Early recognition with anatomical fixation and timely surgery followed by structured rehabilitation leads to superior functional outcomes in volar lip fractures of the middle phalanx, whereas delayed or neglected cases require complex reconstruction with reduced motion and higher disability.
Dr. Jaideep Das, Department of Orthopaedics, GGMC and JJH, Mumbai, Maharashtra, India. E-mail: jaideepdas01@gmail.com
Introduction: Volar lip fractures of the middle phalanx are uncommon but potentially debilitating intra-articular injuries, typically resulting from axial loading combined with hyperextension or dorsal dislocation. They frequently involve avulsion of the volar base of the middle phalanx along with the volar plate, compromising joint congruity and stability. The management of such fractures ranges from non-operative care for small stable fragments to open reduction and internal fixation, volar plate repair, hemi-hamate arthroplasty, or dynamic external fixation in unstable or chronic cases.
Case Series: This series reports five cases of volar lip fractures of the middle phalanx presenting at variable intervals and managed with variable surgical techniques at a tertiary care center which includes: (1) Mini-screw fixation in acute case, (2) mini-screw fixation combined with K-wire stabilization, (3) hemi-hamate arthroplasty, (4) JESS external fixation, (5) mini-screw fixation in a chronic case. Post-operative care included protective splinting for 2–4 weeks, suture removal at 2–3 weeks, and initiation of mobilization with strapping, followed by structured physiotherapy. Comparative analysis revealed that acute cases (Cases 1, 2, and 4) achieved superior outcomes with primary fixation techniques, showing better post-operative proximal interphalangeal joint range of motion, lower Disabilities of the Arm, Shoulder and Hand (DASH) scores, and lower Visual Analog Scale (VAS) pain scores. Chronic cases (Cases 3 and 5) required reconstructive or delayed fixation, yielding restricted motion, higher DASH scores, and higher VAS scores.
Conclusion: Volar lip fractures of the middle phalanx, though rare, have significant functional implications. Early anatomical reduction and fixation provide the best chance for restoring stability, mobility, and hand function. Chronic or neglected injuries often demand salvage procedures such as hemi-hamate arthroplasty, which can achieve functional but limited outcomes. Our case series highlights that timely surgical intervention and structured rehabilitation are key determinants of optimal recovery.
Keywords: Volar lip fracture, proximal interphalangeal joint, hemi-hamate arthroplasty, mini-screw fixation, Jess external fixator.
Volar lip fractures of the middle phalanx are intra-articular fractures of the volar base of the middle phalanx, usually associated with dorsal proximal interphalangeal (PIP) dislocation and volar plate avulsion [1]. It represents a fracture–dislocation injury, where a fragment of the volar base of the middle phalanx is avulsed along with the attachment of the volar plate, usually occurring because of axial load combined with hyperextension or dorsal dislocation of the PIP joint. These are unstable fracture-dislocations of the PIP joint involving the volar articular margin of the middle phalanx, often compromising joint congruity and stability [2]. The primary stability of the PIP joint is provided by its bony articular surface, the proper and accessory collateral ligaments, and the volar plate. Secondary stability is afforded by the flexor and extensor tendons. The fracture pattern at the base of the middle phalanx depends on the direction of the force and position of the joint [3]. A combination of longitudinal load and either hyperextension or hyperflexion causes dorsal or volar fracture dislocations, respectively [4,5]. A predominantly axial load disrupts both the dorsal and volar cortices of the middle phalanx base, creating, by definition, a pilon fracture. Volar lip fracture with PIP–dislocations at about 9/100,000/year, whereas finger/phalangeal fractures overall range widely (≈18–99/100,000/year) depending on region [6].
Management of such fracture includes
Non-operative care (small and stable fragments): Extension splinting or protected early mobilization; indicated for stable avulsions where anatomic reduction is maintained, and the joint is congruent. Good outcomes are reported in the textbook series [7].
Closed reduction + percutaneous fixation: Extension-block (flexion) pinning or transarticular K-wires to hold reduction are effective for many dorsal fracture-dislocations with medium-sized fragments. Minimally invasive, preserves soft tissues. Commonly used when fragments are reducible and not grossly comminuted [8].
