Old patellar tendon can be managed with good functional outcome after reconstruction with peroneus longus autograft.
Dr. Saroj Kumar Patra, Department of Trauma and Emergency, AIIMS, Bhubaneswar, Odisha, India. E-mail: drsaroj123@gmail.com
Introduction: Patellar tendon rupture is a rare injury and is often missed in primary and secondary care centers because of non-visibility in X-rays. Neglected rupture is even rarer and gives rise to significant disability. These injuries are technically difficult to repair with invariably poor functional outcomes. This needs reconstruction with allograft or autograft with or without augmentation. We report such a case of neglected patellar tendon injury treated with peroneus longus autograft.
Case Report: A 37-year-old male patient presented with limping and inability to do a full extension of the knee. There is a history of a lacerated wound over the knee following a bike accident. Reconstruction was done with peroneus longus auto graft by making a trans-osseous tunnel through the patella and tibial tuberosity in the Figure eight 8 manner and fixed by a suture anchor. Postoperatively, the patient was doing well at a 1-year follow-up.
Conclusion: Good clinical outcomes can be achieved in neglected patellar tendon rupture by auto graft without augmentation.
Keywords: Patellar tendon, tendon reconstruction, chronic rupture of the patellar tendon
The incidence of patellar tendon rupture is only 0.68/100000 individuals with neglected rupture still rare [1]. It is usually seen in patients below the age of 40 [2]. Often these types of injuries are missed in primary and secondary centers, which later leads to disabilities such as inadequate knee extension and limping. Unilateral ruptures are always seen following trauma whereas bilateral ruptures are seen following systemic diseases. We report a case of traumatic patellar tendon rupture in a young male who was misdiagnosed in the primary center and getting neglected for 6 months. Patellar tendon reconstruction was done with a trans osseous tunnel in patella and tibia tuberosity in Figure 8 fashion taking peroneus longus autograft. The patient was doing well in the post-operative period with normal knee extension without lag.
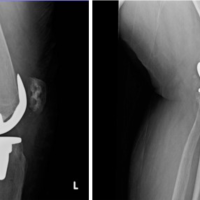
A 37-year-old male presented with decreased range of movement, difficulty during stair climbing, and standing from a seated position. His family members also noticed him limping during walking. There was a history of fall from the bike and had an open injury over the knee six months back. The patient had treated at a local primary center and stitching of the wound was done. At that time, the X-ray was within normal limits due to which patellar tendon rupture was missed primarily. He later consulted us after Six months of injury. On examination, there is a healed scar mark present over the infra-patellar area. A visible and palpable gap is present between the patella and tibial tuberosity with discontinuation of the patellar tendon (Fig. 1a). Tenderness elicited on patellofemoral grinding. There is no local rise in temperature and no synovial thickening. The range of knee movement was 40–135° with a knee extension lag of 45° (Fig. 1b). Quadriceps muscle power was 4/5. His hematological investigation including complete blood count, erythrocyte sedimentation rate, and C-reactive protein was within normal limits. Plain lateral X-ray shows upward migration of patella with a high Insall-Salvati ratio (more than 1.2) (Fig. 1c). MRI knee showed a complete tear of the patellar tendon and a vertical tear in the posterior horn of the lateral meniscus (Fig. 1d). A diagnosis of a 6-month-old patellar tendon rupture was made. The patient was planned for surgical intervention. Patient with supine position, an anterior midline skin incision extending from the superior pole of the patella to tibial tuberosity was given. Complete exposure of the patellar tendon was done by elevating a large medial and lateral side flap. The tendon was found to be ruptured with scarring at both ends (Fig. 2a). After careful dissection and release of the parapatellar retinaculum, the patella could be brought down to its anatomical position. Semitendinosus tendon autograft was planned to be used for the reconstruction of the ruptured tendon. However, during the tendon harvest, it was found to be thinner than expected, and hence procedure was abandoned, and an ipsilateral peroneus tendon graft was harvested in a standard manner (Fig. 2b).
