Patellar tumors, usually presenting as anterior knee pain, are rare, with giant cell tumors (GCTs) being the most common, with treatment encompassing salvage in Campanacci grade 1 and patellectomy in Campanacci grades 2 and 3.
Dr. Indrakshi Basak, Department of Pathology, Apollo Gleneagles Hospital, Kolkata, West Bengal, India. Email: indrakshibasak12@gmail.com
Introduction: Primary bone tumors of the patella are rare, with an incidence as low as 0.12%. The majority are benign, with giant cell tumors (GCT) being the predominant tumor affecting this sesamoid bone. An associated secondary aneurysmal bone cyst (ABC) component with a primary patellar GCT is rarely seen.
Case Report: We report a case of a 20-year-old male with long-standing anterior knee pain for 9 months. Having visited multiple clinics and found no relief, the patient presented to us at our out-patient department. Clinical examination suggested patellar tenderness, and knee radiographs showed a lytic lesion with cortical erosions. Computed tomography and magnetic resonance imaging were suggestive of GCT. A patellectomy with a good extensor repair was performed. A patellar biopsy revealed a mixed picture of a primary GCT with a secondary ABC. The patient was closely followed up, and at 12 months, he recovered completely and recorded an excellent functional outcome.
Conclusion: With the incidence of bone tumors on the rise, one should be aware of this relatively rare cause of anterior knee pain. A simple radiograph will help in early diagnosis and will go a long way toward better salvage procedures than more radical procedures like patellectomy.
Keywords: Patella tumors, giant cell tumor, anterior knee pain.
Primary tumors of the patella are rare and typically affect young adults, often presenting as non-specific knee pain [1,2]. With an incidence as low as 0.12% [3], necessary awareness is required to avoid missing these tumors. Giant cell tumors (GCTs) have an incidence of 33%, whereas aneurysmal bone cysts (ABCs) account for 5% of all patellar tumors [1]. However the occurrence of a symbiotic tumor where both these components coexist is relatively rare [4], with only a handful of cases reported to date. The presenting symptoms are usually chronic knee pain with occasional swelling of a non-traumatic origin in young individuals, which is not intensively investigated and is often treated with analgesics or reassurance, citing over-exertional physical activity as the predisposing cause [5,6]. Patellar tumors are not frequently included in the differentials for anterior knee pain, and this often leads to missing these tumors in the early stages [7]. As a result, patients often present late, wherein salvage becomes challenging.
We report a case of a young male in his early twenties who presented to us with long-standing anterior knee pain, the incidental diagnosis of a patellar tumor, and how it was missed at the initial presentation. We have highlighted the challenges in decision-making regarding the treatment strategy, conducted a detailed analysis of the literature, and drawn a reasonable consensus regarding the treatment of these relatively rare tumors.
A young male in his early twenties, a university student, presented to the outpatient department with pain over the right knee for the last 9 months. The pain was continuous in nature, throbbing in character, aggravated when walking, and increased in intensity at night. He had no history of trauma, and he denied any contact injures as well. He had visited multiple clinics before, where he was given analgesics for the unrelenting pain but found only temporary relief. The pain had stopped him from participating in any recreational activities over the past few months. On clinical examination, the patient had localized tenderness over the anterior aspect of the patella. The patellar grind test was positive. He had a good range of motion, with a painful arc ranging from 40° to 120° of flexion. There was no swelling around the knee. There was no distal neurovascular deficit. A plain radiograph of the affected knee was obtained. X-rays revealed a lytic lesion of the patella with cortical erosions. The geographic destruction was appreciated with a doubtful pathological fracture line on the lateral view of the knee x-rays (Fig. 1).  GCT was considered the closest differential due to classical radiologic features and was graded as Campanacci grade 2. A computed Tomography scan was done to see the extent of cortical involvement. Gross cortical erosions were noted on the inferior articular surface, with thinning on certain cuts. The non-articulating superior surface had minor cortical thinning. Magnetic resonance imaging (MRI) was mandatory to rule out any soft tissue involvement (Fig. 2). We confirmed our diagnosis with a core needle biopsy, which suggested it to be a GCT. A total patellectomy and extensor repair were done using 5-0 Ethibond non-absorbable sutures in a purse string fashion (Fig. 3).
