Thorough arthroscopic evaluation can help diagnose a rare case of ochronotic arthropathy and alleviate symptoms, further avoiding or delaying the need of arthroplasty.
Dr. Amyn M. Rajani,
Department of Orthopedic,
Orthopedic Arthroscopy Knee and Shoulder Clinic, 707,
Panchashil Plaza, Hughes Road, Mumbai – 400 007, Maharashtra, India.
E-mail: dramrajani@gmail.com
Introduction : Ochronotic arthropathy in patients with alkaptonuria is a rare hereditary disorder. The altered metabolism causes the homogentesic acid derivatives to deposit in various connective tissues causing characteristic pigmentation. Due to the close clinical resemblance to that of a degenerative disorder, diagnosis of ochronotic arthropathy usually occurs intraoperatively. We report arthroscopic findings of a 50-year-old female with ochronotic arthropathy.
Methods : A 50-year-old woman came with complaints of pain and swelling in the left knee. Clinical examination and MRI findings were correlated to reveal a tear of lateral meniscus. On arthroscopic examination, the blackish pigmentation of the meniscus and the articular cartilage led to the diagnosis of ochronotic arthropathy.
Conclusion : Arthroscopy plays an important role in diagnosis and treatment of patients with ochronotic arthropathy. The characteristic arthroscopic finding may aid diagnosis even in patients who do not have other systemic manifestations. Timely arthroscopic intervention can help delay the disease progression.
Keywords : Alkaptonuria, Ochronotic arthropathy, Ochronosis, Arthroscopy.
Alkaptonuria is a rare metabolic disorder usually with an autosomal recessive trait. There is altered metabolism of phenylalanine and tyrosine amino acids due to deficiency of homogentisic acid oxidase (HAO) [1]. This causes excessive accumulation of homogentisic acid which further oxidises to form benzoquinone acetic acid (BQA). The characteristic bluish-black pigmentation called “ochronosis” of various connective tissues is due to these deposits of HAO and BQA [2]. Due to high affinity for fibrillary collagen, this pigment affects the hyaline cartilage of the larger peripheral joints. This results in decreased cross-linkage of collagen, thereby making it more susceptible to mechanical stress [3]. This causes the cartilage to become brittle, fragmented which loads the subchondral bone leading to inflamed synovium thereby resulting in “ochronotic arthropathy” [4].
Patients are usually asymptomatic till the fourth decade of life after which there is clinical presentation of ochronotic arthropathy [5]. Clinically, there is degenerative arthropathy of spine and the larger joints, lower limb being more common. The diagnosis is confirmed with histopathologic examination of tissue biopsies and assessment of homogentisic acid in the urine [6].
A 50-year-old woman presented to us with a torn lateral meniscus. On arthroscopic examination, we found brownish-black pigmentation of the menisci and articular cartilage. With the suspect of alkaptonuria, further laboratory examinations of the urine sample and histopathologic examination of tissue biopsies were conducted which confirmed the diagnosis.