Tenderness elicited on patellofemoral grinding. There is no local rise in temperature and no synovial thickening. The range of knee movement was 40–135° with a knee extension lag of 45° (Fig. 1b). Quadriceps muscle power was 4/5. His hematological investigation including complete blood count, erythrocyte sedimentation rate, and C-reactive protein was within normal limits. Plain lateral X-ray shows upward migration of patella with a high Insall-Salvati ratio (more than 1.2) (Fig. 1c). MRI knee showed a complete tear of the patellar tendon and a vertical tear in the posterior horn of the lateral meniscus (Fig. 1d). A diagnosis of a 6-month-old patellar tendon rupture was made. The patient was planned for surgical intervention. Patient with supine position, an anterior midline skin incision extending from the superior pole of the patella to tibial tuberosity was given. Complete exposure of the patellar tendon was done by elevating a large medial and lateral side flap. The tendon was found to be ruptured with scarring at both ends (Fig. 2a). After careful dissection and release of the parapatellar retinaculum, the patella could be brought down to its anatomical position. Semitendinosus tendon autograft was planned to be used for the reconstruction of the ruptured tendon. However, during the tendon harvest, it was found to be thinner than expected, and hence procedure was abandoned, and an ipsilateral peroneus tendon graft was harvested in a standard manner (Fig. 2b). The graft was prepared on a graft board with both ends whip stitched with no.2 Fiber-wire suture. The graft was 26 cm in length and 4.5 mm in diameter. Accordingly, a 5 mm drill hole was made in the mid-patella region. The patella was further pulled down by a stainless-steel wire through the tunnel, to its anatomical position. The graft was passed from the lateral to the medial side of the patella through the tunnel, crossed over in a figure of eight fashion, and passing it through a 5 mm tunnel made horizontally posterior to the tibial tuberosity. Patella was appropriately positioned keeping the patella height and effective length of the reconstructed tendon equal. The graft under tension in this position was fixed to the tibia tunnel with a bioabsorbable screw (Fig. 2c). Additional graft fixation was done with a suture anchor at the proximal tibia (Fig. 2d). The remaining native patella tendon, although of poor quality was sutured for augmenting it. In the early post-operative period, the knee was immobilized in a long knee brace, but static quadriceps exercise was resumed on the 1st post-operative day. The post-operative radiograph showed the position of the patella being like the opposite side and no patella Baja was noted (Fig. 3a). After 3 weeks, knee flexion was initiated, and the patient started walking with a hinge knee brace allowing a gradual increase of flexion of the knee. Up to 90° flexion was achieved in 6 weeks while continuing quadriceps strengthening (Fig. 3b and c). The patient was under regular follow-up and counseled regarding physiotherapy as advised. At 1-year follow-up, knee flexion was possible up to 110°, there was no extensor lag and quadriceps strength was like the opposite side.
The graft was prepared on a graft board with both ends whip stitched with no.2 Fiber-wire suture. The graft was 26 cm in length and 4.5 mm in diameter. Accordingly, a 5 mm drill hole was made in the mid-patella region. The patella was further pulled down by a stainless-steel wire through the tunnel, to its anatomical position. The graft was passed from the lateral to the medial side of the patella through the tunnel, crossed over in a figure of eight fashion, and passing it through a 5 mm tunnel made horizontally posterior to the tibial tuberosity. Patella was appropriately positioned keeping the patella height and effective length of the reconstructed tendon equal. The graft under tension in this position was fixed to the tibia tunnel with a bioabsorbable screw (Fig. 2c). Additional graft fixation was done with a suture anchor at the proximal tibia (Fig. 2d). The remaining native patella tendon, although of poor quality was sutured for augmenting it. In the early post-operative period, the knee was immobilized in a long knee brace, but static quadriceps exercise was resumed on the 1st post-operative day. The post-operative radiograph showed the position of the patella being like the opposite side and no patella Baja was noted (Fig. 3a). After 3 weeks, knee flexion was initiated, and the patient started walking with a hinge knee brace allowing a gradual increase of flexion of the knee. Up to 90° flexion was achieved in 6 weeks while continuing quadriceps strengthening (Fig. 3b and c). The patient was under regular follow-up and counseled regarding physiotherapy as advised. At 1-year follow-up, knee flexion was possible up to 110°, there was no extensor lag and quadriceps strength was like the opposite side.