Open reduction and internal fixation (ORIF): Indicated for larger single fragments that can be anatomically reduced and fixed with small screws, headless compression screws, or miniplates/pins. Best when fracture geometry allows secure fixation and early motion [9].
Volar-plate arthroplasty/Volar plate repair: Reconstruction of the volar rim with volar-plate advancement/repair (sometimes with suture anchors) can restore stability in acute/chronic dorsal subluxations when the fragment is small or unsalvageable. Several series report good functional arcs with this technique [10].
Hemi-hamate (autograft) arthroplasty: Indicated for large or comminuted volar rim defects involving >50% of the articular surface or when the fragment cannot be reliably reconstructed. Hemi-hamate provides a structural osteochondral graft to reconstruct the volar lip – good outcomes reported in multiple series [11].
Dynamic external fixation/Distraction-traction: Useful for severely comminuted fractures or when soft-tissue swelling prevents immediate ORIF. The device maintains reduction while allowing early active/passive range of motion (ROM), improving functional results in unstable injuries [12]. Chronic injuries and salvage: For chronic subluxation or arthritis after volar-lip injury, options include hemi-hamate (primary or salvage), volar-plate arthroplasty, arthrodesis (PIP fusion) for pain/instability in low-demand patients, or limited arthroplasty in select cases. Choice depends on patient age, demands, and residual cartilage [13]. Rehabilitation and expected outcomes: Early controlled motion (when fixation or external fixation permits) improves the final ROM and limits stiffness; however, this must be balanced against the stability of fixation and articular congruity. With appropriate technique, many patients achieve a functional arc, though residual stiffness or some loss of flexion is common in complex injuries. Complications to watch for: Joint stiffness, persistent instability/subluxation, post-traumatic osteoarthritis, graft donor-site morbidity (for hemi-hamate), pin-tract infection (for external fixation/K-wires), and need for secondary procedures [13]
This case series was conducted at a tertiary care hospital between October 2024 and February 2025 and included five patients diagnosed with volar lip fractures of the middle phalanx of the fingers. Patients were identified from emergency and outpatient records and evaluated clinically and radiographically.
Inclusion and exclusion criteria
Patients aged 15–60 years presenting with a fracture of the volar lip of the middle phalanx were included. Both acute and chronic cases were considered, with acute cases defined as presentation within 3 weeks of injury, and chronic cases defined as presentation after 3 weeks or with features of malunion, subluxation, or persistent instability. Patients with open fractures associated with extensive soft-tissue loss, those with concomitant neurovascular compromise requiring vascular repair, individuals outside the specified age group, and those with systemic comorbidities precluding surgery or follow-up were excluded.
Pre-operative assessment and surgical technique
All patients underwent detailed history-taking, clinical examination, and radiological evaluation with anteroposterior, lateral, and oblique X-rays of the affected finger. Pre-operative assessment included routine blood investigations, an electrocardiogram, and anesthetic clearance. Surgical management was tailored to the fracture pattern and timing of presentation, with fixation techniques ranging from mini-screw fixation and K-wire stabilization to external fixation or hemi-hamate arthroplasty for chronic cases. Post-operative care included protective splinting, suture removal at 2–3 weeks, and initiation of mobilization with strapping, followed by structured physiotherapy.
Outcome assessment
Patients were followed up at 2 weeks, 4 weeks, 6 weeks, and 12 weeks, and outcomes were assessed using multiple parameters. Pain relief was evaluated using the Visual Analog Scale (VAS), ROM of the PIP joint was measured in degrees, radiological assessment was performed to determine stability and joint congruity, and functional recovery was assessed using the Disabilities of the Arm, Shoulder, and Hand (DASH) scoring system.
