[box type=”bio”] What to Learn from this Article?[/box]
The importance of seeking an irreducibility factor before the reduction.
Case Report | Volume 7 | Issue 1 | JOCR January – February 2017 | Page 58-60 | Mourad Zaraa, Ismail Jerbi, Sabri Mahjoub, Heithem Sehli, Mondher Mbarek. DOI: 10.13107/jocr.2250-0685.688
Authors: Mourad Zaraa[1], Ismail Jerbi[1], Sabri Mahjoub[1], Heithem Sehli[1], Mondher Mbarek[1]
[1] Department of Orthopedics, Trauma Center of Ben Arous, Ben Arous, Tunisia
Address of Correspondence
Dr. Mourad Zaraa,
Department of Orthopedics, Trauma Center of Ben Arous, Ben Arous, Tunisia.
E-mail: mourad.zaraa@hotmail.com
Abstract
Introduction: Subtalar dislocation is an uncommon lesion in traumatology chiefly when it concerns the lateral form. Surgical treatment is required when a fracture is related or the dislocation is irreducible. Even well treated, these dislocations progress unavoidably to subtalar arthrosis, which stays well tolerated.
Case Report: A 46-year-old male with irreducible lateral subtalar dislocation caused sustentaculum tali incarceration confirmed on computed tomography (CT). The patient underwent emergent open reduction and internal fixation; the sustentaculum tali was reduced and fixed with a compression screw. At 3 years, “American Orthopaedic Foot and Ankle Society Ankle-hindfoot” score was 86, and the functional result was considered excellent despite a Grade I subtalar osteoarthritis on the ankle X-ray.
Conclusion: An irreducible subtalar dislocation is exceptionally due to the incarceration of sustentaculum tali. CT is of great interest for good fracture analysis and management planning. Anatomical reduction of the articular surfaces, stable osteosynthesis, sufficient immobilization, and a well-conducted rehabilitation are the only guarantors of a good functional outcome.
Keywords: Ankle, dislocation, fracture, subtalar joint, surgical traumatology.
Introduction
Lateral subtalar dislocation is an uncommon lesion [1]. When present, it is usually an incomplete dislocation which interests the talocalcaneonavicular joint [2]. Generally, treatment consists of early reduction under adequate sedation. Open reduction is warranted in cases of soft-tissue interposition or locked dislocations. Even well treated, these dislocations progress unavoidably to subtalar arthrosis, which stays well tolerated [3]. We herein report the case of an irreducible dislocation of the talus in a 46-year-old male. We also review the literature for such cases.
