Treatment of metaphyseal–diaphyseal junctional fractures of the distal humerus is difficult in children.
Dr. Gaku Niitsuma, Department of Orthopaedic Surgery, Showa University School of Medicine, Tokyo, Japan. E-mail: gaku-nii09@med.showa-u.ac.jp
Introduction: Although there are few descriptions in textbooks and it is stated that the treatment of metaphyseal–diaphyseal junctional (MDJ) fracture is difficult, there is almost no detailed description on its treatment methods and precautions.
Case Presentation: We encountered two patients, 9-year-old and 1-year and 11-month-old Japanese boys, with MDJ fractures of the distal humerus, which are very rare in children. Unlike supracondylar fractures of the distal humerus, the fractures were spiral fractures, which made percutaneous pinning very difficult. Open reduction was performed using a bilateral approach with two skin incisions. Both patients recovered completely and had no problems carrying out activities of daily living or playing sports.
Conclusions: For patients that are old enough to receive a locking plate, we recommend fixation using a locking plate. In cases of unilateral pinning without cross-pinning, retrograde intramedullary nailing should be considered. MDJ fractures of the distal humerus should be treated as distal humeral shaft fractures, not as subtypes of supracondylar fractures of the humerus.
Keywords: Distal humeral fracture, metaphyseal–diaphyseal junction, children, open reduction.
Metaphyseal–diaphyseal junctional (MDJ) fractures of the distal humerus, which are slightly proximal to the location of humeral condyle fractures, are extremely rare as the humerus is anatomically stronger than the condyle [1,2]. To the best of our knowledge, the only conclusive report was published by Fayssoux et al. [1], including 422 humeral supracondylar fractures in 14 (3.3%) patients with MDJ fractures of the distal humerus. In addition, only Tomori et al. [2] published a case report on such MDJ fractures. Some textbooks have described the difficulty of MDJ fracture treatment; however, there is almost no detailed description on the treatment methods [3]. Here, we describe two cases of MDJ fractures of the distal humerus due to trauma, which were difficult to treat.
Ethics statements
The report was published after obtaining written informed consent from the patients’ parents to publish or use their photographs. This study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Case 1