Case 1
A 28-year-old male presented with a volar lip fracture of the middle phalanx of the left little finger, 20 days after injury. The fracture was managed with mini-screw fixation using a volar approach. Postoperatively, the patient was discharged with a dorsal splint applied in wrist extension with flexion at the metacarpophalangeal (MCP), PIP, and distal interphalangeal (DIP) joints, allowing full flexion with extension block for 2 weeks. After suture removal at 2 weeks, mobilization was initiated with strapping, and on follow-up, the patient achieved a post-operative ROM of 20–90° at the PIP joint (Fig. 1, 2).

Figure 1: Pre-operative left hand clinical pictures and X-rays (a) left hand clinical picture volar aspect, (b) left hand clinical picture dorsal aspect, (c) X-ray left hand AP view, (d) X-ray left little finger lateral view.
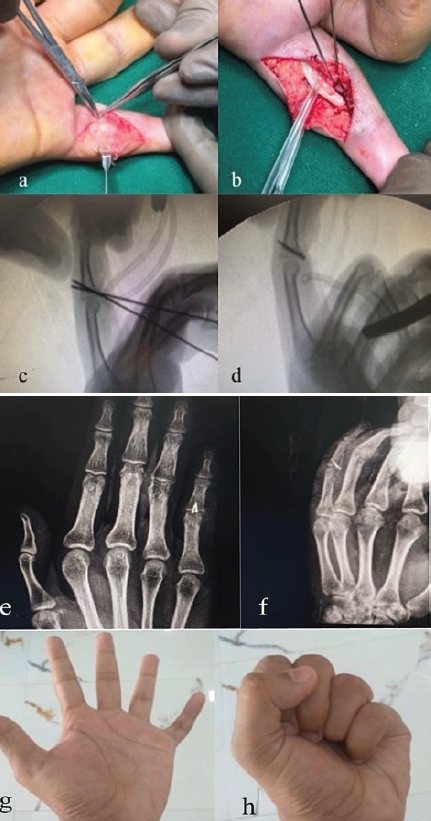
Figure 2: Intra-Operative Clinical Pictures, C-Arm Shoots, Post Operative X-Rays & Follow Up ROM Clinical Picture (a) Volar Incision Taken Over Little Finger, (b) Flexor Tendon Retracted, K-wires placed, (c) C-arm shoot showing K-Wires, (d) C-arm shoot showing Mini-Screws, (e) Post-Operative X-Ray Left Hand AP View, (f) Post-Operative X-Ray Left Hand Oblique View, (g) 6 weeks Follow Up Image showing Finger Extension, (h) 6 weeks Follow Up Image showing Finger Flexion
Case 2
A 46-year-old male presented with a volar lip fracture of the middle phalanx of the left index finger, 25 days after trauma. Surgical management involved mini-screw fixation combined with K-wire stabilization, the K-wire serving as an extension block and removed after 3 weeks. The volar shotgun approach was utilized. Postoperatively, the patient was discharged with a dorsal splint in wrist extension with flexion at MCP, PIP, and DIP joints, allowing full flexion with an extension block for 3 weeks. Mobilization with strapping was initiated after suture removal at 3 weeks. On follow-up, the patient achieved a ROM of 0–90° at the PIP joint (Fig. 3).
