The interposition of cement can cause the disengagement of components of a humeral stem and its respective tray when it expands.
Dr. Rodrigo Brandariz, Shoulder and Elbow Center - Hirslanden Clinique la Colline, Geneva, Switzerland. E-mail: rodrigobrandariz@gmail.com
Introduction: Reverse shoulder arthroplasty (RSA) complication rates range between 1.4% and 28% depending on the nature of the indication. Even though glenosphere dissociation is the third most frequent complication after RSA, with an incidence that can rise to just over 12%, there is no evidence in the literature describing the disassembly between the humeral stem and its metaphysics.
Case Report: It is reported a novel early failure type in a reversed shoulder arthroplasty of a healthy 72-year-old female patient, involving the disassembly of the metaphysis from an onlay tray system due to cement interposition in a reversed shoulder prosthesis.
Conclusion: This case highlights a rare form of early failure after RSA as a result of a disassembly between the humeral stem and its metaphysis due to the presence of interposed cement. To prevent this complication, a two-step implantation procedure is recommended, which consists of cementing the stem before inserting the metaphyseal tray.
Keywords: Reverse shoulder arthroplasty, components disassembly, early failure, complication.
Reverse shoulder arthroplasty (RSA) has become a state-of-the-art procedure to treat several shoulder pathologies. Indeed, its indications have been proliferating during the past 10 years compared to other designs such as anatomic or hemiarthroplasty [1,2,3]. It is projected that the prevalence of shoulder arthroplasty by 2025 is likely to vary between 67% and 235% depending on the modeling predictor [4]. Even though the latest prosthetic designs have tended to enhance outcomes and reduce the rate of complications, it is inevitable that new types of complications than those currently known will emerge with the exponential increase in the number of implanted prostheses, and more than 200 different designs, new types of complications than those currently known will emerge [1,5]. RSA complication rates range between 1.4% and 28% depending on the nature of the indication. Rheumatoid arthritis was reported to be the pathology with the most significant ratio of complications and osteoarthritis the least [6]. Some of the complications described are scapular notching, acromion fracture, instability, infection, and loosening among others. In addition, the disassembly of the prosthesis components has many literature reports [7,8]. Glenosphere dissociation is the third most frequent complication after RSA, with an incidence that can rise to just over 12% [6,9,10]. This complication has not been exclusive to one type of prosthesis but has been described with different designs, from those with a centrally threaded screw for glenosphere fixation to those which solely rely on morse taper. It has been suggested that several causes could lead to a morse taper not fitting correctly between the baseplate and glenosphere components, such as not reaming the glenoid properly, the baseplate screws not being seated correctly, the implant design, and the presence of soft tissues interfering. However, even though humeral stems typically also engage their respective metaphysis with a morse taper, there is no evidence in the literature describing the disassembly of these two components in the post-operative period. Therefore, this article aims to report a novel early failure type in RSA, involving the disassembly of the metaphysis from an onlay tray system due to cement interposition in reversed shoulder prosthesis.
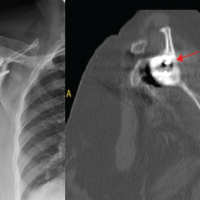
A 72-year-old female patient with a prior history of right shoulder acromioplasty and otherwise healthy underwent a right RSA for cuff tear arthropathy in May 2019 by a senior shoulder specialist surgeon, using an onlay tray stem system (Aequalis Ascend Flex, Wright Medical Group, Memphis, TN, USA). A deltopectoral approach with subscapularis tenotomy was carried out in accordance with standard protocol. A size 4 humeral stem was coupled to a low-eccentricity size 0 metaphyseal tray before the implantation. Because of poor bone quality, the stem was cemented with a half-dose of Palacos® (Zimmer Biomet, Warsaw, IN, USA), using a third-generation technique. After the implantation and the setting of the cement, a standard liner was placed, and the prosthesis was reduced. It was found to be stable, and the subscapularis tendon was reattached using transosseous sutures, thereby enabling the successful completion of the procedure. Following the surgery, the initial recovery period was uneventful. The arm was secured in a sling at an internal rotation for 6 weeks. Passive range of motion was permitted with the aid of physical therapy for the initial 6 weeks, which was then followed by active range of motion and muscle strengthening. At the 6-month follow-up, the patient reported 80% of satisfaction and scored 3 in visual analog scale. Shoulder range of motion was measured as 150° of elevation and abduction, 20° of external rotation, and internal rotation to the L5 level. Radiographic control was also consistent with the found outcomes (Fig. 1). One month after, because of sudden onset of pain and loss of shoulder function in the absence of any history of trauma or fever and chills, the patient returned for a follow-up visit. Objective findings on physical examination included maximal elevation and abduction of the arm at 90°, 10° external rotation, and internal rotation to the buttock. Passive range of motion was limited and associated with pain. Radiological imaging demonstrated a rotation of the metaphyseal plateau around the stem (Fig. 2).