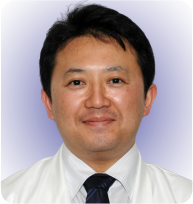
A 9-year-old Japanese boy attempted to jump over a brick flowerbed and smashed his right elbow. He visited the hospital on the day of the injury. Examination revealed no apparent neuropathy or impaired blood flow. A distal MDJ fracture of the right humerus was confirmed using radiography (Fig. 1a).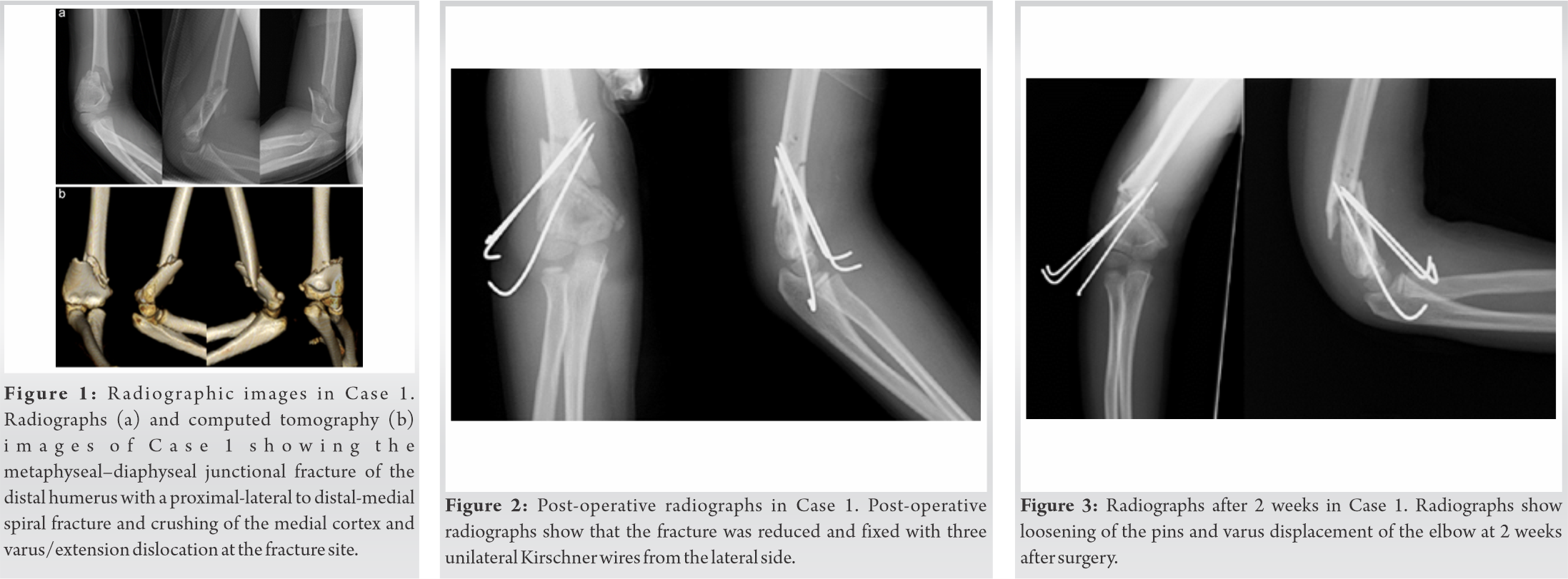 Computed tomography (CT) images revealed a proximal-lateral to distal-medial spiral fracture, with crushing of the medial cortical bone and varus/extension dislocation at the fracture site (Fig. 1b). The AO Foundation/Orthopaedic Trauma Association (AO/OTA) classification was 13-A2.2, and emergency surgery was performed on the same day with the patient under general anesthesia.
Computed tomography (CT) images revealed a proximal-lateral to distal-medial spiral fracture, with crushing of the medial cortical bone and varus/extension dislocation at the fracture site (Fig. 1b). The AO Foundation/Orthopaedic Trauma Association (AO/OTA) classification was 13-A2.2, and emergency surgery was performed on the same day with the patient under general anesthesia.
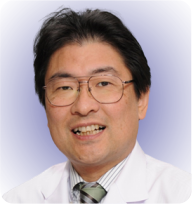
We initially considered a subtype of humeral supracondylar fracture and planned percutaneous pinning. A small incision was made on the medial side of the elbow to protect the ulnar nerve. The fracture was manually reduced, but the cortex of the medial side was crushed and difficult to maintain. We performed lateral open reduction and internal fixation (ORIF) with bone forceps, but ORIF was difficult because the medial cortex was crushed and crimping the fractured site with bone forceps caused varus displacement. While controlling the proximal and distal fracture sites with bone forceps, alignment of the entire elbow was reduced and fixed with three Kirschner wires (K-wires) from the lateral side (Fig. 2). We attempted medial cross-pinning, but we could not fix the fracture because of the large inclination angle of the fracture line. A splint was attached after surgery; varus displacement was observed 2 weeks postoperatively (Fig. 3), therefore, we performed reoperation.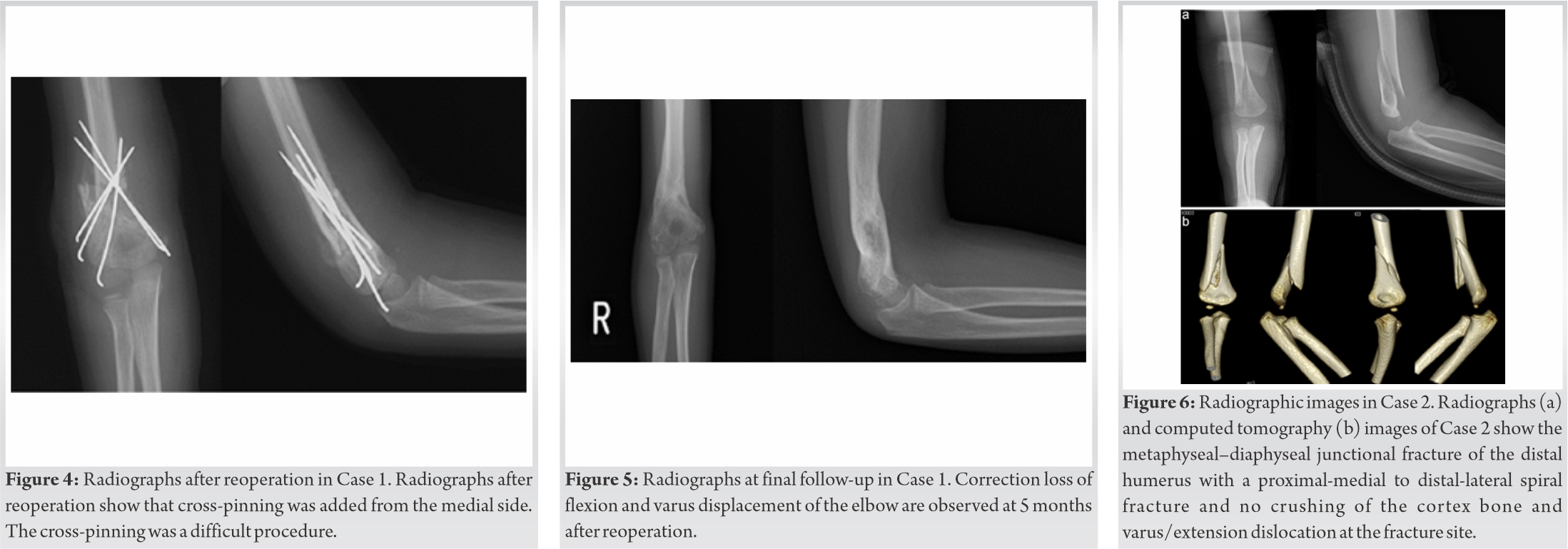
We performed lateral open reduction and medial cross-pinning (Fig. 4). It was difficult to add a cross pin. After reoperation, above-elbow (A-E) cast immobilization was used instead of a splint.
