Giant cell tumor of tendon sheath of flexor pollicis longus tendon is an uncommon entity, can be managed easily with careful excision, and should be carefully followed up to detect recurrences early.
Dr. Aashay Sonkusale, Department of Orthopaedics, Indira Gandhi Government Medical College and Hospital, Nagpur, Maharashtra, India. E-mail: aashay49@gmail.com
Introduction: Giant cell tumors of tendon sheath are benign, rarely malignant, soft-tissue tumors arising from tenosynovial sheath and periarticular soft tissue. They usually present as painless masses with some restriction of movement. Histopathological diagnosis is gold standard although pre-operative fine-needle aspiration cytology (FNAC), plain radiographs, and MRI help in narrowing down the differentials. Giant cell tumor of the tendon sheath (GCTTS) although benign is notorious for having a high rate of recurrences, with most important risk factors being adjacency to joint and incomplete excision. Adequate marginal excision forms the mainstay for managing these tumors. Adjuvant radiotherapy has found some role in treating and decreasing the chances of recurrences.
Case Report: A 55-year-old lady was brought to the outpatient department with a history of painless, gradually progressive swelling on volar aspect of thumb. Swelling was well defined with a smooth surface. Overlying skin showed no signs of local inflammation or adherence. Pain radiographs showed soft-tissue shadow with some articular bony erosions. A ultrasound-guided FNAC and MRI showed a picture of GCTTS. An excisional biopsy was done and confirmed the diagnosis.
Conclusion: GCTTS is a benign entity with a slow course of evolution, although uncommon, and should be kept as differential for swellings of hand and feet. Complete excision with no evidence residual tumor is diagnostic as well as curative. A regular follow-up is essential on account of high rates of recurrences.
Keywords: Giant cell tumor of tendon sheath, thumb, flexor pollicis longus, excisional biopsy.
Giant cell tumor of tendon sheath is benign, fibrous soft-tissue tumor originating from the tenosynovial sheath, bursae, and synovium of the joint [1]. It is considered to be the most common soft-tissue tumor of the hand second only to arthrosynovial cyst [2]. The finger is most frequently involved with most common in the index finger [3]. Various nomenclatures have been described in the literature for giant cell tumor of the tendon sheath (GCTTS) including pigmented villonodular synovitis, localized nodular synovitis, fibrous histiocytoma of the synovium, myeloid epithelioma, sclerosing hemangioma, xanthoma granuloma, and giant cell fibrohemangiona [4,5]. It most commonly affects adults in the 30–50 age group with a predominant female predilection (M:F = 2:3) [6]. GCTTS is mostly benign with low likely hood of malignancy and high rate of recurrence. We report a case of an old 55-year-old female patient diagnosed with GCTTS aimed at studying the diagnostic, therapeutic, and prognostic aspects.
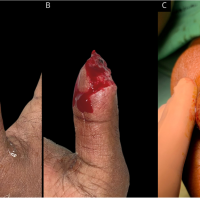
A 55-year-old lady presented to the outpatient department with complaints of swelling on volar aspect and restriction of movement of the right thumb for 1 year. She gave a history of non-specific blunt trauma to the right thumb 6 months before the onset of swelling following which she had mild pain for a period of 1 week, which resolved with rest and oral analgesics. The swelling presented insidiously initially the size of a pea which gradually progressed to a current size of 6×1.5×1 cm. On local examination, a single irregular swelling of soft-to-firm consistency on the volar aspect of the right thumb extending from the distal aspect of the proximal phalanx over the interphalangeal (IP) joint to the distal phalanx was noted. Swelling was well defined with a smooth surface. Overlying skin showed no signs of local inflammation or adherence. There was restriction of movement at the IP joint due to mass effect. There was no area of paresthesia over the thumb and capillary refill was normal. Routine blood investigations were within normal limits. Plain radiographs of the hand in anteroposterior and oblique views showed a localized soft-tissue swelling on the volar aspect of thumb with cortical erosions seen on the articular surfaces of IP joint, more on the proximal phalanx than distal (Fig. 1).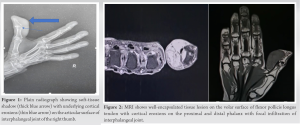 Ultrasonography showed heterogeneously hypoechoic lesion of size 2.8×1.8×2.3 cm on the anteromedial aspect volarly at the IP joint with underlying erosion of bony cortex. Ultrasound-guided fine-needle aspiration cytology (FNAC) showed scant cellularity comprising of few osteoclastic type of giant cells with few mononuclear cells against a hemorrhagic background suggestive of GCTTS. Magnetic resonance imaging showed a well-encapsulated lesion of altered intensity of size 2×1.8×4 cm on the anteromedial aspect of volar surface arising from flexor pollicis longus tendon with infiltration and focal breach at IP joint. It appeared heterogeneously hypointense on T2, isointense on T1-weighted images, hyperintense on PDFS with areas of blooming on gradient sequence, and post-contrast enhancement – princeps pollicis being the feeding vessel. Cortical erosions on the palmar surface of proximal and distal phalanx were noted (Fig. 2). An open excisional biopsy was planned. Under sedation and local anesthetic block, a tourniquet was applied using the finger of a sterilized glove. A Z-shaped Bruner’s incision was taken directly over the most prominent part of the swelling. The mass was carefully dissected off the flexor tendon preserving the cutaneous nerve and vessel. The A1 and A2 pulley along with the tendon were intact. Closure was done in two layers and tourniquet was released. A polyploidal lobulated fibrofatty mass (Fig. 3) was obtained which was sent for histopathological examination.