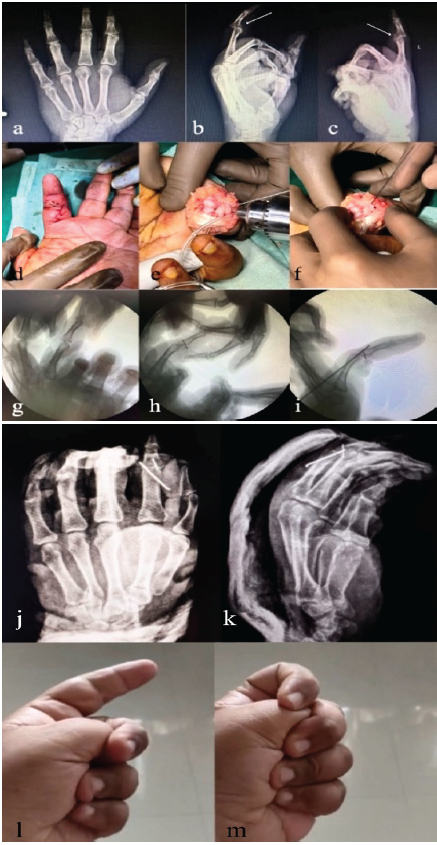
Figure 3: Pre-Operative X-Rays, Intra-Operative Clinical Pictures, C-Arm Shoots, Post Operative X-Rays & Follow Up Clinical Pictures (a) Pre-Operative X-Ray Left Hand AP View, {(b), (c)} Pre-Operative X-Ray Left Index Finger Lateral, (d)Incision at volar aspect of Left Index Finger, {(e), (f)} Intra-Op Image showing Shotgun Approach, (g) C-Arm Shoot showing Index Finger, (h) C – arm Shoot showing mini-screw over the volar lip, (i) C-Arm Shoot showing mini-screw over volar lip and K-wire acting as extension block, (j) Post-Operative X-Rays X-Ray Left Hand AP View, (k) Post-Operative X-Rays X-Ray Left Hand Oblique View, (l) 6 weeks Follow Up Image showing Finger Extension, (m) 6 weeks Follow Up Image showing Finger Flexion
Case 3
A 21-year-old male presented approximately 60 days post-injury with a malunited volar lip fracture of the middle phalanx of the right third finger associated with dorsal subluxation. He was managed with hemi-hamate arthroplasty performed through a shotgun approach. Postoperatively, he was discharged with a dorsal splint in wrist extension with flexion at MCP, PIP, and DIP joints, with a full flexion and extension block maintained for 3 weeks. Suture removal was carried out at 3 weeks, and mobilization with strapping was initiated. On follow-up, the patient achieved a post-operative ROM of 0–70° at the PIP joint (Fig. 4).

Figure 4: Pre-Operative X-Rays, Intra-Operative C-Arm Shoots, Clinical Pictures, Post Operative X-Rays & 6 Weeks Follow Up ROM Clinical Pictures (a) X-Ray Right Hand AP View, (b) X-Ray Right third finger Lateral View, {(c), (d)} C-arm shoots showing autograft fixed with mini screws, (e) Incision over Volar aspect of third finger, (f) shotgun approach, (g) incision & exposure over dorsal aspect for hemi-hamate autograft, {(i),(j)} fixation of autograft with help of mini screws, (k) Post Operative X-Ray Right Hand AP View, (l)Post Operative X-Ray Right third finger Lateral View, (m) 6 Weeks Follow Up Image showing Finger Extension, (n) 6 Weeks Follow Up Image showing Finger Flexion
Case 4
A 36-year-old male presented 7 days after trauma with a post-traumatic volar lip fracture of the middle phalanx of the left index finger. He was managed with a JESS external fixator. The patient was discharged with the external fixator in situ, which was removed after 4 weeks, and mobilization was started immediately thereafter. At follow-up, the patient achieved a ROM of 0–70° at the PIP joint (Fig. 5).

Figure 5: Pre Operative & Post Operative X-Rays, Post Jess Fixator Removal X-Rays & 6 Weeks Follow Up ROM Clinical Pictures (a) X-Ray Left Hand AP View, (b) X-Ray Left Index Finger Lateral View, (c) X-Ray Left Hand AP View showing Jess Fixator, (d) X-Ray Left Index Finger Lateral View, (e) Post Jess Fixator Removal X-Ray Left Hand AP View, (f) Post Jess Fixator Removal X-Ray Left Index Finger Lateral View, (g) Follow Up Image showing Finger Extension, (h) Follow Up Image showing Finger Flexion
Case 5
A 30-year-old male presented 6 weeks post-injury with a volar lip fracture of the middle phalanx of the right little finger. He was managed with mini-screw fixation performed via a shotgun approach. Postoperatively, the patient was discharged with a dorsal splint applied in wrist extension with flexion at MCP, PIP, and DIP joints, allowing full flexion with an extension block for 2 weeks. After suture removal at 2 weeks, mobilization with strapping was initiated. On follow-up, the patient achieved a post-operative ROM of 0–60° at the PIP joint (Fig. 6).
