Trans-sacral Epiduroscopic Laser Decompression(SELD) is safe, precise, less invasive, and effective in the treatment of symptomatic lumbar lesions.
Dr. Rajendra Sakhrekar Yonsei Okay Hospital, Seoul, South Korea Email: raj.sakhrekar1@gmail.com
Introduction: The concept of sacral epiduroscopic laser decompression (SELD) is based on the introduction of a steerable catheter in the sacral hiatus followed by the insertion of a fiberoptic laser system into the ventral side of the epidural disc space with an epiduroscope. This procedure enables the direct decompression of the ruptured annulus as the laser vaporizes the bulging disc in the herniated part, cauterization of the sinuvertebral nerve, adhesiolysis of structures nearby the nerve root, and irrigation of inflammation with saline and steroids.
Case Report: A 44-year-old man presented to the outpatient department with a 12-month history of low back pain. His back pain had increased progressively. At the time of presentation, his back pain VAS score was 7/10 and his ODI score was 44. He had received non-steroidal anti-inflammatories for more than 6 months and an epidural injection elsewhere with minimal relief from symptoms. On physical examination, power in the lower limbs was 5/5 as per the MRC grading, and deep tendon reflexes were normal.
Conclusion: The procedure is a useful technique in treating lumbar disc herniation with rapid pain relief and improvements in functional outcomes without any injury to paraspinal muscles or any resection of the ligaments and bony structures. SELD is safe, precise, and effective in the treatment of symptomatic lumbar lesions. Improvements in the optics and visuals with advancements in lasers’ ability to ablate tissue could be beneficial. Large, randomized, and multicenter trials are needed to further explore the potential of SELD.
Keywords: Trans-sacral epiduroscopic decompression, Ho: YAG laser, lumbar back pain, minimally invasive, VAS score
Epiduroscopy received approval from the United States Food and Drug Administration in 1996, which led to the development of the current trans-sacral epiduroscopic laser decompression (SELD) technique to diagnose and treat various lumbosacral spine pathologies [1]. The concept of SELD is based on the introduction of a steerable catheter in the sacral hiatus, followed by the insertion of a fiberoptic laser system into the ventral side of the epidural disc space with an epiduroscope. This procedure enables the direct decompression of the ruptured annulus as the laser vaporizes the bulging disc in the herniated part, cauterization of the sinuvertebral nerve, adhesiolysis of structures nearby the nerve root, and irrigation of inflammation with saline and steroids [1, 2, 3, 4, 5]. Literature about the SELD procedure is scarce, with limited studies demonstrating positive clinical and radiological outcomes with good safety in patients with lower back pain and radicular leg pain due to lumbar disc herniation [6, 7, 8, 2, 9, 10]. This study reports the case of an annular tear with disc herniation in a 44-year-old male with a 2-year follow-up successfully treated with SELD and a technical note.
A 44-year-old man presented to the outpatient department with a 12-month history of low back pain. His back pain had increased progressively. At the time of presentation, his back pain VAS score was 7/10 and his ODI score was 44. He had received non-steroidal anti-inflammatories for more than 6 months and an epidural injection elsewhere with minimal relief from symptoms. On physical examination, power in the lower limbs was 5/5 as per the MRC grading, and deep tendon reflexes were normal too. The past, personal, addiction, or familial history was not significant. The magnetic resonance (MR) images showed a single fluid-containing lesion with a hyperintense zone at the L4–5 levels (Fig. 1). After adequate counselling with an explanation of the pros and cons of the procedure and its probable complications, the informed consent of the patient was taken, and the patient was planned for the SELD procedure.
Technical note
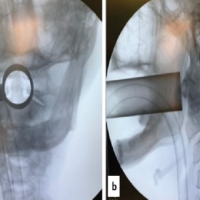
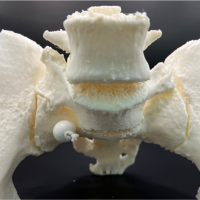
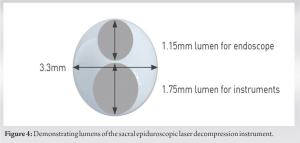
The procedure is performed under local anesthesia using lidocaine over the sacral hiatus, with monitored vital signs by an anesthesiologist. The patient was awake throughout the procedure and conversed with the team, giving input about the pain responses. The patient was positioned in the prone position on a radiolucent table with Wilson’s frame (Fig. 2). The Wilson frame helps to decrease lumbosacral lordosis and intra-abdominal pressure. Two vertical foam bolsters can also be used if the Wilson frame is not available. A 5 mm small skin incision was made on the sacral hiatus with a stabbing knife. A trocar is used under fluoroscopic guidance to puncture the sacrococcygeal ligament, the trocar was advanced to the S2-3 level, then a video-guided catheter of 3.3 mm in diameter (Myelotec) containing two lumens (1.15 mm lumen for the epiduroscope and 1.75 for the instruments) was inserted through the trocar into the sacrococcygeal ventral epidural space (Fig. 3 and 4). 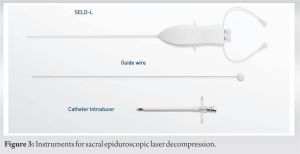
 Verification of the position of the catheter in the ventral epidural space is of the highest importance (Fig. 5), and a C-arm fluoroscope with image intensification should be used to provide images in both the anterior/posterior and lateral planes (Fig. 6).