Ultrasonography showed heterogeneously hypoechoic lesion of size 2.8×1.8×2.3 cm on the anteromedial aspect volarly at the IP joint with underlying erosion of bony cortex. Ultrasound-guided fine-needle aspiration cytology (FNAC) showed scant cellularity comprising of few osteoclastic type of giant cells with few mononuclear cells against a hemorrhagic background suggestive of GCTTS. Magnetic resonance imaging showed a well-encapsulated lesion of altered intensity of size 2×1.8×4 cm on the anteromedial aspect of volar surface arising from flexor pollicis longus tendon with infiltration and focal breach at IP joint. It appeared heterogeneously hypointense on T2, isointense on T1-weighted images, hyperintense on PDFS with areas of blooming on gradient sequence, and post-contrast enhancement – princeps pollicis being the feeding vessel. Cortical erosions on the palmar surface of proximal and distal phalanx were noted (Fig. 2). An open excisional biopsy was planned. Under sedation and local anesthetic block, a tourniquet was applied using the finger of a sterilized glove. A Z-shaped Bruner’s incision was taken directly over the most prominent part of the swelling. The mass was carefully dissected off the flexor tendon preserving the cutaneous nerve and vessel. The A1 and A2 pulley along with the tendon were intact. Closure was done in two layers and tourniquet was released. A polyploidal lobulated fibrofatty mass (Fig. 3) was obtained which was sent for histopathological examination.  Histopathological examination showed a mixture of osteoclastic multinucleated giant cells, xanthoma cells, and chronic inflammatory cells in a collagenous matrix – typical of GCTTS (Fig. 4). Post-operative period was uneventful. 6-month follow-up showed no evidence of recurrence on clinical and radiologic examination. Flexion at the IP joint and metacarpophalangeal joint of thumb were unrestricted with normal capillary refill.
Histopathological examination showed a mixture of osteoclastic multinucleated giant cells, xanthoma cells, and chronic inflammatory cells in a collagenous matrix – typical of GCTTS (Fig. 4). Post-operative period was uneventful. 6-month follow-up showed no evidence of recurrence on clinical and radiologic examination. Flexion at the IP joint and metacarpophalangeal joint of thumb were unrestricted with normal capillary refill.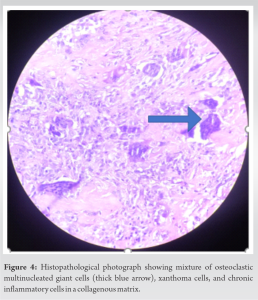
Giant cell tumor of tendon sheath is not really tumors but is more appropriately grouped under reactive lesions similar to PVNS. They may also arise from the bursae or synovium [7]. The etiology of GCTTS is not clear with some theories relating it to an inflammatory reaction [8]. GCTTS starts spontaneously although some patients report and relate it subsequent to an event of minor trauma [9] and presents as a slow-growing, painless mass with minimal functional disability leading to late presentations. GCTTS can be of two types – intraarticular and extrarticular. According to clinical and biological presentation, it can be localized or diffuse. Localized form is more common, occurs in the hands and feet, and is benign. It can be easily controlled with a marginal resection. In case of recurrences, a simple marginal resection again suffices. Diffuse form is the less frequent entity and involves the large joints with high rates of malignant transformation and recurrences. Ozben and Coskun [10] report a recurrence after surgical excision as high as 15–45% with joint capsule adjacency and incomplete removal as the most important risk factors. Other risk factors mentioned by Ushijima et al. [2] with low level of evidence include cortical destruction, presence of degenerative joint disease, and tumors with increased mitosis activity neurovascular dissection during excision. Al Qattan et al. [11] classifies GCTTS as type 1 – single round or multilobulated tumor and type 2 – two or more distinct separate tumors based on MRI and intraoperative findings, with type 2 being the more ominous one. Lancigu et al. [12] reviewed that 96 patients with a follow-up of 12 years are found out recurrences typically occur within 36 months of index surgery and factors which positively influence recurrences are intraarticular infiltration, tendon involvement, and marginal excision. Histologic type did not seem to affect the rate of recurrences. Kotwal et al. [13] advocated post-operative radiotherapy of 20 Gy in daily doses of 2 Gy in case having positive risk factors and reported a 0% recurrence rate in a series of 14 cases but did not recommend routine use. However, the role of radiotherapy is not well established and remains controversial. This case report presents a case of giant cell tumor of flexor pollicis longus tendon sheath. Diagnosis suspected on clinical and plain radiographic examination was supplemented by MRI and FNAC and was confirmed on histopathological examination of excised specimen. The patient was followed up for 6 months post-operatively with no clinical or radiologic signs of recurrence and is planned to be followed up for a period of 36 months.
