Split tears of the peroneus brevis tendon, often associated with superior peroneal retinaculum (SPR) insufficiency, are an under-recognized cause of chronic lateral ankle pain and instability. Diagnosis relies on a high index of suspicion and is best supported by dynamic imaging such as ultrasound or MRI. When conservative management fails, surgical repair with tendon tubularization and SPR reconstruction, followed by structured rehabilitation, can restore stability and enable full return to activity.
Dr. Tushar Nayak, Department of Orthopaedics, Sparsh Hospital, Hennur Road, Bengaluru - 560066, Karnataka, India. E-mail: orthodrtushar@gmail.com
Introduction: Split tears of the peroneus brevis tendon (PBT), often associated with superior peroneal retinaculum (SPR) insufficiency, are a frequently overlooked cause of posterolateral ankle pain and instability, particularly in athletes. Accurate diagnosis requires a high index of suspicion and dynamic imaging to detect tendon subluxation and associated pathology.
Case Report: We present the case of a 28-year-old athlete with persistent posterolateral ankle pain and instability following an ankle twist. Clinical examination and imaging confirmed a partial longitudinal tear of the PBT with concomitant SPR insufficiency. Surgical management involved tendon debridement, tubularization with side-to-side repair, and SPR reconstruction. Post-operative rehabilitation included progressive weight-bearing, range-of-motion exercises, and structured strengthening protocols.
Conclusion: The patient achieved excellent recovery, with an American Orthopaedic Foot and Ankle Society Ankle-Hindfoot Score of 85 at 3 months and a full return to sports without pain or instability. This case highlights the importance of early recognition and comprehensive management of both tendon and ligament pathology to achieve optimal functional outcomes.
Keywords: Peroneus brevis tendon, ankle instability, superior peroneal retinaculum, tendon repair, rehabilitation.
Peroneus brevis tendon (PBT) instability is a rare but significant cause of posterolateral ankle pain, often presenting with symptoms such as retromalleolar pain and functional instability. It frequently coexists with lateral ankle ligament insufficiency, and the contributing factors include a low-lying peroneus muscle belly, accessory muscles such as the peroneus quartus, retromalleolar groove abnormalities, and chronic ankle instability [1,2]. A high body mass index, eccentric inversion, and rapid plantar flexion in sports increase the risk of ankle sprains and peroneus split tears, especially in athletes. Related factors include retromalleolar groove irregularities [3], concave grooves, and prominent ridges causing instability [3,4]. Post-traumatic superior peroneal retinaculum (SPR) instability leads to tendon subluxation and split tears, especially after ankle sprains [5]. This report describes the surgical approach and post-operative outcomes of a patient with a peroneus brevis longitudinal tendon tear, demonstrating the efficacy of anatomical repair in restoring full functionality and enabling pre-injury activities.
A 28-year-old male athlete presented with ongoing pain and instability localized to the posterolateral aspect of his left ankle. He sustained a high-impact ankle twist that was managed conservatively. After an initial period of recovery, his symptoms gradually worsened over time, with a history notable for multiple recurrent ankle sprains, particularly during high-impact activities. The pain was localized to the retromalleolar region, accompanied by swelling and tenderness along the posterolateral ankle, behind the fibula. A snapping or clicking sensation was present along the peroneal tendons during eversion and dorsiflexion of the foot (Video 1). He also experienced episodes of ankle instability, with a tendency for the foot to give way, especially on uneven surfaces.
On examination, there was tenderness over the fibular groove and along the peroneal tendon course. Pain was elicited with resisted ankle eversion and dorsiflexion. The peroneal tendon subluxation test was positive, with dynamic subluxation of the peroneal tendons observed when the foot was actively dorsiflexed and everted against resistance. In addition, there was weakness in eversion strength, particularly in cases of chronic pathology.