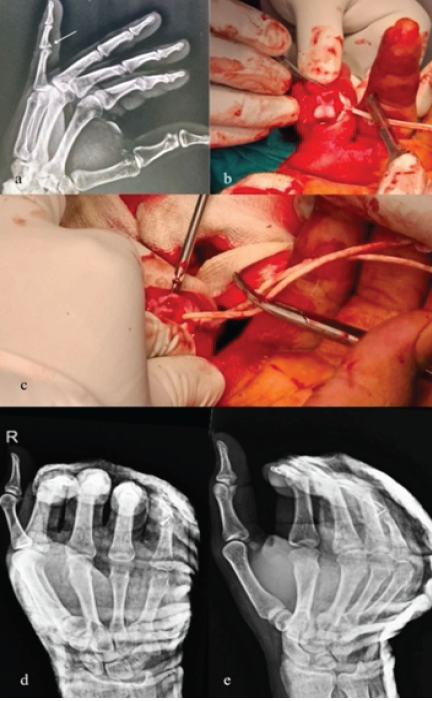
Figure 6: Pre Operative Xray, Intra-Operative Clinical Pictures & Post Operative X-Rays (a) X-Ray Right little Finger Lateral View, (b) Intra-Operative Clinical Picture Showing Shotgun Approach, (c) Intra-Operative Clinical Picture Showing mini-screw fixation, (d) Post Operative X-Ray Right Hand AP View, (e) Post Operative X-Ray Right Hand Oblique View
Clinical and functional outcomes of volar lip fracture cases are mentioned in Table 1. The acute group (Cases 1, 2, and 4) achieved better post-operative ROM, with flexion at the PIP joint reaching up to 90°, whereas the chronic group (Cases 3 and 5) demonstrated restricted final motion, limited to 60–70° of flexion. This limitation in chronic cases was likely due to prolonged immobilization, fibrosis, and persistent articular incongruity at the time of surgical intervention.
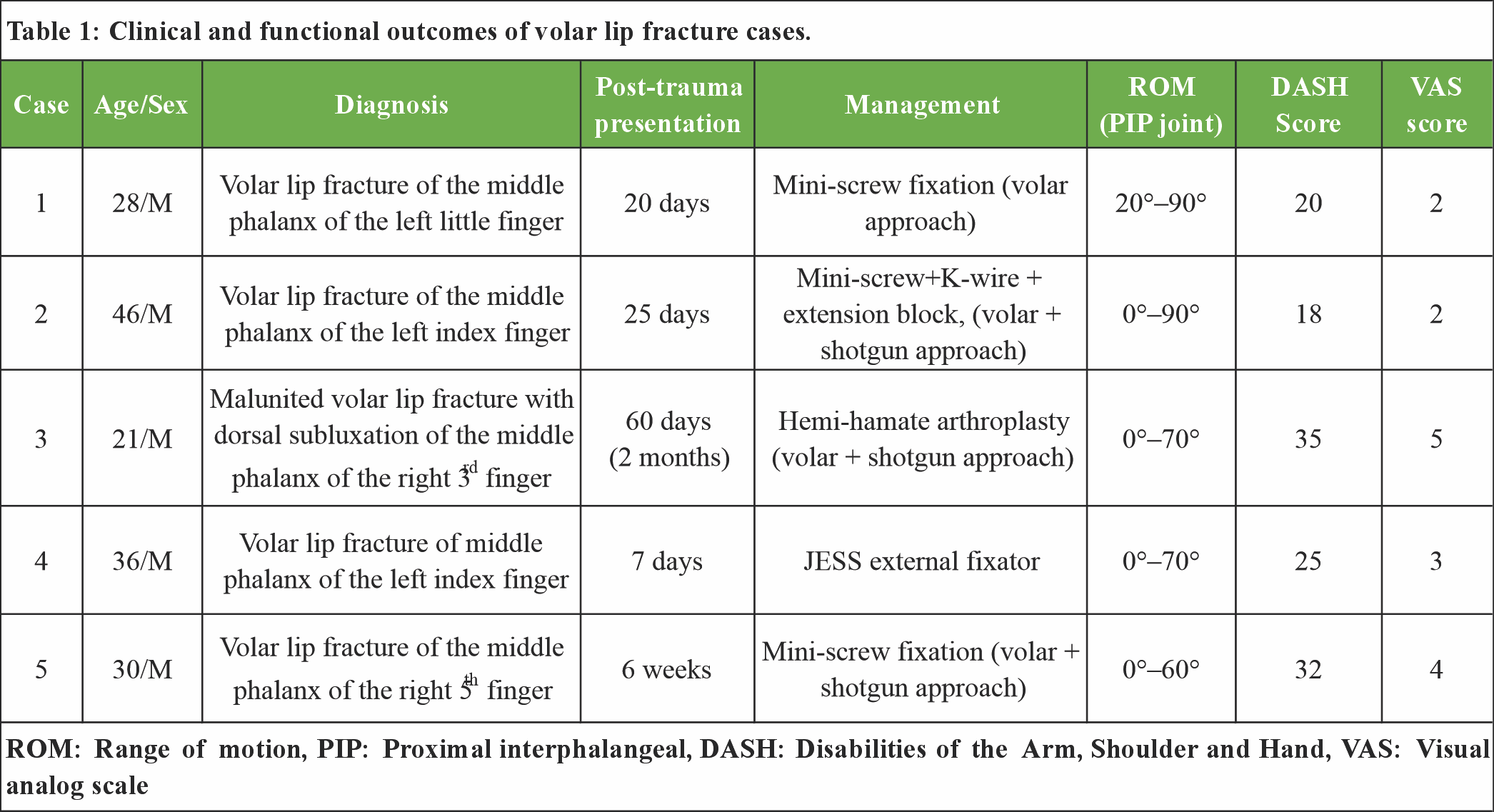
Table 1: Clinical and functional outcomes of volar lip fracture cases.
Acute cases demonstrated lower DASH scores ranging from 18 to 25, indicating good hand function, whereas chronic cases showed higher disability with DASH scores between 32 and 35. Acute cases reported lower VAS scores (2–3) at follow-up, whereas chronic cases had higher VAS scores (4–5), reflecting persistent pain and stiffness. Overall, acute management with early fixation resulted in superior functional outcomes (better ROM, lower DASH and VAS scores), while chronic or neglected fractures required salvage procedures with limited motion and higher residual disability.