Case Report
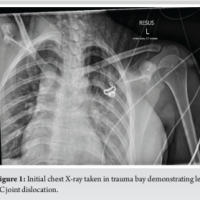
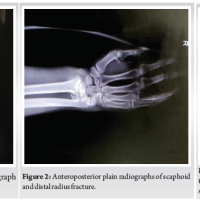
A 46-year-old male with no past medical history was a victim of a motor vehicle accident with a resultant trauma of the right ankle that was locked in equine. The first examination in the emergency department revealed a 3 cm wound under internal malleolus with jagged edges as well as a diffuse swelling of the foot and ankle. Vascular and neural examinations of the lower extremity were normal. Ankle X-ray showed a lateral subtalar dislocation with bony incarceration (Fig. 1). Computed tomography (CT) confirmed the subtalar dislocation with talonavicular subluxation and found that the bone fragment originates from the sustentaculum tali (Fig. 2).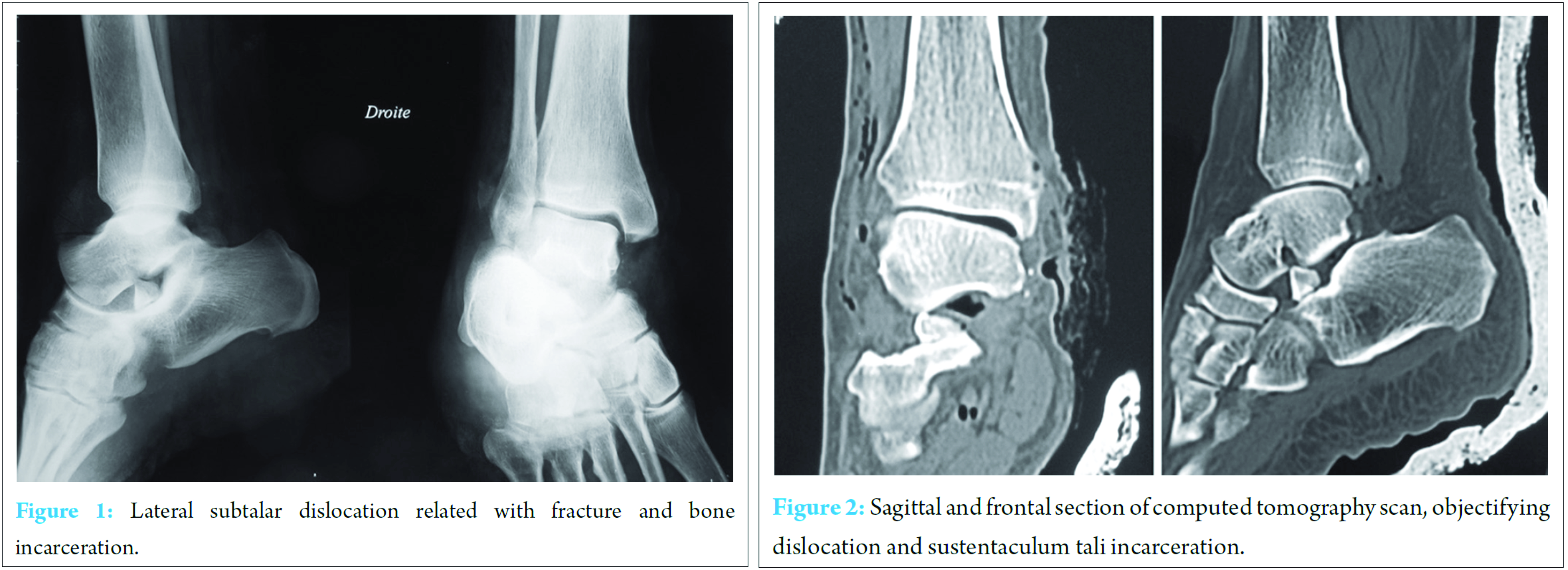
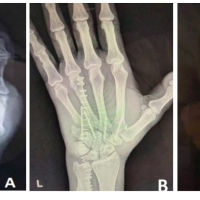
The patient underwent emergent open reduction and internal fixation. The sustentaculum tali fragment was resected allowing easy reduction of subtalar and talonavicular joints. Then, reduction and stabilization was made with pins bridging the talocalcaneal and talonavicular. Finally, the sustentaculum tali was reduced and fixed with a compression screw (Fig. 3). Finally, the patient was immobilized in a cast boot for 6 weeks. Moreover, it was put on antibiotics for 48 h. Fracture consolidation and skin healing were achieved at 6 week follow-up when the pins were removed. The patient’s painless full support was achieved at 8 weeks. At 3 years, “American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-hindfoot” score was 86, and the functional result was considered excellent despite a Grade I subtalar osteoarthritis on the ankle X-ray (Fig. 4).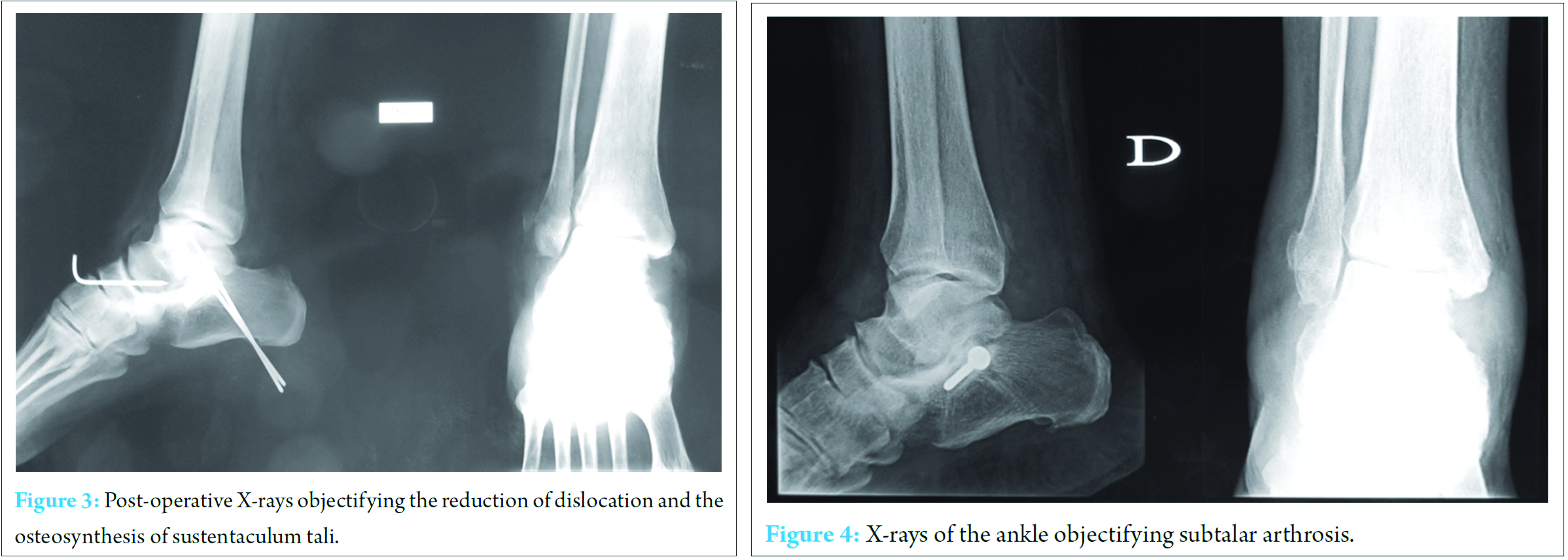
Discussion
