Fatty involution of simple bone cysts in the proximal humerus is a rare phenomenon that presents diagnostic challenges due to the lack of pathognomonic radiological features. When symptomatic, these lesions require surgical intervention, prioritizing symptomatology over imaging characteristics. Extended curettage combined with bio-absorbable antibiotic-loaded cement beads and autologous bone grafting provides excellent functional outcomes with complete lesion removal and structural reinforcement.
Dr. Silambarasi Nagasamy, Villa-A, Malleswari Villas, School Road, Panaiyur, Chennai - 600119, Tamil Nadu, India. E-mail: silambarasi.sn@gmail.com
Introduction: Intraosseous lipomas and simple bone cysts are mesenchymal bone tumors sharing similar characteristics and a suspected common pathophysiologic basis. Fatty involution of simple bone cysts is rare, especially in the proximal humerus. This report highlights a symptomatic case of fatty transformation in the proximal humerus, emphasizing diagnostic challenges and a novel surgical management approach.
Case Report: A 36-year-old male presented with progressive left shoulder pain. Imaging revealed a lytic lesion in the proximal humeral metaphysis. The patient underwent extended curettage, bioabsorbable antibiotic-loaded cement bead application, and autologous bone grafting. Histopathology confirmed fibroadipose tissue with fatty involution. The patient resumed daily activities within 2 weeks, showing significant improvement with disabilities of the arm, shoulder, and hand scores improving from 35 at 2 weeks to 5 at 4 weeks postoperatively.
Conclusion: Extended curettage with bio-absorbable antibiotic-loaded cement beads and autologous bone grafting is an effective option for managing symptomatic fatty involution in the proximal humerus. It provides complete lesion removal and structural reinforcement, offering excellent functional outcomes. Symptomatology should guide treatment decisions rather than imaging characteristics alone.
Keywords: Intraosseous lipoma, simple bone cyst, fatty involution, proximal humerus, extended curettage, bone grafting.
Although simple bone cysts and intraosseous lipomas have distinctly different names, they are both classified as mesenchymal tumors of the bone. As per the 2020 World Health Organization classification of bone tumors, a simple bone cyst is a cystic bone lesion lined by a fibrous membrane and filled with serous or serosanguinous fluid. On the other hand, an intraosseous lipoma is described as a benign neoplasm composed of white adipocytes. Despite their disparate nomenclature and description, intraosseous lipomas and simple bone cysts share a few similar characteristics. They commonly involve long tubular bones and radiologically present as lucent lesions of the bone [1]. The etiopathogenesis of both lesions remains unknown, but a shared pathophysiologic basis is suspected. Intraosseous lipomas have been suggested to arise as a result of adipocyte proliferation [2,3] and also as a result of spontaneous fatty involution of degenerating simple bone cysts [2,4,5]. However, all existing theories surrounding the origin of intraosseous lipomas are controversial and contradict each other. A few case reports have documented the progressive transformation of cystic lesions to fatty deposits. Malghem et al. reported a case of a calcaneal cyst whose fluid contents were progressively replaced by fat [6]. A similar transformation was also documented by Powell et al., wherein an intraosseous ganglion cyst demonstrated gradual deposition of intralesional fat [7]. Tins et al. suggested that calcaneal bone cysts spontaneously heal with fatty transformation of the cystic contents, and put forth the hypothesis that a proportion of intraosseous lipomas are healed simple bone cysts [4]. This limited literature precludes accurate assessment of the stage of transformation and even reliable differentiation between primary intraosseous lipomas and evolving bone cysts. Hence, there is a lack of standardized diagnostic and management protocols for such lesions. While intraosseous lipomas most commonly affect the calcaneum and proximal femur [6,8], involvement of the proximal humerus is rare, with fewer than a dozen cases reported in the literature [5,9,10]. Most reported cases are asymptomatic and managed conservatively, with limited documentation of functional outcomes in symptomatic patients. We present an uncommon case of fatty involution of a simple bone cyst in the proximal humerus, causing significant functional impairment, which was managed with extended curettage, bioabsorbable antibiotic-loaded cement beads, and autologous bone grafting. This case demonstrates excellent functional restoration following treatment and contributes to the sparse literature regarding surgical management of symptomatic proximal humeral intraosseous lipomas.
A 36-year-old male presented with a 6-month history of progressive left shoulder pain, which was exacerbated by activities and relieved only partially with medications. Plain radiographs of the left humerus showed an eccentrically-located lytic lesion within the proximal humeral metaphysis, in proximity to the greater tuberosity (Fig. 1). Computed tomography revealed a well-defined, peripherally enhancing cystic lesion with a homogenous soft tissue density matrix (Fig. 1).