At 1 month postoperatively, callus formation was observed, and we removed the cast and started active exercise of range of motion (ROM). Four months postoperatively, bone fusion was observed, and the patient was excused from sports activities. The K-wires were removed 5 months after the reoperation (Fig. 5). The final ROM measurements (10 months postoperatively) were as follows: Flexion/extension, 115°/-15° (healthy side, 130°/10°); and supination/pronation, 90°/90° (90°/90°), with flexion/extension restriction. The final radiographic measurements were as follows: Carry angle, 3° (healthy side, 3°); Baumann angle, 9° (healthy side, 24°); and tilting angle, 47° (healthy side, 24°), with correction loss of flexion and varus of the elbow. However, he had no problems with activities of daily living.
Case 2
A 1-year and 11-month-old Japanese boy visited the hospital on the day of injury caused by the fall from a bed with no witnesses. His examination revealed no neuropathy or circulatory disorders. Radiographs showed a distal MDJ fracture of the right humerus (Fig. 6a), and CT images showed a spiral fracture. Varus displacement was observed (Fig. 6b). The AO/OTA classification was 13-A 2.2. Based on experience, we decided to perform surgery.
Predicting that manual reduction would be difficult, we protected the ulnar nerve with a medial small skin incision and performed open reduction with bone forceps from the lateral side, aiming for cross-pinning from the beginning. When we reduced the fracture site laterally, we noticed kinking of the radial nerve at the fracture site; however, there was no macroscopic damage. Thus, the radial nerve was detached and protected. The direction of the spiral fracture was opposite to that in Case 1, and we could reduce the fracture with bone forceps from the lateral side. We fixed three K-wires from the medial side, but it was impossible to fix the cross-pinning from the lateral side because of the large angle of inclination of the fracture line. As in Case 1, we fixed three unilateral pins (Fig. 7). A-E cast was fixed immediately after surgery. However, varus displacement persisted 3 days postoperatively (Fig. 8a). The cast was manually reduced to valgus alignment using radiographic fluoroscopy (Fig. 8b). Thereafter, dislocation did not recur, and reoperation was not required.