Subtalar dislocations are rare traumatic injuries. In fact, they represent around 1% of all dislocations according to Perugia et al. [4]. Moreover, they occur frequently in young male after a high energy accident. Medial dislocations account for 80% of the cases [2, 5]. While lateral dislocations represent 20% of subtalar dislocations, 492 cases published between 1998 and 2012 [5]. Even though they are less frequent than medial dislocation, they give more osteoarthritis [6, 7, 8]. On the other hand, subtalar dislocations are often associated with articular fractures [9, 10, 11]. The sustentaculum tali fracture is a very rare injury that reflects the violence of the trauma. To the best of our knowledge, no such fracture was described with the association to subtalar dislocation [12]. Bibbo et al. [13] highlighted the importance of CT to better characterize these injuries. They found that this diagnostic modality gave new information about these injuries and changed the proposed treatment in 44% of the cases. The aim of treatment is to have mobile stable painless ankle. The reduction shall be made promptly to reduce the skin suffering. When articular fractures are associated, an open reduction generally allows anatomical reduction of the articular surfaces, the only guarantee of a good functional outcome [9]. This reduction is followed by an immobilization for 4-6 weeks in simple lesions and for 6-8 weeks in the case of osteoarticular lesions [14]. The rehabilitation will be undertaken soon after cast removal [14]. Lower AOFAS scores were observed on patients with associate peritalar osseous injuries [15], but in our case, the AOFAS score was 86. Necrosis is the most dreaded complication leading to subtalar osteoarthritis and generally occurs between the 2nd and 8th month. In fact, 3 cases of 8 subtalar dislocations (37.5%) developed osteonecrosis according to Foult et al. [9]. It seems to be related to a number of predisposing factors such as age, the association with bone or serious ligament injuries, the quality of the reduction, and the duration of immobilization [16]. Osteoarthritis of the subtalar joint is generally asymptomatic with little pain that is well tolerated. In a matter of fact, our case illustrates this radio-clinical discordance.
Conclusion
We report the case of an irreducible dislocation due to bony incarceration. CT is of great interest for good fracture analysis and management planning. Anatomical reduction of the articular surfaces, stable osteosynthesis, sufficient immobilization, and a well-conducted rehabilitation are the only guarantors of a good functional outcome.
