Anterior extrapharyngeal distraction and fixation of atlas and axis with the new implant is a simple, safe and biomechanically appealing technique.
Dr. Sushil V Patkar,
Department of Neurosurgery, Poona Hospital and Research Center, Pune, Maharashtra, India.
E-mail: patneurosurgeon@gmail.com
Introduction: Anterior retropharyngeal realignment, distraction, and atlantoaxial fixation are an option for the treatment of symptomatic basilar invagination (BI). The anterior implants for distraction and fixation for atlantoaxial joints are still evolving. We share our experience using a novel implant which can easily, safely, and rigidly fix both lateral masses to the body of the axis.
Methods: After exposing both the atlantoaxial joints anteriorly, the joints were prepared, distracted with wedge shaped autologous tricorticate bone grafts and realigned to correct the cervicomedullary strain. The atlantoaxial joints were fixed using a novel titanium plate by passing screws upwards and laterally into the lateral masses of the atlas and centrally into the body of the axis. Post-operative imaging showed effective correction of BI and atlantoaxial dislocation. Post-operative dynamic X-ray images confirmed maintenance of rigid fixation at 6 months. Conclusion: This new plate screw construct is safe, easy, cost-efficient, and biomechanically appealing option for the treatment of symptomatic BI.
Keywords: Basilar invagination, atlantoaxial dislocation, vertebral artery injury, atlantoaxial fixation, atlantoaxial instability.
Realignment of atlantoaxial facets along with distraction using bone grafts and cages followed by fixation is a standard surgical option for symptomatic basilar invagination (BI). We present the case of a 45-year-old male patient who presented with quadriparesis following a trivial fall. He underwent anterior surgery for distraction, bone grafting, and realignment of facets followed by fixation using a novel customized implant. Post-operative imaging showed satisfactory outcome and stable fixation at 6 months. Magnetic resonance imaging demonstrated BI with atlantoaxial dislocation and pinching of the cervicomedullary junction of the neuroaxis with signal change within the medulla and upper cord. Computerized axial tomography (CT) with dynamic study confirmed significant BI with atlantoaxial dislocation (AAD). The atlas was occipitalized with the enlarged lateral masses overhanging and tilting over the anterior edge of the malformed superior facets of the axis resulting in posterior opening of the atlantoaxial joints and resultant AAD with BI. The Grabb-Oakes index was 11.7 mm. The posterior lip of the occiput with the fused atlas was hypertrophied and impinged into the foramen magnum. The spinous process and laminae of the axis were hypertrophied. CT angiography showed a hypo plastic left vertebral artery and large right vertebral with an abnormal course dorsally over the pars of the axis. Lateral X-ray of the craniovertebral junction in extension showed the angle of the mandible at the level of the C2-3 disc (Fig. 1).
The surgical technique described earlier was used to expose the atlantoaxial region, retropharyngeal, from the right side [1]. Both the atlantoaxial joints and the anterior surfaces of the lateral masses of the atlas were exposed after dividing the medial halves of the hypertrophied longus coli and rectus capitis muscles bilaterally. The soft pannus between the anterior arch of the atlas and odontoid was excised. The anterior joint capsules were excised widely and overhanging anterior-inferior edge of the lateral masses of the atlas was reshaped with 3 mm microdrill till they were flush with the superior facet of the axis. All these maneuvers resulted in increased mobility of the atlantoaxial complex permitting skull tong assisted distraction and realignment in extension. The opposing joint surfaces were curetted and abraded till blood oozed from the both the opposing joint surfaces (gardening). Tricorticate bone grafts measuring 7 mm thickness anteriorly and 4 mm posteriorly were harvested from the right iliac crest, and using the skull tongs for distraction, the “wedge” grafts were impacted into the joints bilaterally till they had countersunk beyond the anterior edge of the joint space.