Imaging findings
- Standard radiographs: Appeared normal (Fig. 1a)
- Dynamic ultrasound (USG): Demonstrated tendon subluxation, a longitudinal split tear of the PBT, and a SPR tear. USG also revealed peroneal tendon snapping over the fibula, confirming mechanical instability
- Magnetic resonance imaging (MRI): With greater displacement, a split tear of the peroneus brevis appeared as multiple subtendons. Subluxation of the split tendon was present, accompanied by a SPR tear. The split fragments of the peroneus brevis were displaced by the peroneus longus (Fig. 1b, c, d).
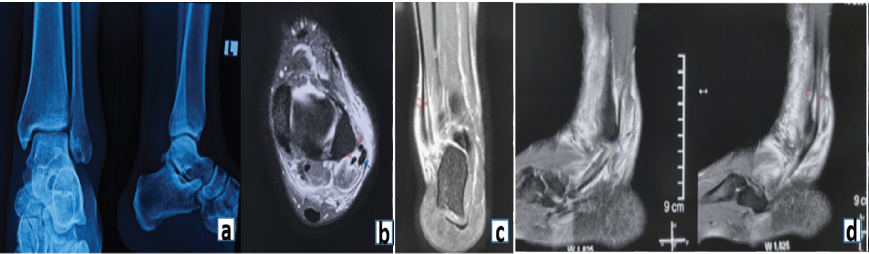
Figure 1: (a) Representative radiograph demonstrating normal appearance. (b) Transverse magnetic resonance imaging (MRI) image showing high signal intensity within the peroneus brevis tendon at the lateral malleolar level (red arrows). The peroneus longus tendon (blue arrows) appears normal. (c) Coronal MRI image demonstrating a longitudinal tear in the peroneus brevis tendon. (d) Sagittal MRI image demonstrating the longitudinal tear in the peroneus brevis tendon (red arrows) and a normal peroneus longus tendon (black arrow).
Surgical management
The patient underwent repair of the PBT tendon through a standard posterolateral approach. A key intraoperative finding was the subluxation of the anterior half of the PBT over the sharp posterior edge of the fibula, accompanied by detachment of the SPR from the posterior fibular ridge (Fig. 2a and b).
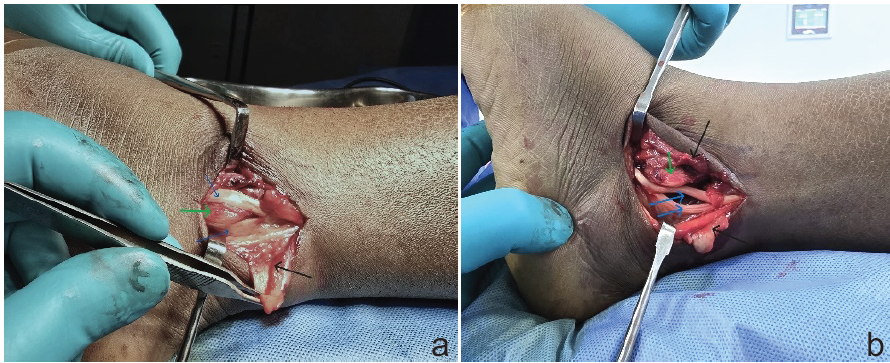
Figure 2: (a and b) Relationship between the longitudinal tear in the peroneus brevis tendon (blue arrows), the sharp posterior edge of the fibula (green arrow), and the torn superior peroneal retinaculum (black arrow).
The surgical steps included:
Tendon repair consisted of excision of the frayed and degenerated tissue and tubularization with side-to-side repair of the PBT (Fig. 3a and b) with non-absorbable sutures.
