Impalement injuries need careful evaluation, proper planning, and removal under vision with adequate antibiotic coverage.
Dr. Joyance James, Department of Orthopaedics, Jiwan Jyoti Christian Hospital, Robertsganj (Affiliated to Emmanuel hospital Association), Uttar Pradesh, India. E-mail: joyancejames@yahoo.co.in
Introduction: Impalement injuries are relatively rare injuries but they can present with significant surgical challenges depending on the site of injury. They can occur through a variety of mechanisms such as fall on a sharp object, assault with a sharp object, high-velocity road traffic accidents, and shrapnel injuries during a blast. Adequate pre-operative planning and surgical execution is of utmost importance for optimal outcome.
Case Report: We report a case of a 7-year-old child who presented with an impalement injury with a metal rod of a fence, following a fall on the fence while playing. The rod was removed under vision after ruling out any vascular injury. The child recovered without any residual deficits or sequelae.
Conclusion: Proper history and mechanism of injury should be verified at the outset. Complete evaluation should be done to make sure it is a local injury; vascular and neurological status needs to be confirmed and documented before any procedure. Removal under vision in the operating theater under the cover of adequate antibiotics and debridement and wound lavage reduces rates of infection and post-operative morbidity.
Keywords: Impalement injury, penetrating injury, metal rod.
Impalement injuries are rare penetrating injuries which can present with significant contamination. They can occur because of a fall from height, a high-velocity road accident, assault with sharp object. These injuries are relatively rare and a review of literature reveals only occasional case reports. Careful inspection of the affected limb and surrounding environment, minimal handling, and prompt transfer to a center equipped to handle such cases, evaluation, broad-spectrum antibiotics, tetanus toxoid prophylaxis, and removal under anesthesia with proper debridement are essential for a good outcome. There can be a delay in the diagnosis of neurovascular deficits, especially in upper extremity injuries in patients who are unconscious which can lead to bad outcomes. Here, we report a case of successful management of a boy who presented with forearm impalement injury in a rural hospital.
A 7-year-old boy was brought to the emergency following a fall over the metal fence at home which resulted in a penetrating injury to the left forearm. The forearm was impaled with a metal spike of the fence, which had to be detached with a saw to bring the patient to the hospital. The boy presented with a penetrating wound on the left proximal forearm, with a metal rod sticking out of the wound (Fig. 1).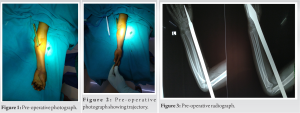 The other end of the rod could be palpated on the dorsum of the hand. The distal pulses were palpable and capillary refill was good, and finger movements were normal although thumb movements were painful. The child had no other injuries, and he was conscious, oriented, and hemodynamically stable. Radiographs of the left forearm with elbow and wrist were ordered to rule out concomitant fracture (Fig. 2), and complete blood counts were sent and were within normal limits. The patient was taken up in the operating room under general anesthesia. The entry wound in the proximal volar aspect of forearm was extended (Fig. 3). Distal incision was given over the palpable end of the rod in the dorsum of hand over the 1st web space (Fig. 4). The rod was found to have traversed in the subcutaneous plane with no obvious injury to the flexor muscle bellies or the tendons in the forearm. The rod was carefully freed off of the soft tissues and the rod was extracted by gentle pull from the distal wound (Fig. 5). Post-removal the wounds were explored for any tendon injury and none was found, radiographs were done under the image intensifier, and any bony injury was ruled out. Copious saline irrigation was done and the wounds were closed in layers over a drain. Broad-spectrum antibiotics which were started pre-operatively were continued post-operatively for 5 days. Suture line dressings were done on the 2nd and 4th days and the sutures were removed on the 14th day. There were no signs of infection or any neurovascular deficit till 2-month follow-up.
The other end of the rod could be palpated on the dorsum of the hand. The distal pulses were palpable and capillary refill was good, and finger movements were normal although thumb movements were painful. The child had no other injuries, and he was conscious, oriented, and hemodynamically stable. Radiographs of the left forearm with elbow and wrist were ordered to rule out concomitant fracture (Fig. 2), and complete blood counts were sent and were within normal limits. The patient was taken up in the operating room under general anesthesia. The entry wound in the proximal volar aspect of forearm was extended (Fig. 3). Distal incision was given over the palpable end of the rod in the dorsum of hand over the 1st web space (Fig. 4). The rod was found to have traversed in the subcutaneous plane with no obvious injury to the flexor muscle bellies or the tendons in the forearm. The rod was carefully freed off of the soft tissues and the rod was extracted by gentle pull from the distal wound (Fig. 5). Post-removal the wounds were explored for any tendon injury and none was found, radiographs were done under the image intensifier, and any bony injury was ruled out. Copious saline irrigation was done and the wounds were closed in layers over a drain. Broad-spectrum antibiotics which were started pre-operatively were continued post-operatively for 5 days. Suture line dressings were done on the 2nd and 4th days and the sutures were removed on the 14th day. There were no signs of infection or any neurovascular deficit till 2-month follow-up.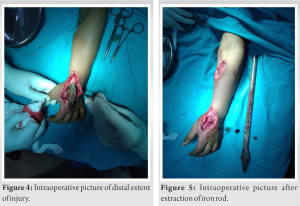