GCTTS is a benign entity with a slow course of evolution, although uncommon, and should be kept as differential for swellings of hand and feet. Local malignancy on account of infiltration of noble structures is common. Complete excision with no evidence residual tumor is diagnostic as well as curative. Rates of recurrences are high and patients should be followed up for early detection and management of recurrences.
A differential of giant cell tumor of tendon sheath should also be kept in mind while evaluating a case of hand/finger swelling. Recurrences are common, therefore complete excision without evidence of residual tumor is essential.
References
- 1.Lanzinger WD, Bindra R. Giant cell tumor of the tendon sheath. J Hand Surg Am 2013;38:154-7. [Google Scholar | PubMed]
- 2.Ushijima M, Hashimoto H, Tsuneyoshi M, Enjoji M. Giant cell tumour of the tendon sheath (nodular tenosynovitis). A study of 207 cases to compare the large joint group with the common digit group. Cancer 1986;57:875-84. [Google Scholar | PubMed]
- 3.Lautenbach M, Kim S, Millrose M, Eisenschenk A. Nodular giant cell tumour of the tendon sheath of the hand: Analysis of eighty-four cases: Diagnostic decisions and outcome. Int Orthop 2013;37:2211-5. [Google Scholar | PubMed]
- 4.Darwish FM, Haddad WH. Giant cell tumour of tendon sheath: Experience with 52 cases. Singapore Med J 2008;49:879-82. [Google Scholar | PubMed]
- 5.Adams EL, Yoder EM, Kasdan ML. Giant cell tumour of tendon sheath: Experience with 65 cases. Eplasty 2012;12:e50. [Google Scholar | PubMed]
- 6.Kant KS, Manav AK, Kumar R, Abhinav, Sinha VK, Sharma A. Giant cell tumour of tendon sheath and synovial membrane: A review of 26 cases. J Clin Orthop Trauma 2017;8 Suppl 2:96-9. [Google Scholar | PubMed]
- 7.Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, Walker EA. Pigmented villonodular synovitis: Radiologic-pathologic correlation. Radiographics 2008;28:1493-518. [Google Scholar | PubMed]
- 8.Kerfant N, Bardin T, Roulot E. Multiple giant cell tumors of the tendon sheath: Separate volar and dorsal lesions involving three digits of the same hand following repetitive trauma. J Hand Microsurg 2015;7:233-5. [Google Scholar | PubMed]
- 9.Fawi HM, Dojcinov S, Lyons K, Matthews TJ. Trauma or tumour: Giant cell tumour of distal biceps tendon sheath, an unusual cause of elbow pain. Shoulder Elbow 2019;11:137-9. [Google Scholar | PubMed]
- 10.Ozben H, Coskun T. Giant cell tumor of tendon sheath in the hand: Analysis of risk factors for recurrence in 50 cases. BMC Musculoskelet Disord 2019;20:457. [Google Scholar | PubMed]
- 11.Al-Qattan MM. Giant cell tumours of tendon sheath: Classification and recurrence rate. J Hand Surg Br 2001;26:72-5. [Google Scholar | PubMed]
- 12.Lancigu R, Rabarin F, Jeudy J, Saint Cast Y, Cesari B, Fouque PA, et al. Giant cell tumors of the tendon sheaths in the hand: Review of 96 patients with an average follow-up of 12 years. Orthop Traumatol Surg Res 2013;99 4 Suppl:S251-4. [Google Scholar | PubMed]
- 13.Kotwal PP, Gupta V, Malhotra R. Giant-cell tumour of the tendon sheath. Is radiotherapy indicated to prevent recurrence after surgery? J Bone Joint Surg Br 2000;82:571-3. [Google Scholar | PubMed]