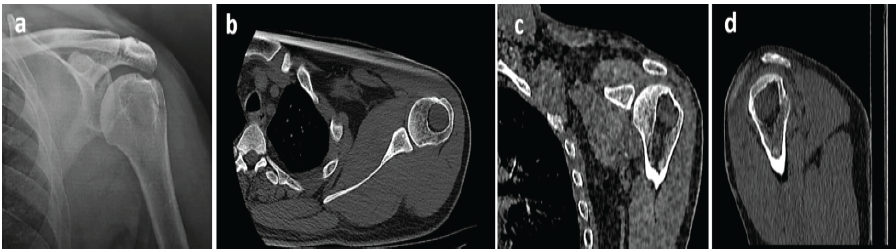
Figure 1: (a) Pre-operative radiograph demonstrating a lytic lesion in the proximal humerus, (b) axial, (c) coronal, and (d) sagittal computed tomography sections showing the lesion at its maximum diameter in each anatomical plane.
An excision biopsy followed by extended curettage was performed. A cortical window was created to gain access to the lesion, which was found to be filled with a yellow-colored mass (Fig. 2).
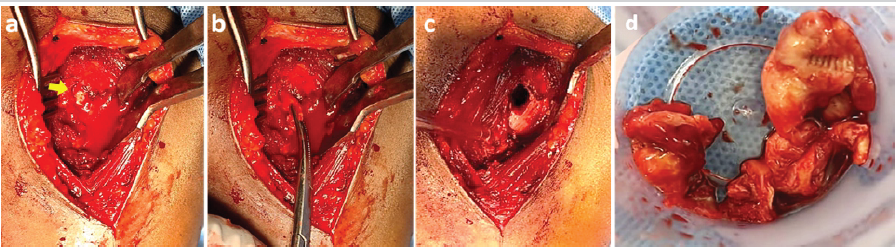
Figure 2: Intraoperative photographs demonstrating (a) fatty extrusion of the lesion through the proximal humerus, (b) extraction of the lesion, (c) the resultant cavity following its removal, and (d) the gross appearance of the excised lesion.
Contrast was injected to delineate the boundaries of the lesion, and the mass was excised in toto. Gross examination revealed a soft yellow mass with multiple septations enclosed within a thin capsule. Complete excision was confirmed using fluoroscopy. Extended curettage was performed using hydrogen peroxide. The resultant cavity was filled using bioabsorbable antibiotic-impregnated polymethylmethacrylate beads along with autologous bone graft harvested from the ipsilateral iliac crest (Fig. 3).
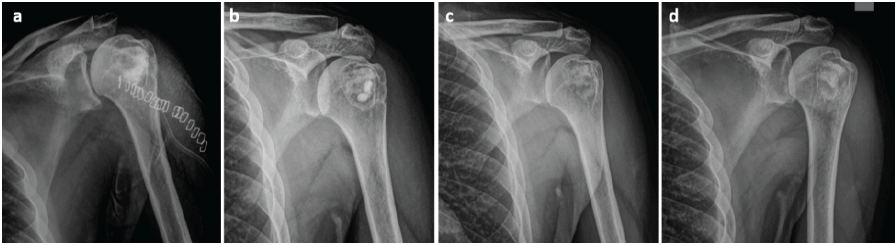
Figure 3: (a) Immediate post-operative radiograph following excision, curettage, and packing of the cavity with bone graft and antibiotic-loaded cement beads, (b) 3-month and (c) 5-month post-operative radiographs demonstrating progressive graft incorporation, and (d) 8-month post-operative radiograph showing complete graft incorporation and cavity consolidation.
Histopathologic analysis revealed the tissue to have fragments of fibroadipose tissue and fibrocollagenous cyst wall devoid of any lining. A focal collection of lymphocytes and pigment-laden macrophages was noted. Postoperatively, the patient reported a significant reduction in pain and was able to resume his activities of daily living by 2 weeks. Functional assessment using the disabilities of the arm, shoulder, and hand questionnaire [11], which evaluates upper extremity function through 30 items scored from 1 (no difficulty) to 5 (severe difficulty), demonstrated improvement from a score of 35 at 2 weeks postoperatively to 5 at 4 weeks, indicating substantial enhancement in functional capacity and quality of life.
This case represents an incidental discovery of fatty involution of a simple bone cyst of the proximal humerus, highlighting a diagnostic challenge that is often overlooked in clinical practice. The lesion, presumed to be a simple bone cyst, was found to be undergoing fatty transformation. Intraosseous lipomas typically present as well-defined, osteolytic lesions, and when high-grade, may demonstrate the “Cockade sign,” which is a nidus of calcification [12]. This insidious transformation from cystic to fatty tissue occurs without characteristic clinical or radiological markers, making early identification a challenge. This delayed recognition is compounded by the rarity of proximal humeral involvement, where the suspicion of such lesions is typically low. Kang et al. reported a collection of 21 cases from a single institute, wherein 20 cases were treated with curettage and bone grafting, and one with excision. It is also worth noting that only 11 of them were symptomatic pre-operatively, of which 4 had persistent pain [9]. Khal et al. managed a case of intraosseous lipoma of the calcaneum through curettage and bone cement application [12]. A collection of 5 cases was treated by Eyzaguirre et al. via curettage alone (4 cases) and excision alone (1 case) [13]. Surprisingly, studies by Campbell et al. [14] and Milgram [2], the largest collection of cases in literature to date, do not mention the modality of treatment. We took an offbeat approach by performing an extended curettage, combined with the application of bioabsorbable antibiotic-loaded cement beads and autologous bone grafting. This mode of intervention was necessitated by the symptomatic presentation and the need to address both the fatty tissue and the underlying structural compromise. The combination of extended curettage, antibiotic-loaded cement bead application, and autologous bone grafting represents a novel treatment approach that has not been reported previously for these lesions. This technique enabled complete excision of the lesion while simultaneously offering structural reinforcement that facilitated osseous healing and consolidation. This treatment consideration is frequently underemphasized when managing benign bone lesions, despite its critical importance in cases requiring extensive curettage. This case report highlights a diagnostic dilemma, as fatty transformation in bone cysts presents clinical as well as radiological challenges that are not well-established in current literature. Most often, these are incidental findings and are rarely symptomatic. Symptomatic lesions present a therapeutic paradox – while appearing benign on imaging, they may necessitate far more aggressive intervention than conventional wisdom suggests. The functional results obtained through extended curettage and comprehensive cavity management provide compelling evidence that surgical intervention should be prioritized in symptomatic patients. Symptomatology should serve as the primary driver for therapeutic decision-making rather than imaging characteristics that may be misleadingly reassuring.