Clinical Message
Irreducible subtalar dislocation imposes a CT scan exploration enabling accurate diagnosis and adequate treatment. Good functional outcome depends on the rapidity and quality of treatment.
References
1. Harris AP, Ramirez JM, Johnson J, Waryasz GR. Lateral subtalar fracture-dislocation with maintenance of the talonavicular joint: case study, diagnosis and management. Am J Emerg Med 2016;34(10):2055.e3-2055.e5.
2. Abu-Laban RB, Rose NG. Ankle and foot. Rosen’s emergency medicine – concepts and clinical practice. Elsevier 2014;58:723-750.
3. Schepers T, Backes M, Schep NW, Carel Goslings J, Luitse JS. Functional outcome following a locked fracture-dislocation of the calcaneus. Int Orthop 2013;37(9):1833-1838.
4. Perugia D, Basile A, Massoni C, Gumina S, Rossi F, Ferretti A. Conservative treatment of subtalar dislocations. Int Orthop 2002;26(1):56-60.
5. Hoexum F, Heetveld MJ. Subtalar dislocation: two cases requiring surgery and a literature review of the last 25 years. Arch Orthop Trauma Surg 2014;134(9):1237-1249.
6. Garofalo R, Moretti B, Ortolano V, Cariola P, Solarino G, Wettstein M, et al. Peritalar dislocations: a retrospective study of 18 cases. J Foot Ankle Surg 2004;43(3):166-172.
7. Wagner R, Blattert TR, Weckbach A. Talar dislocations. Injury 2004;35 Suppl 2:SB36-SB45.
8. de Palma L, Santucci A, Marinelli M, Borgogno E, Catalani A. Clinical outcome of closed isolated subtalar dislocations. Arch Orthop Trauma Surg 2008;128(6):593-598.
9. Foult H, Bricout J, Favart L, Burdin P. Dislocations: A review of 10 cases with a 2 to 14 year follow-upSubtalar dislocations: A review of 10 cases with a 2 to 14 years follow-up. Ann Orthop Ouest 1992;2:87-90.
10. Nepple JJ, Putnam RM, Gardner MJ, Bartlett CS 3rd, Johnson JE. Calcaneal fracture-dislocation with fracture of the sustentaculum and lateral column: A unique injury pattern. Foot Ankle Int 2013;34(2):290-294.
11. Jungbluth P, Wild M, Hakimi M, Gehrmann S, Djurisic M, Windolf J, et al. Isolated subtalar dislocation. J Bone Joint Surg Am 2010;92(4):890-894.
12. Della Rocca GJ, Nork SE, Barei DP, Taitsman LA, Benirschke SK. Fractures of the sustentaculum tali: injury characteristics and surgical technique for reduction. Foot Ankle Int 2009;30(11):1037-1041.
13. Bibbo C, Lin SS, Abidi N, Berberian W, Grossman M, Gebauer G, et al. Missed and associated injuries after subtalar dislocation: the role of CT. Foot Ankle Int 2001;22(4):324-328.
14. Lasanianos NG, Lyras DN, Mouzopoulos G, Tsutseos N, Garnavos C. Early mobilization after uncomplicated medial subtalar dislocation provides successful functional results. J Orthop Traumatol 2011;12(1):37-43.
15. Camarda L, Abruzzese A, Gattuta AL, Lentini R, D’Arienzo M. Results of closed subtalar dislocations. Musculoskeletal surg 2016;100(1):63-69.
16. Tucker DJ, Burian G, Boylan JP. Lateral subtalar dislocation: review of the literature and case presentation. J Foot Ankle Surg 1998;37(3):239-247.
| How to Cite This Article: Zaraa M, Jerbi I, Mahjoub S, Sehli H, Mbarek M. Irreducible Subtalar Dislocation Caused by Sustentaculum Tali Incarceration. Journal of Orthopaedic Case Reports 2017 Jan-Feb;7(1): 58-60. Available from: https://www.jocr.co.in/wp/wp-content/uploads/18.-2250-0685.688.pdf |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com