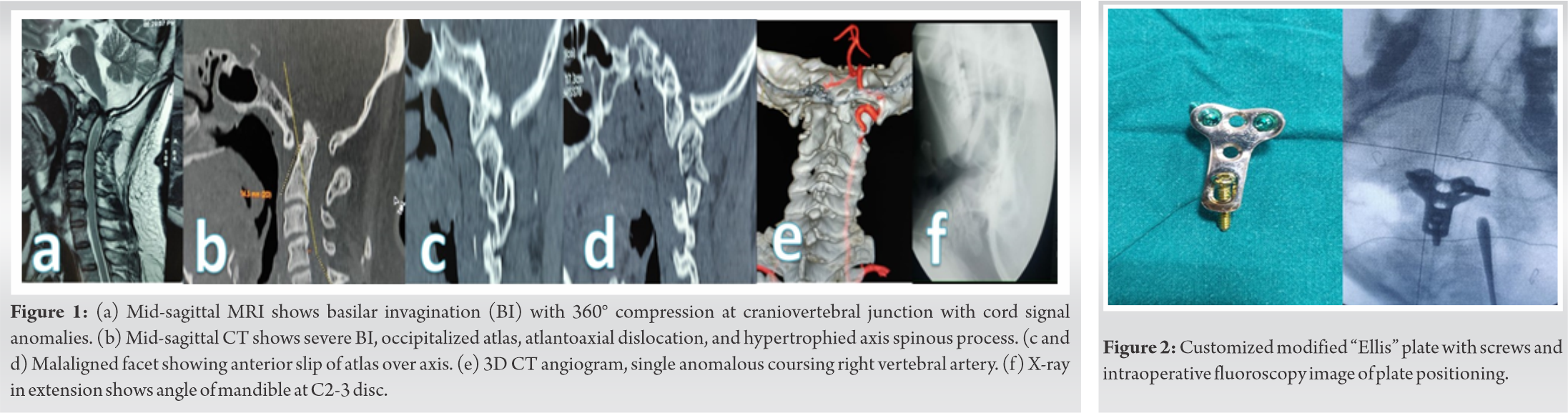
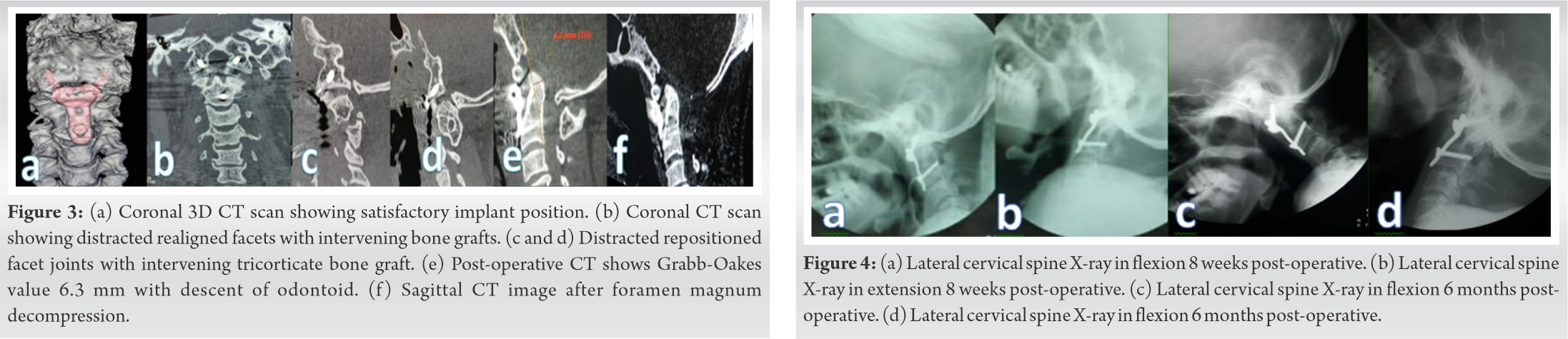
A customized “T”-shaped medical grade titanium plate (3.5 mm thickness) manufactured by Bombay Orthopaedics Company (Rajkot, Gujarat, India), was contoured, and placed over the region so that the upper outer screws could be passed upward and outward onto the lateral masses and the stem of the plate sat snugly on the anterior surface of the axis (Fig. 2). Using a 3 mm microdrill bit screw holes were marked, holding the plate in position, for both lateral masses just above the medial half of the anterior-inferior edge and directed upward and laterally toward the upper lateral posterior end of the lateral mass under lateral fluoroscopy, and the axis in midline just above the C2-3-disc space under anterior-posterior fluoroscopy. Plate was first fixed to the axis with a self-drilling cortical-cancellous screw (4 mm thickness, 22 mm length) through the previously marked drill hole to achieve bicortical purchase, length calculated on CT console preoperatively, and last few mms tightened under lateral fluoroscopic guidance. Lateral masses were fixed with cortical screws (3.5 mm thickness and 18 mm length) passed through the previously drilled holes after tapping. As the posterior lip of foramen magnum was also impinging on the cervicomedullary region, the patient underwent posterior foramen magnum decompression after 5 days. Post-operative CT scan imaging showed improved Grabb-Oakes index of 6.3 mm and remarkable descent of the odontoid. The atlantoaxial joints had realigned with intervening countersunk bone grafts and satisfactory position of plate and screws and favorable Grabb-Oakes measurement (Fig. 3). He has shown marginal clinical improvement and is undergoing rehabilitation. Dynamic X-rays at 8 weeks and 6 months show sustained rigid fixation (Fig. 4).
