Lady Reading Hospital, Peshawar, Pakistan. E-mail: dr_mohammadinam@yahoo.co.uk
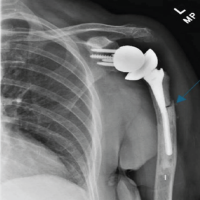
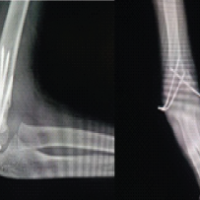
Pediatric supracondylar fractures of the humerus accounts for 18% of all pediatric fractures [1]. They are classified into extension (98%) and flexion (2%) [2]. The extension fractures were classically divided by Gartland into three types in 1959 [3]. Gartland Type I fracture is undisplaced and stable, Gartland Type II fracture is partially displaced and partially stable and Gartland Type III fracture is completely displaced and unstable. In 2006, Leitch et al. [4] added a fourth “Multidirectionally Unstable” fracture, which results from circumferential tearing of the periosteum and is unstable in both flexion and extension. Leitch labeled this variant as a modified Gartland Type IV fracture and reported that its incidence varies from 7% to 10%. Modified Gartland Type IV fracture is usually diagnosed intraoperatively under fluoroscopy [5]. The gold standard treatment for Gartland Type III and Type IV fracture is closed reduction and percutaneous pinning [4]. Open reductions and pinning, however, are needed in Gartland Type III and more often in modified Gartland Type IV fractures, which are difficult to treat with closed reduction and percutaneous pinning [6,7].
The pre-operative diagnosis of modified Gartland Type IV fracture is extremely subjective as it is usually diagnosed intraoperatively by the operating surgeon [8,9]. This diagnostic dilemma is due to little information on this subject and a lack of gold standard pre-operative radiographic parameters for confidentially diagnosing modified Gartland Type IV fracture. After extensive searching the literature, we were able to find only a few relevant studies on this topic. Mitchell et al. [10] reviewed the records of 39 Type IV fractures and noted five pre-operative radiographic parameters which were more frequently associated with Type modified Gartland IV fractures than Type III fractures. These five radiographic parameters were Flexion Angulation (odds ratio [OR] = 17, 95% confidence interval [CI] = 4.9–59), Valgus Angulation (OR = 5.6, 95% CI = 1.6–20), Lateral Translation of the distal fragment (OR = 4.1, 95% CI = 1.6–11), bony contact between the proximal and distal fracture fragment (OR = 4.0, 95% CI = 1.8–9.0) and extension of fracture line to proximal diaphysis fragment (OR = 9.2, 95% CI = 1.6–53). Mitchell concluded that although overlap exists between Type III and IV fractures, Type IV fractures required open reduction more frequently than Type III and with longer operative time than Type III fractures. Barik et al. [9] reviewed the records of 33 patients (type III fractures = 16, Type IV fractures = 17) They documented that pre-operative elbow radiographs indicating ≥17 degrees’ valgus angulation of the distal fragment (OR = 20.22, 95% CI = 3.45–118.65) and ≥10 degrees flexion angulation (OR = 5.32, 95% CI = 0.24–119.88) of the distal fracture fragment had a sensitivity of 41% and specificity of 100% for predicting type IV fracture. Yigit et al. [8] treated 99 patients of Gartland Type III and 21 with modified Gartland Type IV fractures. These authors noted that pre-operative radiographs showing varus or valgus angulation of more than 25.5° (OR = 1.725, 95% CI = 1.170 2, 541, P = 0.001, r = 0.616, sensitivity = 81%, specificity = 85%), and amount of bony apposition more than 9.5 mm (OR = 1.471, 95% CI = 0.714–3.029, P = 0.001, r = 0.433, sensitivity = 85%, specificity = 81%) were more relevant for predicting modified Type IV fractures than Type III fractures.
Contrary to the above studies, Soldado et al., [11] is of the opinion that a lateral radiograph of the elbow can mislead an Orthopaedic surgeon for deciding fracture displacement and fracture classification. He presumed that trauma to the elbow results in more circumferential loss of periosteum in the coronal plane and that can be the reason that AP radiograph are more specific for indicating displacement of fracture fragment than lateral radiographs. He noted that lateral translation or angulation (Valgus Type) and medial translation or angulation (Varus type) on AP radiograph were more predictive of Type IV fracture. Abraham et al. [12] revealed that modified Gartland Type IV fracture is seen in both flexion and extension types, and the frequency of Type IV extension supracondylar fracture is 0.9%. Abraham presented a case report of an extension supracondylar Type IV fracture and successfully operated with a modified technique of closed reduction and percutaneous pinning.