One month after surgery, callus formation appeared, and we removed the cast and started ROM exercises. Bone fusion was observed, and the K-wires were removed 3 months postoperatively. Five months after surgery, ROM measurements of the elbow were as follows: Flexion/extension, 130°/10° (healthy side, 130°/10°); and pronation/supination, 90°/90° (healthy side, 90°/90°). The final radiographic measurements were as follows: CA, 11° (healthy side, 11°); BA, 26° (healthy side, 26°); and TA, 32° (healthy side, 22°) (Fig. 9). The patient had no radial nerve symptoms.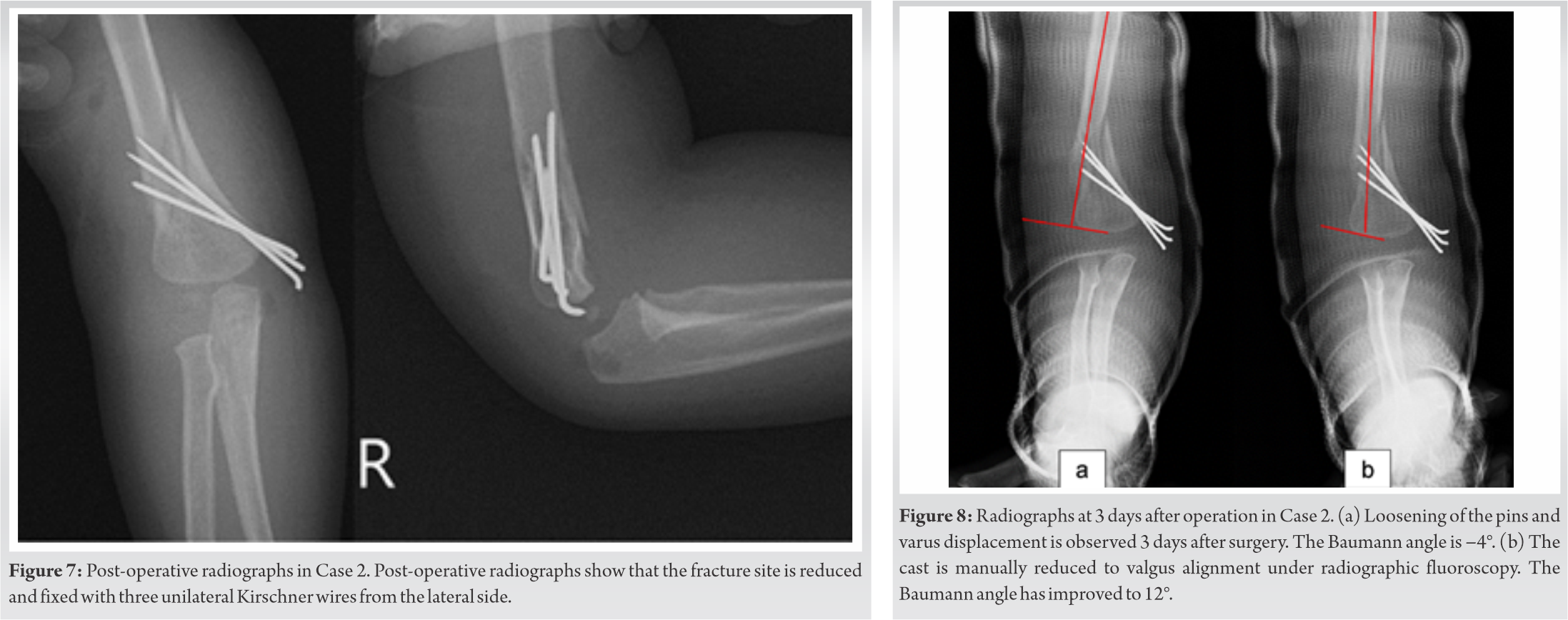
MDJ fractures of the distal humerus are considered more unstable than supracondylar fractures because the bone shape is closer to a triangle compared to the supracondyle and condyle of the humerus [4]. In addition, as the periosteum is thin, bone fusion takes time. However, MDJ fracture of the distal humerus is stronger than that of the humeral supracondyle because the cortex is thicker and the bone stock is larger [5,6]. Thus, MDJ fractures of the distal humerus may be oblique or spiral fractures that break from the thick cortex of the MDJ toward the thin olecranon fossa [1].
It is important to recognize that MDJ fractures of the distal humerus should be treated as distal shaft fractures, not as a subtype of supracondylar fractures [1,2].