These findings are consistent with established literature that links timing and fracture morphology to outcome. Kiefhaber and Stern emphasized that joint stability and the ability to restore articular congruity are central determinants of success in volar lip fracture–dislocations; fractures with articular depression, comminution, or inability to maintain reduction are more likely to have poor outcomes with conservative measures and frequently require operative management [4]. When the fracture geometry permits anatomic reduction and fixation, volar ORIF with mini-screws yields good functional recovery. Hamilton and colleagues and subsequent series reported favorable arcs of motion and functional results following mini-screw fixation for volar fragments, paralleling our acute-case outcomes, where the best ROM (up to 90°) was seen after early anatomic fixation [14]. For comminuted or chronic defects involving a substantial portion of the volar lip, hemi-hamate arthroplasty is well described as an effective reconstructive option. Williams initially popularized the procedure and reported good clinical and radiographic results; larger series and later reviews (McAuliffe et al.) have reinforced hemi-hamate as a reliable salvage/reconstructive technique when primary fixation is not feasible. In our chronic Case 3 (hemi-hamate), the final arc (0–70°) and higher DASH/VAS are comparable to ranges reported in those series, which typically document functional but not full restoration of motion [11]. Dynamic external fixation is valuable for unstable or highly comminuted injuries and when soft-tissue swelling precludes immediate ORIF; it provides stability while allowing early controlled motion and can improve outcomes in appropriately selected injuries. Our Case 4 treated with an external fixator achieved a modest ROM (0–70°), consistent with published experience that external fixation preserves joint motion better than prolonged immobilization but may not reproduce the ROM after anatomic ORIF [8].