Patellar tendon injury happens following trauma and is usually unilateral [3,4]. Most tendon injury diagnosed early, and repair is done primarily. Whereas chronic patellar tendon injuries following trauma are presented late because of neglect, native treatment, or missed injury [1]. Non-operative management has limited indications and does not restore the function of the affected extremity. These cases of chronic ruptures of the patella tendon have small distal stumps with poor tissue quality and fibrosis. Hence, end to end repair of the tendon is not feasible or inadequate and the need for autograft / allograft / artificial graft is almost indispensable for surgical management of chronic ruptures. Patella due to contracted quadriceps migrating upwards and extensive release is required to bring it down to normal position [3,5,6]. The reconstruction procedure of the patella tendon should be compatible with the biomechanical load produced during quadriceps contraction to allow early and optimum rehabilitation and better functional outcomes [2]. Suture anchor augmentation with suture tape internal brace has been evaluated for the repair of acute ruptures and found to provide adequate strength. The cerclage wire technique has been used to strengthen the repair or reconstruction with a single [7] or multiple strands of wire in the figure of eight fashion [8]. However, longer operative time, risk of intraoperative fracture, risk of infection, re-surgery for hardware removal, and limitation of terminal flexion are the complication associated with it. Suture anchors are being used efficiently for the rupture of the quadriceps mechanism in the superior pole of the patella [9]. In our case, fixation of the graft with a suture anchor and bioabsorbable screw made it stable enough to allow immediate mobilization and early range of motion though we delayed active extension of the knee from a flexed position to allow healing of the tendon-bone interface. Patella Alta increases tension over repair/ reconstructed tendon and should be brought down to anatomic position. Lengthening of quadriceps by V-Y plasty or Z-lengthening or applying pre-operative pin traction was performed by some surgeons to allow the patella to come distally but was not required in our case [4]. When lengthening is carried out, it can cause a decrease in quadriceps power and may be difficult to regain complete power in the subsequent period. Hence, we preferred to bring down the patella by a stainless-steel wire intraoperatively with a fixation on the tibial side by bio screw and suture anchor to get a stable reconstruction of the patellar tendon.
Good knee range of motion and functional outcome was obtained in chronic patella rupture patients by reconstruction with peroneus longus tendon.
All cases of open knee injuries must be assessed adequately for tendon and ligament injuries. Neglected patellar tendon rupture can be managed by reconstruction with peroneus longus and gives a satisfactory outcome.
References
- 1.Core M, Anract P, Raffin J, Biau DJ. Traumatic patellar tendon rupture repair using synthetic ligament augmentation. J Knee Surg 2020;33:804-9. [Google Scholar | PubMed]
- 2.Matava MJ. Patellar tendon ruptures. J Am Acad Orthop Surg 1996;4:287-96. [Google Scholar | PubMed]
- 3.Bek D, Demiralp B, Kömürcü M, Sehirlioğlu A. Neglected patellar tendon rupture: A case of reconstruction without quadriceps lengthening. J Orthop Traumatol 2008;9:39-42. [Google Scholar | PubMed]
- 4.Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am 1981;63:932-7. [Google Scholar | PubMed]
- 5.Ayas MS, Gül O, Okutan AE, Turhan AU. Extensor mechanism reconstruction with peroneus longus tendon autograft for neglected patellar fracture, report of 2 cases. J Clin Orthop Trauma 2019;10(Suppl 1):S226-30. [Google Scholar | PubMed]
- 6.Jain S, Jain AK, Dhammi IK, Modi P. Neglected patellar tendon rupture treated by trans-osseous Encirclage wire and turn-o-flap: Case report. J Orthop Case Rep 2014;4:5-8. [Google Scholar | PubMed]
- 7.Lewis PB, Rue JP, Bach BR Jr. Chronic patellar tendon rupture: Surgical reconstruction technique using 2 Achilles tendon allografts. J Knee Surg 2008;21:130-5. [Google Scholar | PubMed]
- 8.Ramanath SK, Shah RH, Patil S, Umesh S. Reconstruction of neglected patellar tendon rupture using Tendoachilles’ allograft with transosseous tunnels: A case report. J Orthop Case Rep 2020;10:27-9. [Google Scholar | PubMed]
- 9.Phillips K, Costantino TG. Diagnosis of patellar tendon rupture by emergency ultrasound. J Emerg Med 2014;47:204-6. [Google Scholar | PubMed]