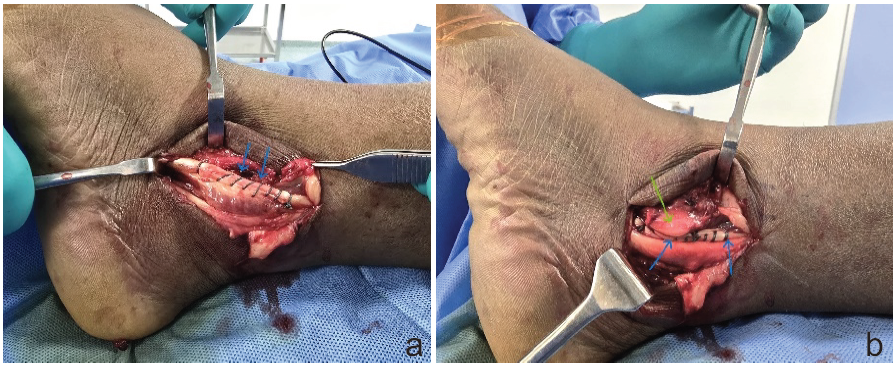
Figure 3: (a and b) Side-to-side repair of the partial longitudinal tear of the peroneus brevis tendon, followed by reconstruction of the superior peroneal retinaculum.
Reconstruction of the SPR
Underlying tendon instability and subluxation were given careful attention at the time of the procedure to prevent recurrence, and careful attention was paid to reconstruct the volume and tightness of the SPR so that the tendons are neither compressed nor able to subluxate using a pants over vest repair technique (Video 2).
Postoperative rehabilitation
The ankle was immobilized in a plaster back slab for 2 weeks, followed by an Aircast brace for range-of-motion training. The rehabilitation protocol included:
- Weeks 3–6: Progressive weight-bearing and mobility exercises
- Weeks 6–8: Coordination training with tilt boards
- Weeks 8–12: Strength training with weight boots
- Week 12 onward: Return to sports if stability was achieved and swelling resolved. Ankle support (taping or brace) was used as needed.
Outcomes
The patient achieved a postoperative American Orthopaedic Foot and Ankle Society Ankle-Hindfoot Score [6] of 85, indicating good functional recovery. At the 3-month follow-up, he had returned to his pre-injury level of activity without pain or instability. The ankle demonstrated full mobility and normal strength, allowing him to perform daily activities comfortably and resume sports without limitation.
Peroneus brevis split tears are an uncommon yet clinically important cause of posterolateral ankle pain and instability. Although relatively rare, they are encountered more often than complete ruptures and may result in intra-sheath instability when the peroneus longus tendon subluxates through the torn brevis [3,7]. The condition is frequently overlooked because symptoms mimic chronic lateral ankle instability, and imaging findings may be subtle. Dynamic USG or MRI is particularly useful in confirming tendon subluxation and identifying associated injuries, especially when SPR insufficiency is present [7]. Management decisions are largely guided by the extent of tendon involvement. Krause and Brodsky [8] proposed a grading system in which Grade 1 tears (<50% cross-sectional area) are treated with debridement and tubularization, while Grade 2 tears (>50%) require resection and tenodesis to the peroneus longus. Redfern and Myerson [9] expanded on this to address complex situations, including concomitant peroneus longus pathology, recommending tenodesis or tendon transfer when excursion is compromised. These algorithms emphasize that surgical planning should consider not only the degree of tendon damage but also the presence of SPR insufficiency and structural variations such as retromalleolar groove irregularities. Clinical outcomes following surgical intervention have generally been favorable but remain variable [10]. Krause and Brodsky [8] reported over 90% patient satisfaction, particularly with tubularization procedures. Demetracopoulos et al. [11] observed excellent pain relief and a 94% return to sports following debridement and repair, while Steginsky et al. [12] noted that 76% of patients resumed pre-injury activities with high satisfaction. Conversely, Steel and DeOrio [13] reported lower return-to-sport rates, with only 46% achieving full participation and a notable proportion experiencing persistent symptoms. These differences highlight the importance of accurate grading, appropriate patient selection, and meticulous surgical technique in achieving consistent results. Our case supports the growing evidence that early recognition of peroneus brevis split tears with concomitant SPR insufficiency, followed by anatomical repair and structured rehabilitation, can restore ankle stability and function. By addressing both tendon and ligament pathology, patients can reliably regain pre-injury levels of activity with minimal long-term impairment.