Volar lip fractures of the middle phalanx represent a complex spectrum of intra-articular injuries that demand timely recognition and appropriate surgical planning. Our case series highlights that early intervention with stable fixation (mini-screw, K-wire, or external fixator) provides superior outcomes in terms of ROM, pain relief, and functional recovery compared to delayed or chronic presentations. Chronic or neglected fractures often necessitate salvage procedures such as hemi-hamate arthroplasty, which restore joint stability and function but with relatively limited motion and higher disability scores.
Early recognition and anatomical fixation of volar lip fractures of the middle phalanx yield superior functional outcomes. Delayed presentations often necessitate reconstructive procedures such as hemi-hamate arthroplasty, which can restore stability but are associated with restricted ROM and higher disability. Timely diagnosis and intervention remain the most important determinants of prognosis.
References
- 1. Wolfe, Pederson, Kozin, Cohen, Green’s Operative Hand Surgery. 8th ed. Netherlands: Elsevier; 2021 [Google Scholar] [PubMed]
- 2. Paul Tornetta, William M. Ricci, Robert F. Ostrum, Michael D. McKee, Benjamin J. Ollivere, Victor A. de Ridder Rockwood and Green’s Fractures in Adults. United States: Lippincott Williams and Wilkins; 2025. [Google Scholar] [PubMed]
- 3. Hastings H 2nd, Ernst JM. Dynamic external fixation for fractures of the proximal interphalangeal joint. Hand Clin 1993;9:659-74. [Google Scholar] [PubMed]
- 4. Kiefhaber TR, Stern PJ. Fracture dislocations of the proximal interphalangeal joint. J Hand Surg Am 1998;23:368-80. [Google Scholar] [PubMed]
- 5. Durham-Smith G, McCarten GM. Volar plate arthroplasty for closed proximal interphalangeal joint injuries. J Hand Surg Br 1992;17:422-8. [Google Scholar] [PubMed]
- 6. De Haseth KB, Neuhaus V, Mudgal CS. Dorsal fracture-dislocations of the proximal interphalangeal joint: Evaluation of closed reduction and percutaneous Kirschner wire pinning. Hand (N Y) 2015;10:88-93. [Google Scholar] [PubMed]
- 7. Pattni A, Jones M, Gujral S. Volar plate avulsion injury. Eplasty 2016;16:ic22. [Google Scholar] [PubMed]
- 8. Ellis SJ, Cheng R, Prokopis P, Chetboun A, Wolfe SW, Athanasian EA, et al. Treatment of proximal interphalangeal dorsal fracture-dislocation injuries with dynamic external fixation: A pins and rubber band system. J Hand Surg Am 2007;32:1242-50. [Google Scholar] [PubMed]
- 9. Kang R, Stern PJ. Fracture dislocations of the proximal interphalangeal joint. J Am Soc Surg Hand 2002;2:47-59. [Google Scholar] [PubMed]
- 10. Lee LS, Lee HM, Hou YT, Hung ST, Chen JK, Shih JT. Surgical outcome of volar plate arthroplasty of the proximal interphalangeal joint using the mitek micro GII suture anchor. J Trauma 2008;65:116-22. [Google Scholar] [PubMed]
- 11. Williams RM, Kiefhaber TR, Sommerkamp TG, Stern PJ. Treatment of unstable dorsal proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg Am 2003;28:856-65. [Google Scholar] [PubMed]
- 12. Ruland RT, Hogan CJ, Cannon DL, Slade JF. Use of dynamic distraction external fixation for unstable fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am 2008;33:19-25. [Google Scholar] [PubMed]
- 13. Smith SR, Sabet A, Gullborg EJ, Fernandez JJ, Cohen MS, Simcock XC, et al. Outcomes of hemi-hamate arthroplasty for proximal interphalangeal joint reconstruction. Hand (N Y) 2025;15589447251329581. [Google Scholar] [PubMed]
- 14. Hamilton SC, Stern PJ, Fassler PR, Kiefhaber TR. Mini-screw fixation for the treatment of proximal interphalangeal joint dorsal fracture-dislocations. J Hand Surg Am 2006;31:1349-54. [Google Scholar] [PubMed]