Verification of the position of the catheter in the ventral epidural space is of the highest importance (Fig. 5), and a C-arm fluoroscope with image intensification should be used to provide images in both the anterior/posterior and lateral planes (Fig. 6).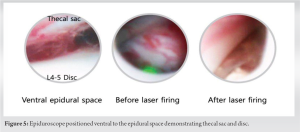 Through the video-guided catheter, an epiduroscope and the Ho: YAG laser were advanced into the end of the catheter to visualize the epidural space and perform cauterization of the sinuvertebral nerve, adhesiolysis of nearby the nerve roots, and irrigation of inflammation. The Ho: YAG laser is of high quality in the ablation of the disc, and it also does not cause significant thermal injury to the neural structures as compared to other lasers. Continuous, slow, and smooth irrigation with cool saline also helps visualization of the anatomical structures and helps prevent thermal damage to the nerves. Irrigation also helps reduce bleeding by its hydrostatic pressure during the procedure. The target area of annulus disc bulge ablation is ideally limited between the posterior longitudinal ligament (PLL) and the posterior annulus to reduce damage to the posterior annulus. Radio-opaque dye was introduced between the dura and bulging PLL with an underlying herniated nucleus pulposus (HNP), which did not cross the pathological L4-5 site due to adhesions and bulging PLL (Fig. 6).
Through the video-guided catheter, an epiduroscope and the Ho: YAG laser were advanced into the end of the catheter to visualize the epidural space and perform cauterization of the sinuvertebral nerve, adhesiolysis of nearby the nerve roots, and irrigation of inflammation. The Ho: YAG laser is of high quality in the ablation of the disc, and it also does not cause significant thermal injury to the neural structures as compared to other lasers. Continuous, slow, and smooth irrigation with cool saline also helps visualization of the anatomical structures and helps prevent thermal damage to the nerves. Irrigation also helps reduce bleeding by its hydrostatic pressure during the procedure. The target area of annulus disc bulge ablation is ideally limited between the posterior longitudinal ligament (PLL) and the posterior annulus to reduce damage to the posterior annulus. Radio-opaque dye was introduced between the dura and bulging PLL with an underlying herniated nucleus pulposus (HNP), which did not cross the pathological L4-5 site due to adhesions and bulging PLL (Fig. 6). 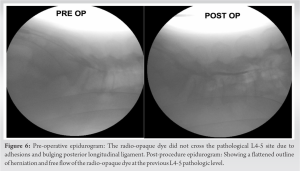 As the surgeon decompressed the disc bulge below the PLL by Ho: YAG laser, the epidural space between the dura and bulging PLL with an underlying HNP became wider and confirmed by a repeat epidurogram showed a flattened outline of herniation and free flow at the previous pathologic level (Fig. 6). Steroid and normal saline irrigation was performed before the incision closure with adhesive glue and sutures were taken.
As the surgeon decompressed the disc bulge below the PLL by Ho: YAG laser, the epidural space between the dura and bulging PLL with an underlying HNP became wider and confirmed by a repeat epidurogram showed a flattened outline of herniation and free flow at the previous pathologic level (Fig. 6). Steroid and normal saline irrigation was performed before the incision closure with adhesive glue and sutures were taken.
Outcome measures:
The patient’s pain and neurological symptoms kept improving on post-procedure days 1, 2 weeks, 1 month, and 6 months. There was a rapid relief of pain on day 1, and VAS improved from 7 to 1. At 6 months of follow-up, the VAS score was 0 and the ODI improved from 50 to 19. These results were maintained at a 2-year follow-up with a telephone conversation. Patient satisfaction was surveyed using Odom’s criteria at each follow-up visit (at 1 week, 1 month, 6 months, and 2 years) and found to be excellent. These cases demonstrated no early or late complications in terms of neurologic deficits, infection, or epidural hematomas.