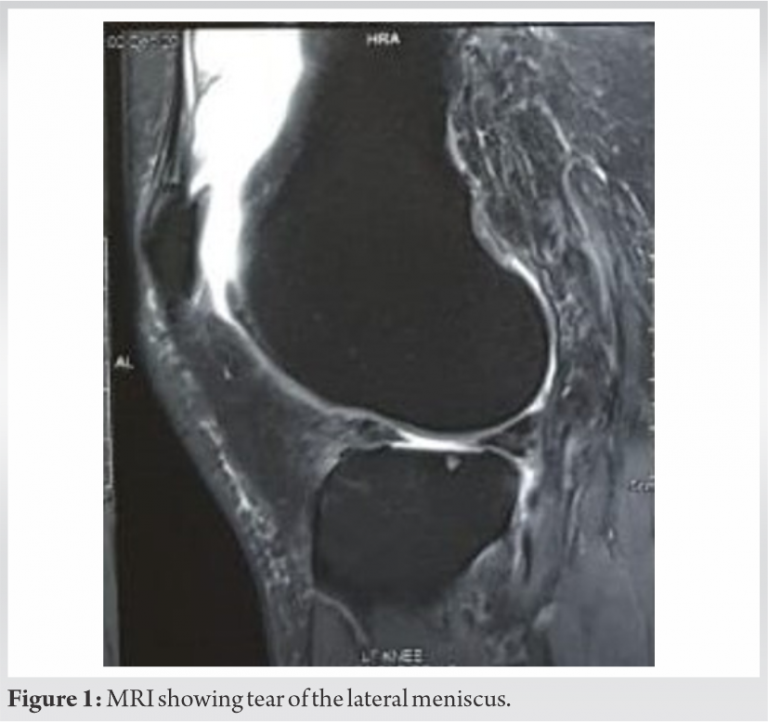
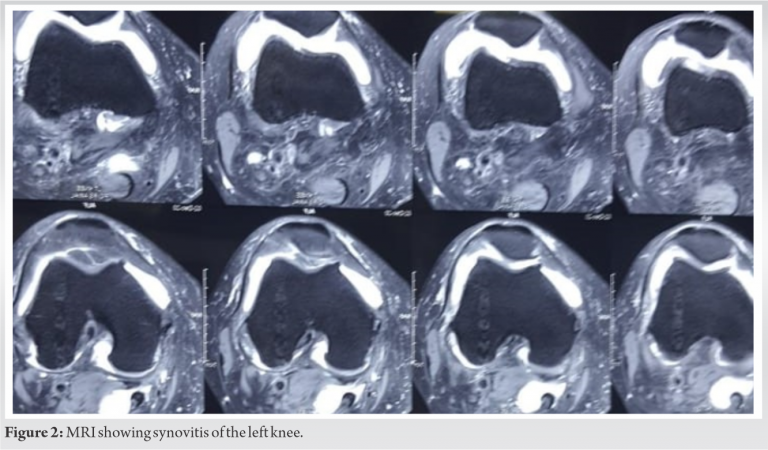
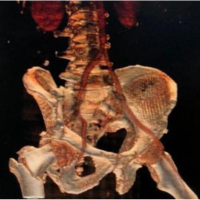
A 50-year-old woman came with chief complaints of pain and swelling in the left knee. She had a recent history of twisting injury while walking. Physical examination revealed tenderness along the lateral joint line and McMurray’s test was positive for lateral meniscus. Flexion was terminally restricted and painful. Radiographs showed evidence of lateral compartment osteoarthritic changes. Tear of lateral meniscus (Fig. 1) along with synovitis (Fig. 2) and degenerative changes in the cartilage were evident on magnetic resonance imaging (MRI) of the left knee. Arthroscopic partial meniscectomy was planned on the basis of her clinical and radiological presentation.
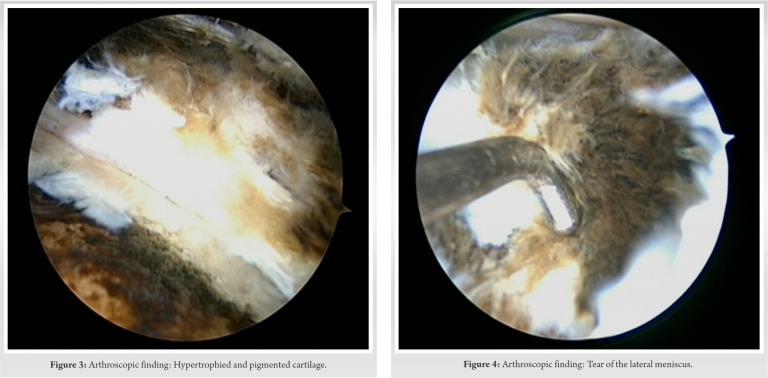
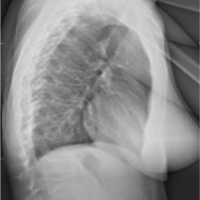
Arthroscopic findings revealed hypertrophied and pigmented synovium (Fig. 3). There were small chondral defects of size 3 mm to 5 mm, Grade 2+ more over the lateral condyle than the medial condyle. There were pigmented loose bodies with size varying from 0.5 mm to 5 mm. Grade 3 changes were observed in the cartilage with kissing lesions and greyish-blackish discoloration. Both the menisci were discolored with tear in the lateral meniscus (Fig. 4). Although the integrity of all the ligaments was maintained, there was evident discoloration and thinning out.
Partial lateral meniscectomy was performed with removal of loose bodies. Arthroscopic debridement was done to remove the hypertrophied synovium and specimen was sent for histopathological examination. With the suspect of ochronotic arthropathy due to the discoloration observed in arthroscopic intervention, further examination and investigation were planned.
Urine was normal in color but turned dark brown when tested with sodium hydroxide (NaOH). Urine showed high levels of HGA. Histopathological reports revealed brownish pigmentation along with degenerative changes. Detailed examination of the skin, sclera, eye, and ear showed no abnormalities.
Patient achieved immediate pain relief after the arthroscopic intervention. Postoperatively, physical therapy rehabilitation program, emphasizing on full weight- bearing walking, was started along with achieving pain-free range of motion followed by strength training. Patient had no complaints in the subsequent follow-ups at week 2, week 4, and week 8.
Ochronotic arthropathy is a rare disorder found in patients with alkaptonuria. Alkaptonuria is a metabolic disease which occurs in about 1 per billion births [7]. Albert and Zdareck studied the association between alkaptonuria and ochronosis in 1902 [8]. Few case reports of arthroscopic diagnosis and management of ochronosis have been reported. At present, no cure has been found for ochronosis or alkaptonuria. The rare prevalence of the disease makes it difficult to form a consensus on surgical treatment options.