This case report illustrates the rare phenomenon of symptomatic fatty involution of a simple bone cyst in the proximal humerus. Such cases pose a diagnostic challenge, especially due to the lack of pathognomonic radiological features. The combination of extended curettage, bioabsorbable antibiotic-loaded cement beads, and autologous bone grafting achieved excellent functional outcomes with complete resolution of pain. Treatment decisions for such lesions should be guided primarily by symptomatology rather than imaging characteristics, with surgical intervention prioritized in symptomatic patients to ensure complete removal of the lesion and to restore function.
Extended curettage with bioabsorbable antibiotic-loaded cement beads and autologous bone grafting is an effective treatment for symptomatic bone lesions in functionally critical sites and can offer complete resolution of pain. This case highlights the importance of symptom-driven treatment decisions and suggests the adoption of appropriate surgical techniques when managing symptomatic osseous lesions, regardless of their benign radiological appearance.
References
- 1. Anderson WJ, Doyle LA. Updates from the 2020 world health organization classification of soft tissue and bone tumours. Histopathology 2021;78:644-57. [Google Scholar] [PubMed]
- 2. Milgram JW. Intraosseous lipomas. A clinicopathologic study of 66 cases. Clin Orthop Relat Res 1988;231:277-302. [Google Scholar] [PubMed]
- 3. Hatori M, Hosaka M, Ehara S, Kokubun S. Imaging features of intraosseous lipomas of the calcaneus. Arch Orthop Trauma Surg 2001;121:429-32. [Google Scholar] [PubMed]
- 4. Tins BJ, Berkowitz YJ, Konala P, Davies M, Cassar-Pullicino VN, Lalam R, et al. Intraosseous lipomas originating from simple bone cysts. Skeletal Radiol 2021;50:801-6. [Google Scholar] [PubMed]
- 5. Wada R, Lambert RG. Deposition of intraosseous fat in a degenerating simple bone cyst. Skeletal Radiol 2005;34:415-8. [Google Scholar] [PubMed]
- 6. Malghem J, Lecouvet F, Omoumi P, Vande Berg B. Intraosseous lipomas originating from simple bone cysts. Skeletal Radiol 2021;50:2129. [Google Scholar] [PubMed]
- 7. Powell GM, Turner NS 3rd, Broski SM, Ringler MD, Howe BM. Intraosseous “Lipoma” of the calcaneus developing in an intraosseous ganglion cyst. J Radiol Case Rep 2018;12:16-24. [Google Scholar] [PubMed]
- 8. Sanae S, Ayman EF, Youssef O, Hounayda J, Rachida L, Ittimade N. Femoral intraosseous lipoma: Case report. Int J Case Rep Images 2021;12:1. [Google Scholar] [PubMed]
- 9. Kang HS, Kim T, Oh S, Park S, Chung SH. Intraosseous lipoma: 18 years of experience at a single institution. Clin Orthop Surg 2018;10:234-9. [Google Scholar] [PubMed]
- 10. Noble JS, Leeson MC. Intraosseous lipoma of the humerus. Orthopedics 1992;15:51-4. [Google Scholar] [PubMed]
- 11. Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: Longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord 2003;4:11. [Google Scholar] [PubMed]
- 12. Khal AA, Mihu RC, Schiau C, Fetica B, Tomoaia G, Luna MV. Symptomatic intraosseous lipoma of the calcaneum. Diagnostics (Basel) 2021;11:2243. [Google Scholar] [PubMed]
- 13. Eyzaguirre E, Liqiang W, Karla GM, Rajendra K, Alberto A, Gatalica Z. Intraosseous lipoma. A clinical, radiologic, and pathologic study of 5 cases. Ann Diagn Pathol 2007;11:320-5. [Google Scholar] [PubMed]
- 14. Campbell RS, Grainger AJ, Mangham DC, Beggs I, Teh J, Davies AM. Intraosseous lipoma: Report of 35 new cases and a review of the literature. Skeletal Radiol 2003;32:209-22. [Google Scholar] [PubMed]