Surgical approach: In MDJ fractures, as in the case of humeral supracondylar fractures, a medial incision was used to protect the ulnar nerve and was planned to be fixed with cross-pinning. However, it was difficult to maintain manual reduction, and we reduced the open reduction from the lateral side, resulting in a bilateral approach. Tomori et al. [2] reported that with the anterior approach, the fracture site could be reduced by thumb compression. Rizk [7] reported a posterior approach and performed fixation with cross-pinning to preserve the triceps. In our bilateral approach, the scar is not large and is less noticeable compared to that used in the anterior or posterior approach. However, it is difficult to determine the center of the fracture site. The brachial artery and median nerve can be confirmed by the anterior approach; however, if the median nerve is not expanded when the K-wires are inserted, there is a risk of ulnar nerve damage, and a large, highly invasive scar. The posterior approach is considered disadvantageous cosmetically because it is highly invasive and carries a risk of skin necrosis caused by a larger skin incision. A textbook also recommends a lateral or posterolateral approach for radial nerve protection [3].
In Case 1, ORIF was performed laterally without considering the direction of the spiral fracture and crushed site. During ORIF from the medial region, it is necessary to perform neurolysis to protect the ulnar nerve. However, neurolysis is invasive, reduction is difficult, and correction loss persists. We found that lateral ORIF was disadvantageous because the fracture type was difficult to reduce, and medial side ORIF may be preferable. It is necessary to consider whether to perform open reduction from the lateral or medial side depending on the direction of the fracture line before surgery.
Emergency surgery: On the day of the injury, we performed emergency surgery for humeral supracondylar fractures because these fractures may cause brachial arterial or nerve injury and Volkmann contracture or callus myositis due to the displacement of the fracture site. In MDJ fractures, the distal fragment is displaced proximally, and the radial nerve is trapped and injured between fragments of the MDJ fracture of the distal humerus [4]. However, the brachial artery and median nerve may become pinched or damaged anteriorly. When neuropathy or blood flow disorder is not observed before surgery, as in this case, it is possible to prepare the locking plate for elective surgery.
Internal fixation of fractures: In elective surgery, Case 1 was 9 years old, and we considered ORIF with a locking plate. The fracture was unstable because it was a spiral fracture; it was difficult to manually reduce the fracture and perform cross-pinning. Therefore, we recommend locking plate fixation in similar cases. However, Case 2 was an infant younger than 2 years of age, and no appropriately sized locking plates for infants are available. Depending on the patient’s age and physique, locking plates may not be usable, and intramedullary nails or pinning is required. Liu et al. [8] and Kamara et al. [9] compared each internal fixation method (number of cross-pins, number of unilateral pins, number of intramedullary nails, and use of external fixation combined with unilateral pinning) for MDJ fractures of the distal humerus using finite element method analysis. Three cross pins (two perpendicular to the fracture line and one contralateral) were the strongest followed by intramedullary nails and two cross pins (one lateral and one medial). Unilateral pinning suggests that either two or three pins have weak fixational force. Cross-pinning should be attempted first, but cross-pinning is very difficult because of similar distal humeral shaft fractures [2].
Some reports exist on using them intramedullary antegrade or retrograde nails to treat humeral shaft fractures [10]. Antegrade nails must be used in the surgical techniques. Children have short and thick extremities; therefore, it is difficult to use antegrade nails during open reduction using a tourniquet, as in Case 2. In addition, antegrade nails reportedly have a greater possibility of varus displacement than retrograde nails [11]. Based on these findings, retrograde intramedullary nails are recommended. Tomori et al. reported that in pediatric cases, treatment only includes intramedullary nails and cast immobilization because bone fusion occurs rapidly in children [2]. However, MDJ fractures of the distal humerus are unstable; the fixation force for rotation is weak with only intramedullary nails and cast immobilization, and the risk of dislocation is high. Therefore, the fixation force of the cast is unreliable and surgical treatment is preferred. However, in Case 2, dislocation was caused by unilateral pinning, and there was a history of manual reduction and cast immobilization; thus, it is possible that the patient could have been managed by conservative treatment. In our cases, we performed surgical instead of conservative treatment because of our experience with Case 1.