Peroneal tendon injuries, particularly split tears of the PBT, remain an under-recognized cause of lateral ankle pain and dysfunction. Diagnosis can be challenging, as imaging findings with MRI and USG are often variable and sometimes inconclusive. This case demonstrates the effectiveness of a comprehensive treatment strategy that combines precise anatomical repair with a structured rehabilitation program. Addressing both tendon and associated ligament pathology is critical for restoring ankle stability and function. Early recognition, accurate diagnosis, and individualized management are key to achieving reliable long-term outcomes.
PBT splits should be suspected in patients with recurrent ankle sprains and persistent posterolateral ankle pain or instability. Careful clinical evaluation, supported by dynamic imaging, improves diagnostic accuracy. When conservative treatment fails, surgical repair with SPR reconstruction offers predictable outcomes, enabling patients to regain stability, prevent chronic disability, and safely return to activity.
References
- 1. Adachi N, Fukuhara K, Kobayashi T, Nakasa T, Ochi M. Morphologic variations of the fibular malleolar groove with recurrent dislocation of the peroneal tendons. Foot Ankle Int 2009;30:540-4. [Google Scholar] [PubMed]
- 2. Chauhan B, Panchal P, Szabo E, Wilkins T. Split peroneus brevis tendon: An unusual cause of ankle pain and instability. J Am Board Fam Med 2014;27:297-302. [Google Scholar] [PubMed]
- 3. DIGiovanni BF, Fraga CJ, Cohen BE, Shereff MJ. Associated injuries found in chronic lateral ankle instability. Foot Ankle Int 2000;21:809-15. [Google Scholar] [PubMed]
- 4. Strauss JE, Forsberg JA, Lippert FG 3rd. Chronic lateral ankle instability and associated conditions: A rationale for treatment. Foot Ankle Int 2007;28:1041-4. [Google Scholar] [PubMed]
- 5. Bonnin M, Tavernier T, Bouysset M. Split lesions of the peroneus brevis tendon in chronic ankle laxity. Am J Sports Med 1997;25:699-703. [Google Scholar] [PubMed]
- 6. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 1994;15:349-53. [Google Scholar] [PubMed]
- 7. Bokwa-Dąbrowska K, Mocanu D, Romanus I, Zych R, Huuskonen M, Szaro P. Peroneus brevis split tear – A challenging diagnosis: A pictorial review of magnetic resonance and ultrasound imaging – Part 2: Imaging with magnetic resonance and ultrasound. Eur J Radiol Open 2025;14:100627. [Google Scholar] [PubMed]
- 8. Krause JO, Brodsky JW. Peroneus brevis tendon tears: Pathophysiology, surgical reconstruction, and clinical results. Foot Ankle Int 1998;19:271-9. [Google Scholar] [PubMed]
- 9. Redfern D, Myerson M. The management of concomitant tears of the peroneus longus and brevis tendons. Foot Ankle Int 2004;25:695-707. [Google Scholar] [PubMed]
- 10. Kerkhoffs GM, Handoll HH, De Bie R, Rowe BH, Struijs PA. Surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults. Cochrane Database Syst Rev 2007;???:CD000380. [Google Scholar] [PubMed]
- 11. Demetracopoulos CA, Vineyard JC, Kiesau CD, Nunley JA 2nd. Long-term results of debridement and primary repair of peroneal tendon tears. Foot Ankle Int 2014;35:252-7. [Google Scholar] [PubMed]
- 12. Steginsky B, Riley A, Lucas DE, Philbin TM, Berlet GC. Patient-reported outcomes and return to activity after peroneus brevis repair. Foot Ankle Int 2016;37:178-85. [Google Scholar] [PubMed]
- 13. Steel MW, DeOrio JK. Peroneal tendon tears: Return to sports after operative treatment. Foot Ankle Int 2007;28:49-54. [Google Scholar] [PubMed]