GCT was considered the closest differential due to classical radiologic features and was graded as Campanacci grade 2. A computed Tomography scan was done to see the extent of cortical involvement. Gross cortical erosions were noted on the inferior articular surface, with thinning on certain cuts. The non-articulating superior surface had minor cortical thinning. Magnetic resonance imaging (MRI) was mandatory to rule out any soft tissue involvement (Fig. 2). We confirmed our diagnosis with a core needle biopsy, which suggested it to be a GCT. A total patellectomy and extensor repair were done using 5-0 Ethibond non-absorbable sutures in a purse string fashion (Fig. 3). 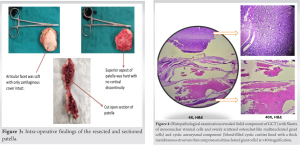 Intra-operatively, the articular surface of the patella was soft and friable, with an intact cartilage cover. The patella was sectioned into two and sent for histopathological examination (HPE). HPE revealed a mixed picture of GCT with secondary ABC (Fig. 4). Post-operatively, the knee was immobilized in a long knee brace for 2 weeks. Passive range of motion at the knee was started at 3 weeks. Active movements were allowed at 6 weeks, and full weight bearing was given at 8 weeks. The patient was on close follow-up over a span of 12 months. Initial post-operative follow-up was at regular intervals till stitch off. The patient was asked to report at 2-month interval thereafter. On follow-up at 12 months, he had a good range of motion at the knee, movements were pain-free, and he was ambulating without any support (Fig. 5). Sequential knee and chest x-rays were recorded every 4 months. At 12 months, an MRI of the knee was done to rule out the recurrence of the tumor.
Intra-operatively, the articular surface of the patella was soft and friable, with an intact cartilage cover. The patella was sectioned into two and sent for histopathological examination (HPE). HPE revealed a mixed picture of GCT with secondary ABC (Fig. 4). Post-operatively, the knee was immobilized in a long knee brace for 2 weeks. Passive range of motion at the knee was started at 3 weeks. Active movements were allowed at 6 weeks, and full weight bearing was given at 8 weeks. The patient was on close follow-up over a span of 12 months. Initial post-operative follow-up was at regular intervals till stitch off. The patient was asked to report at 2-month interval thereafter. On follow-up at 12 months, he had a good range of motion at the knee, movements were pain-free, and he was ambulating without any support (Fig. 5). Sequential knee and chest x-rays were recorded every 4 months. At 12 months, an MRI of the knee was done to rule out the recurrence of the tumor.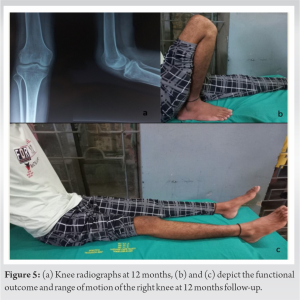
Primary tumors of the patella represent a rare group of bony tumors with an uncommon etiology of knee pain [1]. Symptoms such as joint erythema, pain and swelling, and tenderness on palpation should be closely looked into, and this will help prevent such tumors at initial presentation [8]. A casual physician approach concerned with symptomatic relief and pain management instead of visualizing the other aspects of pain is a strong reason why these tumors are often missed [2]. A similar scenario was seen with our patient, who consulted multiple clinics over the span of 9 months. He was prescribed analgesics and was advised to rest for his chronic knee pain. The first knee radiograph was done when the patient presented to us, and we identified a lytic lesion involving the entire patella. GCT continues to be the most common among the patellar tumors, and with its growing incidence, it has to be considered an important differential while evaluating chronic knee pain in adolescents [6]. Secondary ABC has been associated with GCT in almost 14% of cases of long-term bony involvement [9]. But a combined GCT and ABC in a sesamoid bone remains a rare entity and needs to be brought to light. These symbiotic tumors present with similar clinical features as a solitary GCT of the patella, and many times the treatment protocol remains unchanged [9]. Definitive diagnosis of such rare tumors is often established on histopathology examination but requires intensive imaging primarily. In symbiotic tumors, the primary tumors dominate the radiologic appearance in 80% of cases, with the secondary ABC component often being obscured in the background of the primary GCT [10]. All these make a radiologic diagnosis difficult and make a core biopsy an absolute pre-requisite before embarking on any surgical intervention. Devkota et al. [11] cited some important differentials mimicking patellar GCT, which includes-chondroblastoma (the second most common tumor of the patella), haemangioma, osteoblastoma, and enchondroma. A bone biopsy turns out to be a fundamental test to confirm the diagnosis in such a setting. The real challenge is decision-making and choosing the line of management for these tumors. Cortical thinning, Campanacci grading, pathological fractures, and soft tissue involvement are some important parameters to keep in mind while deciding whether to salvage or resect [5]. While the consensus in treating long bony GCT is quite established, there still exists a cloud of uncertainty revolving around the treatment of patellar tumors [9]. Being a relatively rare tumor, various authors have treated them according to two schools of thought: extended curettage with