The weight of the cranium is transmitted from the occipital condyles on lateral masses of the atlas to the superior facets of axis which distributes, most weight to the body of the axis and some to the posterior elements through the pars of the axis to the facet joints of C2-C3 [2,3]. The Grabb-Oakes index has become an accepted criteria to decide the extent of ventral cervicomedullary strain and surgical treatment should aim at reducing it below 9 mm [4]. Facet distraction for BI has reduced the need for odontoidectomy [5,6]. Abnormal atlantoaxial facetal anatomical relationship in sagittal and coronal planes decides the BI severity and treatment is directed toward realignment restoration of a normal facetal relationship followed by fixation and ultimately fusion of the realigned atlantoaxial joints [7,8,9]. Technical descriptions of posterior approach suggest interfacet bone pieces or flat cages (parallel surfaces) which result in distraction in the slipped position and will not be in compression mode (with floating cage or bone grafts), once atlas and axis are repositioned for fixation, as the joint will open up anteriorly. However, parallel surface cages are still used because wedge-shaped cages cannot be passed from behind into joints which are inclined anteriorly and inferiorly. Lordotic wedge cages and anterior approach are biomechanically important in correcting deformity, enhancing fusion, and restoring the sagittal spinal balance [10,11]. The posterior tension band, the muscles, and the fulcrum (axis spinous process) play an important role in limiting the anterior and inferior slip of the atlas over the axis which is supported by the fact that in most cases of congenital BI there is associated hypertrophy of the axis laminae and spinous process. Posterior atlantoaxial fixation surgery has a small but definite risk of vertebral artery injury and literature is studded with descriptions of ways to prevent and treat this devastating complication [12,13,14,15,16]. Posterior approach in spinal surgery disrupts the posterior tension band and the extensively detached muscles always heal with a scar. In addition, the intervening screw plate or rod implants prevent their reattachment to the skull and posterior elements of the atlantoaxial bones [17]. In appropriately selected cases (angle of the mandible is at or above the C2-3 disc in lateral X-ray in extension), the atlantoaxial joints can easily and safely be approached anteriorly in supine position by a unilateral submandibular retropharyngeal approach as described earlier [18,19,20]. This approach permits wide unhindered and safe exposure of both atlantoaxial joints for joint surface, minimal division of the anterior muscles, ligament, and joint capsule creates additional instability which is important to correct the deformity. Preparation of the joint surfaces and tricorticate “wedge” autografting in compression mode is the primal step to realign the joints and finally achieve solid bone fusion along the line of weight transmission [21]. Transoral anterior atlantoaxial joint fixation with plates and screws across each joint as described earlier can be simplified and strengthened using a single plate fixed across both joints by the retropharyngeal approach avoiding the risk of infection [22]. The body of the axis offers a large volume of bone stock and the ability to get bicortical screw hold with a larger diameter screw further enhances the fixation. This new plate screw construct is safe, easy, inexpensive, and biomechanically appealing. More cases and longer follow-up are necessary before it becomes a universal option.
Anterior submandibular extrapharyngeal approach to treat atlantoaxial instability and deformity is simple safe and biomechanically superior. This new plate screw construct is easy to perform, cost-efficient, and biomechanically appealing option for the treatment of symptomatic BI.
Symptomatic BI needs surgery. The Grabb-Oakes index is useful to assess the extent of cervicomedullary strain. Posterior distraction of the atlantoaxial joints with fixation of the atlantoaxial joints has become the standard of care for the treatment of BI. Anterior surgery and fixation with the new plate screw construct can achieve all the goals more easily and safely.