Therefore, cross-pinning should first be used. When cross-pinning is difficult, the fixation force will be weak only with intramedullary nails or unilateral pinning, as in our report. We propose a hybrid method that combines three or more unilateral pins and two or more retrograde intramedullary nails (Fig. 10).
Pediatric MDJ fractures of the distal humerus are rare and difficult to treat. Percutaneous cross-pinning may not be possible for treating humeral supracondylar fractures. If the patients are old enough to receive the locking plate, we recommend locking plate fixation. Retrograde intramedullary nails should be considered instead of overestimating cast immobilization when only unilateral pinning is used for fixation.
This report describes the treatment of pediatric MDJ fractures of the distal humerus. If the patients are old enough to receive the locking plate, we recommend locking plate fixation. Retrograde intramedullary nails should be considered instead of overestimating cast immobilization when only unilateral pinning is used for fixation. MDJ fractures should be treated as distal shaft fractures, not as subtypes of supracondylar fractures.
References
- 1.Fayssoux RS, Stankovits L, Domzalski ME, Guille JT. Fractures of the distal humeral metaphyseal-diaphyseal junction in children. J Pediatr Orthop 2008;28:142-6. [Google Scholar | PubMed]
- 2.Tomori Y, Sawaizumi T, Nanno M, Takai S. A case report: Distal humeral diaphyseal fracture in a child. Medicine (Baltimore) 2017;96:e5812. [Google Scholar | PubMed]
- 3.Bae BS. Proximal humerus fractures. Humeral shaft and proximal humerus, shoulder dislocation. In: Rockwood CA Jr., Wilkins KE, editors. Fractures in Children. 8th ed. Philadelphia, PA: Wolters Kluwer; 2001. p. 784-800. [Google Scholar | PubMed]
- 4.Perez EA. Fractures of the shoulder, arm, and forearm. In: Canale ST, Beaty JH, editors. Campbell’s Operative Orthopaedics. 12th ed. Philadelphia, PA: Elsevier Mosby; 2013. p. 2860-1. [Google Scholar | PubMed]
- 5.Williams J. Humerus, shaft. In: Buckley RE, Moran CG, Apivatthakakul T, editors. AO Principles of Fracture Management. 3rd ed., Ch. 6.2.2. Switzerland: AO Foundation, Davos Platz; 2018. p. 579-93. [Google Scholar | PubMed]
- 6.Skaggs DL, Flynn JM. Principle of management. Supracondylar fractures of the distal humerus. In: Rockwood CA Jr., Wilkins KE, editors. Fractures in Children. 8th ed. Philadelphia, PA: Wolters Kluwer; 2001. p. 582. [Google Scholar | PubMed]
- 7.Rizk AS. Triceps-sparing approach for open reduction and internal fixation of neglected displaced supracondylar and distal humeral fractures in children. J Orthop Traumatol 2015;16:105-16. [Google Scholar | PubMed]
- 8.Liu C, Kamara A, Liu T, Yan Y, Wang E. Mechanical stability study of three techniques used in the fixation of transverse and oblique metaphyseal-diaphyseal junction fractures of the distal humerus in children: A finite element analysis. J Orthop Surg Res 2020;15:34. [Google Scholar | PubMed]
- 9.Kamara A, Ji X, Liu T, Zhan Y, Li J, Wang E. A comparative biomechanical study on different fixation techniques in the management of transverse metaphyseal-diaphyseal junction fractures of the distal humerus in children. Int Orthop 2019;43:411-6. [Google Scholar | PubMed]
- 10.Marengo L, Canavese F, Cravino M, De Rosa V, Rousset M, Samba A, et al. Outcome of displaced fractures of the distal metaphyseal-diaphyseal junction of the humerus in children treated with elastic stable intramedullary nails. J Pediatr Orthop 2015;35:611-6. [Google Scholar | PubMed]
- 11.Ge YH, Wang ZG, Cai HQ, Yang J, Xu YL, Li YC. Flexible intramedullary nailing had better outcomes than kirschner wire fixation in children with distal humeral metaphyseal-diaphyseal junction fracture: A retrospective observational analysis. Int J Clin Exp Med 2014;7:3568-72. [Google Scholar | PubMed]