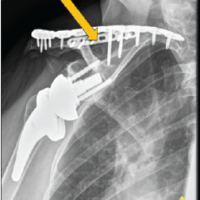
One month after, because of sudden onset of pain and loss of shoulder function in the absence of any history of trauma or fever and chills, the patient returned for a follow-up visit. Objective findings on physical examination included maximal elevation and abduction of the arm at 90°, 10° external rotation, and internal rotation to the buttock. Passive range of motion was limited and associated with pain. Radiological imaging demonstrated a rotation of the metaphyseal plateau around the stem (Fig. 2).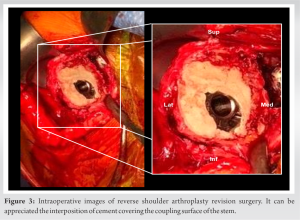 The patient was brought back to the operating room for a revision, using the same deltopectoral approach. Subsequently, culture samples were collected for bacteriological analysis as a standard precautionary measure, which ultimately resulted in a negative report after an extended culture period. During the inspection, it was detected an interposition of cement backflow between the tray and the stem which had expanded and decoupled the taper bond (Fig. 3). The cement interface was meticulously removed using an osteotome, the metaphysis was reamed, the stem was well fixed and retained, and a new tray and polyethylene liner of the same size were impacted. The remaining steps of the procedure were carried out according to standard care, and rehabilitation was resumed. At the 18-month follow-up, the patient reported sustained satisfaction, although she experienced occasional pain with end-range movements. Abduction and elevation were 160°, external rotation 40°, and internal rotation to L5. Radiological evaluation revealed no signs of loosening or disassembly.
The patient was brought back to the operating room for a revision, using the same deltopectoral approach. Subsequently, culture samples were collected for bacteriological analysis as a standard precautionary measure, which ultimately resulted in a negative report after an extended culture period. During the inspection, it was detected an interposition of cement backflow between the tray and the stem which had expanded and decoupled the taper bond (Fig. 3). The cement interface was meticulously removed using an osteotome, the metaphysis was reamed, the stem was well fixed and retained, and a new tray and polyethylene liner of the same size were impacted. The remaining steps of the procedure were carried out according to standard care, and rehabilitation was resumed. At the 18-month follow-up, the patient reported sustained satisfaction, although she experienced occasional pain with end-range movements. Abduction and elevation were 160°, external rotation 40°, and internal rotation to L5. Radiological evaluation revealed no signs of loosening or disassembly.