References
- 1.Patkar S. Anterior extra pharyngeal approach and fixation of the atlanto-axial joint with screw plate construct or anterior transarticular screws: And review of literature. Spinal Surg 2013;27:230-7. [Google Scholar | PubMed]
- 2.Pal GP, Routal RV. A study of weight transmission through the cervical and upper thoracic regions of the vertebral column in man. J Anat 1986;148:245-61. [Google Scholar | PubMed]
- 3.Menon VK. Mechanically relevant anatomy of the axis vertebra and its relation to hangman’s fracture: An illustrated essay. Neurospine 2019;16:223-30. [Google Scholar | PubMed]
- 4.Grabb PA, Mapstone TB, Oakes WJ. Ventral brain stem compression in pediatric and young adult patients with Chiari I malformations. Neurosurgery 1999;44:520-7; discussion 527-8. [Google Scholar | PubMed]
- 5.Goel A, Bhatjiwale M, Desai K. Basilar invagination: A study based on 190 surgically treated patients. J Neurosurg 1998;88:962-8. [Google Scholar | PubMed]
- 6.Goel A, Shah A. Atlantoaxial joint distraction as a treatment for basilar invagination: A report of an experience with 11 cases. Neurol India 2008;56:144-50. [Google Scholar | PubMed]
- 7.Chandra PS, Goyal N. The severity of basilar invagination and atlantoaxial dislocation correlates with sagittal joint inclination, coronal joint inclination, and craniocervical tilt: A description of new indices for the craniovertebral junction. Neurosurgery 2014;76:E235-9. [Google Scholar | PubMed]
- 8.Chandra PS, Prabhu M, Goyal N, Garg A, Chauhan A, Sharma BS, et al. Distraction, compression, extension, and reduction combined with joint remodeling and extra-articular distraction: Description of 2 new modifications for its application in basilar invagination and atlantoaxial dislocation: Prospective study in 79 cases. Neurosurgery 2015;77:67-80; discussion 80. [Google Scholar | PubMed]
- 9.Patkar S. Anterior facetal realignment and distraction for atlanto-axial subluxation with basilar invagination a technical note. Neurol Res 2016;38:748-50. [Google Scholar | PubMed]
- 10.Lewandrowski KU, Ransom NA, León JF, Anthony Yeung A. The concept for A standalone lordotic endoscopic wedge lumbar interbody fusion: The LEW-LIF. Neurospine 2019;16:82-95. [Google Scholar | PubMed]
- 11.Kapustka B, Kiwic G, Chodakowski P, Miodoński JP, Wysokiński T, Łączyński M, et al. Anterior lumbar interbody fusion (ALIF): Biometrical results and own experiences. Neurosurg Rev 2020;43:687-93. [Google Scholar | PubMed]
- 12.Hsu WK, Kannan A, Mai HT, Fehlings MG, Smith ZA, Traynelis VC, et al. Epidemiology and outcomes of vertebral artery injury in 16 582 cervical spine surgery patients: An AOSpine North America multicenter study. Global Spine J 2017;7 Suppl 1:21S-7S. [Google Scholar | PubMed]
- 13.Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: Case series and technical note. J Spinal Disord Tech 2004;17:158-62. [Google Scholar | PubMed]
- 14.Lang Z, Tian W, Liu B, Yuan Q, He D, Wang YQ, et al. Posterior C1-C2 transarticular screw fixation for atlantoaxial instability assisted by intraoperative 3-dimensional fluoroscopy-based navigation. Zhonghua Yi Xue Za Zhi 2013;93:2296-300. [Google Scholar | PubMed]
- 15.Tian W, Liu YJ, Liu B, He D, Wu JY, Han XG, et al. Guideline for posterior atlantoaxial internal fixation assisted by orthopaedic surgical robot. Orthop Surg 2019;11:160-6. [Google Scholar | PubMed]
- 16.Patkar S. Posterior atlantoaxial fixation with new subfacetal axis screw trajectory avoiding vertebral artery with customized variable screw placement plate and screws to enhance biomechanics of fixation. Neurosurg Focus Video 2020;3:V10. [Google Scholar | PubMed]
- 17.Pourtaheri S, Issa K, Lord E, Ajiboye R, Drysch A, Hwang K, et al. Paraspinal muscle atrophy after lumbar spine surgery. Orthopedics 2016;39:e209-14. [Google Scholar | PubMed]
- 18.Koller H, Kammermeier V, Ulbricht D, Assuncao A, Karolus S, van den Berg B, et al. Anterior retropharyngeal fixation C1-2 for stabilization of atlantoaxial instabilities: Study of feasibility, technical description and preliminary results. Eur Spine J 2006;15:1326-38. [Google Scholar | PubMed]
- 19.Patkar S. Anterior retropharyngeal cage distraction and fixation for basilar invagination: “The wedge technique”. Neurospine 2019;16:286-92. [Google Scholar | PubMed]
- 20.Patkar S. Anterior retropharyngeal cage distraction with atlantoaxial plate-screw fixation for basilar invagination with atlantoaxial dislocation. Neurosurg Focus Video 2020;3:V11. [Google Scholar | PubMed]
- 21.Kowalski RJ, Ferrara LA, Benzel EC. Biomechanics of bone fusion. Neurosurg Focus 2001;10:E2. [Google Scholar | PubMed]
- 22.Zhang B, Liu H, Cai X, Wang Z, Xu F, Liu X, et al. Biomechanical comparison of modified TARP technique versus modified goel technique for the treatment of basilar invagination: A finite element analysis. Spine (Phila Pa 1976) 2016;41:E459-66. [Google Scholar | PubMed]