The literature highlights the arthroscopic findings of ochronosis observed in knee and some in hip and shoulder [9, 10, 11]. The arthroscopic findings studied in this case report were consistent with the other cases documented. Case reported by Thacker et al. [11] described the arthroscopic findings in a 40-year-old male with multiple joint involvements. The findings revealed pigmented hypertrophic synovium with loose bodies in the knee joint and frying of rotator cuff along with hypertrophic synovium in the shoulder joint. The patient did exhibit greyish-blackish discoloration on the surface, unlike in our case, where there was no obvious finding on the surface. The findings of pigmented hypertrophic synovium with loose bodies and lack of involvement of ligamentous structures, though less pliable than normal, were similar in our case. The involvement of the lateral meniscus in our case was consistent with the findings reported by Chen et al. [9], Kural et al. [12], and Raaijmaaker et al. [13] where the patient had degenerative tear of menisci for which partial meniscectomy was performed. Generalized cartilage degeneration found in our case has also been reported consistently in the literature.
Arthroscopy in ochronotic arthropathy is recommended for diagnostic and therapeutic purpose. It helps to reduce pain and swelling and also improves range of motion. Removal of loose bodies and debridement of the frayed tissue can further reduce the insult to the articular cartilage. This helps in slowing down the rate of cartilage degradation, thereby delaying the need for arthroplasty. Therapeutic arthroscopy can thus provide immediate symptomatic relief and help impede the disease progression.
Arthroscopy as diagnostic and therapeutic tool plays an important role in the management of patients with ochronosis. The characteristic findings in this case report may help in diagnosis of ochronotic arthropathy without other systemic presentation. Arthroscopy can provide excellent symptomatic relief and avoid or delay the need for arthroplasty.
Arthroscopy plays a vital role in diagnosis of ochronotic arthropathy as radiological findings including MRI may mimic degenerative or other traumatic conditions.
References
- 1.Mistry JB, Bukhari M, Taylor AM. Alkaptonuria. Rare Dis 2013;1:e27475. [Google Scholar | PubMed]
- 2.Phornphutkul C, Introne WJ, Perry MB, Bernardini I, Murphey MD, Fitzpatrick DL, et al. Natural history of alkaptonuria. N Engl J Med 2002;347:2111-21. [Google Scholar | PubMed]
- 3.Taylor AM, Boyde A, Wilson PJ, Jarvis JC, Davidson JS, Hunt JA, et al. The role of calcified cartilage and subchondral bone in the initiation and progression of ochronotic arthropathy in alkaptonuria. Arthritis Rheum 2011;63:3887-96. [Google Scholar | PubMed]
- 4.Hamdi N, Cooke TD, Hassan B. Ochronotic arthropathy: Case report and review of the literature. Int Orthop 1999;23:122-5. [Google Scholar | PubMed]
- 5.Cetinus E, Cever I, Kural C, Ertürk H, Akyıldız M. Ochronotic arthritis: Case reports and review of the literature. Rheumatol Int 2005;25:465-8. [Google Scholar | PubMed]
- 6.Millea TP, Segal LS, Liss RG, Stauffer ES. Spine fracture in ochronosis. Report of a case. Clin Orthop Relat Res 1992;281:208-11. [Google Scholar | PubMed]
- 7.Garrod AE. The incidence of alkaptonuria: A study in chemical individuality. 1902. Mol Med 1996;2:274-82. [Google Scholar | PubMed]
- 8.Zatkova A. An update on molecular genetics of Alkaptonuria (AKU). J Inherit Metab Dis 2011;34:1127-36. [Google Scholar | PubMed]
- 9.Chen AL, Rose DJ, Desai P. Arthroscopic diagnosis and management of ochronotic arthropathy of the knee. Arthroscopy 2001;17:869-73. [Google Scholar | PubMed]
- 10.Dom K, Pittevils T. Ochronotic arthropathy: The black hip. Case report and review of the literature. Acta Orthop Belg 1997;63:122-5. [Google Scholar | PubMed]
- 11.Thacker M, Garude S, Puri A. Ochronotic arthropathy: Arthroscopic findings in the shoulder and the knee. Arthroscopy 2003;19:E14-7. [Google Scholar | PubMed]
- 12.Kural C, Cetinus EM, Kural A, Ugras AA, Kaya I. Knee ochronotic arthropathy and arthroscopic findings. Acta Orthop Traumatol Turc 2009;43:67-71. [Google Scholar | PubMed]
- 13.Raaijmaakers M, Steenbrugge F, Dierickx C. Ochronosis, arthroscopy of a black knee: A case report and review of the literature. Knee Surg Sports Traumatol Arthrosc 2008;16:182-4. [Google Scholar | PubMed]