The use of lasers for removing a small volume of tissue from the disc to reduce intradiscal pressure and the volume of disc herniation was well documented by Ascher and Heppner in 1984 with CO2 and Nd lasers with good clinical outcomes for patients with lumbar back pain [11]. Choy et al. in 1992 first published the novel technique of epiduroscopic neural laser decompression (ENLD) [12]. In 1996, after US FDA approval, the technique and instrumentation of ENLD significantly improved [13, 14, 15, 16]. The advantages of SELD include immediate pain relief, rapid recovery, no paravertebral muscle injury, and no resection of the ligaments and bony structures. As the SELD involves additional effects of the laser ablation of hydrated soft tissue, it is considered more beneficial over conventional drug injection or adhesiolysis procedures like epidural neuroplasty [16, 17]. The currently used Ho: YAG is based on the vaporizing effect to destroy the disc, which is influenced by energy absorption by water [14, 18, 19]. It has the optimal wavelength, which is close to the absorption of water (2000 nm) helping to strongly absorb the water molecules. It has a 350-microsec pulse duration, and it absorbs <0.4 mm of fluid. In SELD, the laser light is transmitted through flexible fibers at the precise pathological site and with its fast-absorbing wavelength of <0.4 mm depth, the hemostatic cutting and ablation of tissue are safer. It is effective with minimal thermal damage to the surrounding neural structures and can be achieved with the least invasive approach. The indications for SELD include mainly mild-to-moderate disc herniation but also include spinal stenosis, adhesion, chronic low back pain, radicular leg pain, failed back syndrome, and cystic lesions in the lumbosacral spine despite adequate conservative treatment [4, 17]. The contraindications for SELD include progressive neurological deficits or cauda equina syndrome or severe motor deficits with motor power Grade 3 or less, a hard calcified disc on imaging, foraminal, or extraforaminal disc herniation, which is difficult to reach using SELD, severe spinal stenosis (Schizas Grade C and D), instability (Meyerding Grade 2 or higher), infection, and anatomical variations of sacral hiatus or peri-dural cyst compromising catheter accessibility [1, 3, 4, 6]. In 2016, Lee et al. reported that in a cohort of 250 patients with lumbar back pain and radiculopathy who had HNP, the VAS score and ODI dramatically improved after SELD. The HNP size and neurological compression were both significantly reduced on post-operative MR imaging (MRI). They concluded that SELD may be a useful therapy approach for people with symptomatic HNP [7]. In 2018, Kim et al. demonstrated ENLD using a Holmium–YAG laser in the treatment of symptomatic benign spinal cysts [4]. In 2020, Son et al. in a study of 82 patients reported that at the final follow-up, the average for low back pain and leg pain as measured by the VAS improved from 5.43 to 1.73 and 6.10 to 1.67, respectively (P = 0.001). At the last follow-up of 6 months, the success rate was defined as excellent or good in 58.5% of patients by Odom’s standards. They concluded that their results were less favorable as compared to previous studies and mentioned several reasons for this variation in clinical outcomes, including a learning curve and baseline influencing factors on outcomes and suggested further study with a larger cohort [1]. This study has some limitations in terms of the SELD technique. The technique’s major drawbacks include the restricted epiduroscopic field of view and poor picture quality in the constrained epidural space, which occasionally reduce visibility and restrict the end-firing laser’s ability to ablate soft tissue [7]. In the future, epiduroscopy will need improvements in picture quality to a high definition and a wide optic angle to address this issue. Second, since the herniated disc cannot be entirely cauterized, there is a limit to how much volume of the disc can be fired. In the future, the side-firing laser with a more efficient energy source than the disc could be beneficial. As this is a case report and technical note, a small sample size and a short-term follow-up of 2 years are the limitations. As the patient improved clinically considering cost-effectiveness and patient interests, an MRI post-procedure was deemed unnecessary. However, in future studies with long-term follow-up, a larger sample size and an MRI post-procedure to document radiological outcomes could be suggested.
The SELD procedure is a useful technique in treating lumbar disc herniation with rapid pain relief and improvements in functional outcomes without any injury to paraspinal muscles or any resection of the ligaments and bony structures. SELD is safe, precise, and effective in the treatment of symptomatic lumbar lesions. Improvements in the optics and visuals with advancements in lasers’ ability to ablate tissue could be beneficial. Large, randomized, and multicenter trials are needed to further explore the potential of SELD.
Trans-sacral Epiduroscopic Laser Decompression(SELD) is safe, precise, less invasive, and effective in the treatment of symptomatic lumbar lesions.