This study documents a previously unreported early type of failure after RSA, involving the disassembly of the metaphysis from an onlay tray system due to the interposition of cement, which was identified only 7-month post-implantation. The emergence of modular prostheses has highlighted the need to investigate the uncoupling of their components, as this may lead to a sudden change in biomechanical functionality and consequent functional deterioration. Regarding RSA, the reports in the literature mention only the disassembly between the glenosphere and its metaglene as an example of this complication, which is the third most frequently reported complication, rising up to 12%. The possible causes of its entity may be due to an inadequate glenoid reaming, a baseplate with not well-seated screws not being, the implant design, and the presence of soft-tissues interfering. Taking into account the similarities in the coupling methods between the humeral stem and its metaphysis with the metaglene and its glenosphere, decoupling could potentially occur due to the same reasons previously outlined. Nonetheless, to date, we have not found records in the literature that describe this complication. The likelihood of a low rate of incidence of this complication may be a result of the combined influence of multiple factors, not only during the operation but also in the short, medium, and long postoperative term. First, the deltopectoral approach allows better exposure of the humerus than the glenoid, and any interposition of soft tissue can be better controlled visually. Second, due to the biomechanics of the RSA, the load applied to the glenoid components is significantly higher than to the humeral’s counterparts [11]. Indeed, it has been observed in several studies that variations in the design of the baseplate fixation, such as the length of the central peg and the lower bone density at the positions of the screws, could potentially lead to micromotion and eventual loosening of these components [12,13,14]. Finally, and related to the previous factors, the incidence of radiographic changes such as loosening is significantly higher on the glenoid than on the humeral side. Some reports mention up to 96% loss of bone stock associated with the glenoid component, while others have <3% radiographic lucencies associated with the humeral component. Consequently, the prosthetic loosening of one of the components could cause greater movement between the coupling surface and possible subsequent disengagement [15,16,17]. Regarding the cause of the humeral metaphysis disassembly presented in this case report; the identified cause was the interposition of cement between the humeral stem and its metaphysis during implantation, which expanded during the setting phase, generating enough pressure to disassemble the morse taper junction. A similar complication has been reported in knee prostheses where the cement interposition generated mismatches between the liner and the tibial plateau [18,19,20]. However, unlike knee prostheses which can limit the visibility of cement fragments on the posterior surface, the base of the humeral stem is directly visible when impacting the metaphysics, making it difficult to avoid recognizing that cement is interposed. Analysis of the previous studies has indicated that the use of cementless fixation of humeral components in RSA may be preferable to cement fixation, as it carries a reduced risk of complications arising from the treatment of rotator cuff arthropathy [21]. Therefore, avoiding the use of cement whenever possible when using this type of implant is therefore recommended, and if required because of poor bone quality, it is recommended that the humeral stem should be placed first, and once the cement has set, the humeral tray may be impacted.
This case highlights a rare form of early failure after RSA as a result of a disassembly between the humeral stem and its metaphysis due to the presence of interposed cement. To prevent this complication, a two-step implantation procedure is recommended, which consists of cementing the stem before inserting the metaphyseal tray.
To prevent a cement interposition between the humeral stem and its humeral trail in an RSA, a two-step implantation procedure is recommended, which consists in cementing the stem before inserting the metaphyseal tray.
References