Impalement injuries are relatively rare as compared to other traumatic injuries presenting to the emergency room. Ketterhagen and Wassermann [1] were among the first to publish their management of two impalement injuries, one being a thigh impalement and another being a thoracoabdominal impalement. Horowitz et al. [2] presented successful management of trunk impalement by iron rod. Complex impalement injuries trap the patient and interfere with transport to hospital, and such injuries are common during natural disasters such as earthquakes. At times, the metal rod or penetrating object has to be cut with a saw to facilitate transfer to the hospital the same was done in the case described here. In any case, the trial of removal of the penetrating object should not be undertaken outside the operating room as it may aggravate hemorrhage by removing tamponade effect and can cause injury to neurovascular structures. Once at the hospital, thorough evaluation should be done and initial resuscitation should be done, in case of active bleeding or blood loss, which may need resuscitation with bolus of crystalloids. In case of thoracoabdominal injuries, it is uniformly agreed that in patients unstable after initial resuscitation, it is prudent to shift for an exploratory surgery rather than waste time on radiological investigations [3,4,9]. However, in stable patients, it is best to do radiological investigations before surgery, especially in patients with extremity injuries to rule out concomitant fractures. Patient positioning in the operating room is dictated by the nature and trajectory of the foreign object and the part of the body involved [1,2,7]. In the case presented above, the patient was under general anesthesia in the supine position with the affected forearm on the hand table and a tourniquet was used. Surgical exposure should take into account the entry, exit, and trajectory of the impaling object [1,2,5], and also, it should allow exploration of the tract and allow direct removal of the object under vision [1,2,4,7,8]. Ketterhagen and Wasserman [1] recommended a fistulotomy type of incision connecting entry and exit points carried down to the object. However, according to Bajaj et al. [6], it is not necessary to lay open the tract taken by impaling object in every case; irrigating the wound with normal saline by introducing a catheter in the tract is sufficient. All the devitalized tissues and foreign body and metallic debris need to be thoroughly debrided along with freshening of skin margins and the wound should be thoroughly irrigated with normal saline [1,2,5,7]. et al. [6] stressed the need to individualize management in every case when they presented a series of four cases of such injuries. et al. [7] studied a series of impalement injuries three of them involved extremities. Since then, many authors have reported individual experiences with extremity impalement in the form of case reports discussing principles of management. et al. [8] described their experience while managing a thigh impalement injury. et al. [10] described an interesting case of unusual knee impalement injury. Early administration of broad-spectrum antibiotics covering both aerobic and anaerobic organisms as soon as possible preferably in the emergency room is of utmost importance [1,2,5,11]. Most of the impalement injuries are field injuries with a metallic rod, most commonly iron rods, along with further contamination with soil, hence routine tetanus prophylaxis according guidelines and patient’s immunization status [12]. Regular follow is required to detect any early or delayed infections [2,8,11], and patients should also be made aware of delayed infections in cases of gross contamination. In the case presented above, the operative wound healed without any post-operative complications and was asymptomatic till his 6-month follow-up.
Impalement injuries ideally require a multidisciplinary approach. Management of each case needs to be individualized based on the nature of the injury. Thorough wound exploration, effective debridement, copious irrigation with normal saline, and good antibiotic coverage are needed to successfully tackle these rare yet severe injuries.
Impalement injuries to limbs warrant a thorough neurovascular examination which may in turn be suboptimal due to the severe pain and the pressure effects of the foreign object. Adequate surgical exposure to allow extraction under direct vision with a good debridement and copious irrigation and good antibiotic coverage is essential for good post-operative outcomes.
References
- 1.Ketterhagen JP, Wassermann DH. Impalement injuries: The preferred approach. J Trauma 1983;23:258-9. [Google Scholar | PubMed]
- 2.Horowitz MD, Dove DB, Eismont FJ, Green BA. Impalement injuries. J Trauma 1985;25:914-6. [Google Scholar | PubMed]
- 3.Shikata H, Tsuchishima S, Sakamoto S, Nagayoshi Y, Shono S, Nishizawa H, et al. Recovery of an impalement and transfixion chest injury by a reinforced steel bar. Ann Thorac Cardiovasc Surg 2001;7:304-6. [Google Scholar | PubMed]
- 4.Oya S, Miyata K, Yuasa N, Takeuchi E, Goto Y, Miyake H, et al. Impalement injury to the left buttock with massive bleeding: A case report. Nagoya J Med Sci 2013;75:147-52. [Google Scholar | PubMed]
- 5.Naito K, Obayashi O, Mogami A, Han C, Kaneko K. Impalement injury of the pelvis due to car brake pedal. Injury Extra 2008;39:11-3. [Google Scholar | PubMed]
- 6.Bajaj HN, Rao PS, Kumar B. Impalement injuries. Arch Orthop Trauma Surg 1989;108:58-9. [Google Scholar | PubMed]
- 7.Kelly IP, Attwood SE, Quilan W, Fox MJ. The management of impalement injury. Injury 1995;26:191-3. [Google Scholar | PubMed]
- 8.Banshelkikar SN, Sheth BA, Dhake RP, Goregaonkar AB. Impalement injury to thigh: A case report with review of literature. J Orthop Case Rep 2018;8:71-4. [Google Scholar | PubMed]
- 9.Malla G, Basnet B, Vohra R, Herrforth C, Adhikari S, Bhandari A. Thoraco- abdominal impalement injury: A case report. BMC Emerg Med 2014;14:7. [Google Scholar | PubMed]
- 10.Kodidasu HA, Murugan AK, Siddanathi CS, Patnala AK. An unusual impalement injury to knee. J NTR Univ Health Sci 2020;9:201-4. [Google Scholar | PubMed]
- 11.Alani M, Mahmood S, El-Menyar A, Atique S, Al-Thani H, Peralta R. An unusual case of transpelvic impalement injury: A case-report. Int J Surg Case Rep 2017;41:26-9. [Google Scholar | PubMed]
- 12.Center for Disease Control and Prevention Guidelines. Available from: https://www.cdc.gov/tetanus/clinicians.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fdisasters%2Fdisease%2Ftetanus.html. Last accessed on 22-09-2023. [Google Scholar | PubMed]