References
- 1.Son S, Lee SG, Ahn Y, Kim WK. Clinical outcomes of trans-sacral epiduroscopic laser decompression (SELD) in patients with lumbar disc herniation. Pain Res Manag 2020;2020:1537875. [Google Scholar | PubMed]
- 2.Kim SK, Lee SC, Park SW. Trans-sacral epiduroscopic laser decompression versus the microscopic open interlaminar approach for L5-S1 disc herniation. J Spinal Cord Med 2020;43:46-52. [Google Scholar | PubMed]
- 3.Son S, Yoo CJ, Yoo BR, Kim WS, Jeong TS. The learning curve of trans-sacral epiduroscopic laser decompression in herniated lumbar disc disease. BMC Surg 2021;21:39. [Google Scholar | PubMed]
- 4.Kim SK, Lee BH, Song MB, Lee SC. A novel technique for managing symptomatic spinal cysts using epiduroscopic neural laser decompression: technical note and preliminary results. J Orthop Surg Res 2018;13:136. [Google Scholar | PubMed]
- 5.Kim HS, Wu PH, Jang IT. Narrative review of pathophysiology and endoscopic Management of basivertebral and sinuvertebral neuropathy for chronic back pain. J Korean Neurosurg Soc 2023;66:344-5 [Google Scholar | PubMed]
- 6.Yoo BR, Son S, Lee SG, Kim WK, Jung JM. Factors predicting the clinical outcome after trans-sacral epiduroscopic laser decompression for lumbar disc herniation. Neurospine 2021;18:336-43. [Google Scholar | PubMed]
- 7.Lee SH, Lee SH, Lim KT. Trans-sacral epiduroscopic laser decompression for symptomatic lumbar disc herniation: A preliminary case series. Photomed Laser Surg 2016;34:121-9. [Google Scholar | PubMed]
- 8.Oh J, Jo D. Epiduroscopic laser neural decompression as a treatment for migrated lumbar disc herniation: Case series. Medicine (Baltimore) 2018;97:e0291. [Google Scholar | PubMed]
- 9.Kim SK, Lee SC, Park SW, Kim ES. Complications of lumbar disc herniations following trans-sacral epiduroscopic lumbar decompression: A single-center, retrospective study. J Orthop Surg Res 2017;12:187. [Google Scholar | PubMed]
- 10.Moon BJ, Yi S, Ha Y, Kim KN, Yoon DH, Shin DA. Clinical efficacy and safety of trans-sacral epiduroscopic laser decompression compared to percutaneous epidural neuroplasty. Pain Res Manag 2019;2019:2893460. [Google Scholar | PubMed]
- 11.Ascher PW, Heppner F. CO2-Laser in neurosurgery. Neurosurg Rev 1984;7:123-33. [Google Scholar | PubMed]
- 12.Choy DS, Ascher PW, Ranu HS, Saddekni S, Alkaitis D, Liebler W, et al. Percutaneous laser disc decompression. A new therapeutic modality. Spine (Phila Pa 1976) 1992;17:949-56. [Google Scholar | PubMed]
- 13.Shimada S, Tamaki N, Kobe J. Assessment of safety and feasibility of spinal endoscope in the thoracic and lumbar region: A cadaveric study. Kobe J Med Sci 2001;47:263-72. [Google Scholar | PubMed]
- 14.Ruetten S, Meyer O, Godolias G. Application of holmium: YAG laser in epiduroscopy: Extended practicabilities in the treatment of chronic back pain syndrome. J Clin Laser Med Surg 2002;20:203-6. [Google Scholar | PubMed]
- 15.Donato AD, Fontana C, Pinto R, Beltrutti D, Pinto G. The effectiveness of endoscopic epidurolysis in treatment of degenerative chronic low back pain: A prospective analysis and follow-up at 48 months. Acta Neurochir Suppl 2011;108:67-73. [Google Scholar | PubMed]
- 16.Jo DH, Kim ED, Oh HJ. The comparison of the result of epiduroscopic laser neural decompression between FBSS or not. Korean J Pain 2014;27:63-7 [Google Scholar | PubMed]
- 17.Ceylan A, Aşık İ, Özgencil GE, Erken B. Evaluation of the efficacy of epiduroscopic adhesiolysis in failed back surgery syndrome. Turk J Med Sci 2019;49:249-57. [Google Scholar | PubMed]
- 18.Jo D, Lee DJ. The extent of tissue damage in the epidural space by Ho/YAG laser during epiduroscopic laser neural decompression. Pain Physician 2016;19:E209-14 [Google Scholar | PubMed]
- 19.Lee GW, Jang SJ, Kim JD. The efficacy of epiduroscopic neural decompression with Ho: YAG laser ablation in lumbar spinal stenosis. Eur J Orthop Surg Traumatol 2014;24:S231-7. [Google Scholar | PubMed]