- 1.Kozak T, Bauer S, Walch G, Al-Karawi S, Blakeney W. An update on reverse total shoulder arthroplasty: Current indications, new designs, same old problems. EFORT Open Rev 2021;6:189-201. [Google Scholar | PubMed]
- 2.Dines DM. 5 Emerging Indications for Reverse Total Shoulder Arthroplasty. Reverse Shoulder Arthroplasty; 2017. [Google Scholar | PubMed]
- 3.Morrey BF. Increasing incidence of shoulder arthroplasty in the United States. In: Yearbook of Orthopedics. United States: Mosby; 2012. p. 221-2. [Google Scholar | PubMed]
- 4.Wagner ER, Farley KX, Higgins I, Wilson JM, Daly CA, Gottschalk MB. The incidence of shoulder arthroplasty: Rise and future projections compared with hip and knee arthroplasty. J Shoulder Elbow Surg 2020;29:2601-9. [Google Scholar | PubMed]
- 5.Frank JK, Siegert P, Plachel F, Heuberer PR, Huber S, Schanda JE. The evolution of reverse total shoulder arthroplasty-from the first steps to novel implant designs and surgical techniques. J Clin Med Res 2022;11:1512. [Google Scholar | PubMed]
- 6.Kennedy J, Klifto CS, Ledbetter L, Bullock GS. Reverse total shoulder arthroplasty clinical and patient-reported outcomes and complications stratified by preoperative diagnosis: A systematic review. J Shoulder Elbow Surg 2021;30:929-41. [Google Scholar | PubMed]
- 7.MacAskill ML, Thomas RJ, Barnes LA. Case report: Watching and waiting? A case of incomplete glenosphere seating with spontaneous reversal in reverse shoulder arthroplasty. J Shoulder Elb Arthroplast 2020;4:2471549220949147. [Google Scholar | PubMed]
- 8.Casagrande D, Harmsen S, Norris TR. Glenosphere and baseplate failure in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2016;25:e181-2. [Google Scholar | PubMed]
- 9.Somerson JS, Hsu JE, Neradilek MB, Matsen FA. Analysis of 4063 complications of shoulder arthroplasty reported to the US Food and Drug Administration from 2012 to 2016. J Shoulder Elbow Surg 2018;27:1978-86. [Google Scholar | PubMed]
- 10.Barco R, Savvidou OD, Sperling JW, Sanchez-Sotelo J, Cofield RH. Complications in reverse shoulder arthroplasty. EFORT Open Rev 2016;1:72-80. [Google Scholar | PubMed]
- 11.Cogan CJ, Ho JC, Entezari V, Iannotti JP, Ricchetti ET. The influence of reverse total shoulder arthroplasty implant design on biomechanics. Curr Rev Musculoskelet Med 2023;16:95-102. [Google Scholar | PubMed]
- 12.Lung TS, Cruickshank D, Grant HJ, Rainbow MJ, Bryant TJ, Bicknell RT. Factors contributing to glenoid baseplate micromotion in reverse shoulder arthroplasty: A biomechanical study. J Shoulder Elbow Surg 2019;28:648-53. [Google Scholar | PubMed]
- 13.Irlenbusch U, Kohut G. Evaluation of a new baseplate in reverse total shoulder arthroplasty-comparison of biomechanical testing of stability with roentgenological follow up criteria. Orthop Traumatol Surg Res 2015;101:185-90. [Google Scholar | PubMed]
- 14.Frankle M, Marberry S, Pupello D. Reverse Shoulder Arthroplasty: Biomechanics, Clinical Techniques, and Current Technologies. Germany: Springer; 2015. p. 486. [Google Scholar | PubMed]
- 15.Brolin TJ, Cox RM, Horneff JG, Namdari S, Abboud JA, Nicholson K, et al. Humeral-sided radiographic changes following reverse total shoulder arthroplasty. Arch Bone Jt Surg 2020;8:50-7. [Google Scholar | PubMed]
- 16.Lo EY, Rizkalla J, Montemaggi P, Majekodunmi T, Krishnan SG. Clinical and radiographic outcomes of cementless reverse total shoulder arthroplasty for proximal humeral fractures. J Shoulder Elbow Surg 2021;30:1949-56. [Google Scholar | PubMed]
- 17.Pinkas D, Carpenter S, Wiater JM. Reverse shoulder arthroplasty in the setting of proximal humeral bone loss. Reverse Shoulder Arthroplasty 2016;1:213-8 [Google Scholar | PubMed]
- 18.Chen CE, Juhn RJ, Ko JY. Dissociation of polyethylene insert from the tibial baseplate following revision total knee arthroplasty. J Arthroplasty 2011;26:339.e11-3. [Google Scholar | PubMed]
- 19.Ay GR, Rajan DS, Chiranjeevi T, Karthik C, Kiran EK. Failure of polyethelene insert locking mechanism after a posterior stabilised total knee arthroplasty-a case report. J Orthop Case Rep 2016;6:35-7. [Google Scholar | PubMed]
- 20.Jindal S, Bansal V, Ahmed M. Disengagement of tibial insert locking pin in total knee arthroplasty-a rare failure case report. J Clin Orthop Trauma 2022;33:101996. [Google Scholar | PubMed]
- 21.Phadnis J, Huang T, Watts A, Krishnan J, Bain GI. Cemented or cementless humeral fixation in reverse total shoulder arthroplasty? Bone Joint J 2016;98-B:65-74. [Google Scholar | PubMed]