Pre-operative diagnosis of a modified Gartland Type IV fracture in children is extremely subjective. No consensus has been achieved regarding the gold standard pre-operative radiographic criteria. Although limited evidence is available, the operating surgeon can predict a modified Gartland Type IV fracture based on assessment of multiple radiographic signs. These may include flexion angulation, valgus angulation, lateral translation of the distal fragment, bony contact between the proximal and distal fracture fragment, and extension of the fracture line to proximal diaphysis fragment on good-quality pre-operative AP and lateral view radiographs of the elbow. Further good quality research is also needed to identify not only radiographic but non-radiographic parameters such as injury-related factors (mechanism, severity) and patient-related factors (delay in surgery, obesity, age) for predicting Type IV fractures. New validated techniques for closed reduction and percutaneous pinning of modified Gartland Type IV fractures need to be devised. We also recommend that every Orthopaedic surgeon should master both the techniques of closed reduction and percutaneous pinning and open reduction and pinning of modified Gartland Type IV fractures in children.
References
- 1. Kim TJ, Sponseller PD. Pediatric supracondylar humerus fractures. J Hand Surg Am 2014;39:2308-11; quiz 2311. [Google Scholar] [PubMed]
- 2. Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg Am 2008;90:1121-32. [Google Scholar] [PubMed]
- 3. Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet 1959;109:145-54. [Google Scholar] [PubMed]
- 4. Leitch KK, Kay RM, Femino JD, Tolo VT, Storer SK, Skaggs DL. Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified Gartland type-IV fracture. J Bone Joint Surg Am 2006;88:980-5. [Google Scholar] [PubMed]
- 5. Pei X, Mo Y, Huang P. Leverage application on Gartland type IV supracondylar humeral fracture in children. Int Orthop 2016;40:2417-22. [Google Scholar] [PubMed]
- 6. Novais EN, Andrade MA, Gomes DC. The use of a joystick technique facilitates closed reduction and percutaneous fixation of multidirectionally unstable supracondylar humeral fractures in children. J Pediatr Orthop 2013;33:14-9. [Google Scholar] [PubMed]
- 7. Transtrum MB, Sanchez D, Griffith S, Godinez B, Singh V, Klahs KJ, et al. Predictors associated with the need for open reduction of pediatric supracondylar humerus fractures: A meta-analysis of the recent literature. JB JS Open Access 2024;9:e24.00011. [Google Scholar] [PubMed]
- 8. Yigit S, Aslan R, Arslan H, Ozkul E, Atic R, Akar MS. Predictive factors for the development of Gartland type IV supracondylar humerus fractures: A prospective clinical study. Acta Orthop Traumatol Turc 2022;56:361-5. [Google Scholar] [PubMed]
- 9. Barik S, Singh G, Maji S, Azam MQ, Singh V. Preoperative prediction of Gartland IV supracondylar fractures of humerus: Is it possible? Rev Bras Ortop (Sao Paulo) 2021;56:230-4. [Google Scholar] [PubMed]
- 10. Mitchell SL, Sullivan BT, Ho CA, Abzug JM, Raad M, Sponseller PD. Pediatric Gartland Type-IV supracondylar humeral fractures have substantial overlap with flexion-type fractures. J Bone Joint Surg Am 2019;101:1351-6. [Google Scholar] [PubMed]
- 11. Soldado F, Hodgson F, Barrera-Ochoa S, Diaz-Gallardo P, Garcia-Martinez MC, Ramirez-Carrasco TR, et al. Gartland Type-IV supracondylar humeral fractures: Preoperative radiographic features and a hypothesis on causation. Orthop Traumatol Surg Res 2022;108:103049. [Google Scholar] [PubMed]
- 12. Abraham E, Deshpande A, Lichtig A, Paladino L. A Type IV extension supracondylar fracture with comminuted fracture pattern: A case report. J Am Acad Orthop Surg Glob Res Rev 2023;7:e23.00020. [Google Scholar] [PubMed]