adjuvant or total patellectomy with a good extensor repair. Just like GCT of long bones, there are instances of recurrences in patellar GCT treated with curettage. Devkota et al. [11] reported two instances of patellar GCT recurrence, which were primarily treated with extended curettage. Both of these tumors were radiologically graded as Campanacci grade 2 on initial evaluation pre-opertively. Iqbal et al. [6] recommended patellectomy as a better single-shot management of such tumors, which yields good results with proper extensor repair. In another article by Slavchev et al. [2], it has been highlighted that, being a rare tumor with no strict treatment protocol, it is better to opt for patellectomy for these locally aggressive tumors. Very recently, Tripathy et al. [9] treated a combined GCT and ABC tumor in an adolescent girl with total patellectomy, which recorded an excellent result at 1 year follow-up. Our patient was also treated with a total patellectomy, which yielded an excellent functional outcome. Our report highlights an unusual occurrence of a patellar GCT combined with ABC. Although this diagnosis is based on histology and the presence of an additional ABC component does not alter the course of management, such rare tumors must be identified. A simple patellectomy might look like an overzealous treatment, but it significantly reduces the risk of recurrence, which might require multiple procedures. Often, patients are suffering from long-standing pain and willingly opt for a single-staged patellectomy after they have been briefed about the pros and cons of the treatment options. But the long-term results of such radical procedures as patellectomy still need to be reviewed [9]. Denosumab has played a new role in shrinking these tumor sizes and providing good tumor resection margins when used pre-operatively in long bone GCTs [12]. However, it is costly, and using it in a scenario where there is no soft tissue involvement for a GCT of a sesamoid bone where salvage is difficult does not seem judicious. Having done a thorough review of the literature, we found surgeons favoring to preserve the patella in Campanacci grade 1 GCT, while patellectomies in grades 2 and 3 have yielded good results over the years. Hence, it is critical to diagnose these tumors at an early stage. A good clinical examination, meticulous history-taking, and a plain radiograph of the affected joint will go a long way toward prevent missing such tumors. It is important to keep these tumors as an important differential to anterior knee pain while treating patients, as it will always leave an option to salvage the patella when diagnosed early.
With the incidence of bone tumors on the rise, one should be aware of this relatively rare cause of anterior knee pain. Early diagnosis is the crux of an effective treatment protocol and a better rehabilitation and functional outcome. A simple radiograph will help in early diagnosis and will go a long way toward better salvage procedures than more radical procedures like patellectomy.
Patellar tumors are rare. The presentation of anterior knee pain in young adults must be evaluated properly to prevent missing such tumors. An early diagnosis will help in the effective salvage of this sesamoid bone.
References
- 1.Mercuri M, Casadei R. Patellar tumors. Clin Orthop Relat Res 2001;389:35-46. [Google Scholar | PubMed]
- 2.Slavchev SA, Georgiev GP, Patrikov K. An active giant cell tumor of the patella: A case report. Cureus 2017;9:e1642. [Google Scholar | PubMed]
- 3.Lucas DR. Dahlin’s bone tumors: General aspects and data on 11,087 cases. Am J Clin Pathol 1996;106:693. [Google Scholar | PubMed]
- 4.Song M, Dai W, Sun R, Liang H, Liu B, Wu Y, et al. Giant cell tumor of the patella with a secondary aneurysmal bone cyst: A case report. Oncol Lett 2016;11:4045-8. [Google Scholar | PubMed]
- 5.Morris TM, Gamie Z, Ghosh KM, Rankin KS. Giant cell tumour of the patella with local recurrence: Successful management with excision, curettage and artificial bone grafting. BMJ Case Rep 2018;2018:bcr2017221275. [Google Scholar | PubMed]
- 6.Iqbal M, Khan AS, Khawaja UA, Saleem A. Giant cell tumour of the patella: A missing differential diagnosis in the young. Cureus 2022;14:e25151. [Google Scholar | PubMed]
- 7.Escribano Rueda LC, Sánchez Gutiérrez SJ, Gómez-Rice A, de Lucas Aguilar R, Gómez García A. Tumor de células gigantes en rótula: A propósito de un caso y revisión de la literatura [Patellar giant cell tumour: Presentation of a case and a review of the literature]. Rev Esp Cir Ortop Traumatol 2012;56:486-90. [Google Scholar | PubMed]
- 8.Song M, Zhang Z, Wu Y, Ma K, Lu M. Primary tumors of the patella. World J Surg Oncol 2015;13:163. [Google Scholar | PubMed]
- 9.Tripathy SK, Doki S, Behera G, Sable M. Giant cell tumor with secondary aneurysmal bone cyst of the patella: A case report. Cureus 2019;11:e5819. [Google Scholar | PubMed]
- 10.Bonakdarpour A, Levy WM, Aegerter E. Primary and secondary aneurysmal bone cyst: A radiological study of 75 cases. Radiol 1978;126:75-83. [Google Scholar | PubMed]
- 11.Devkota K, Bhattarai M, Adhikari K. Giant cell tumor of the patella: An uncommon site. Nepal J Radiol 2018;8:30-2. [Google Scholar | PubMed]
- 12.Li H, Gao J, Gao Y, Lin N, Zheng M, Ye Z. Denosumab in giant cell tumor of bone: Current status and pitfalls. Front Oncol 2020;10:580605. [Google Scholar | PubMed]