It should be kept in mind that the hip may be luxated due to hip movement limitation in children diagnosed with JIA.
Dr. Murat Taşc, Assistant Professor, Umraniye Training and Research Hospital, Department of Orthopedics and Traumatology, Istanbul, Turkey. E-mail: drtascimurat@gmail.com
Introduction: Juvenile idiopathic arthritis (JIA) is a persistent autoimmune-inflammatory disease that affects children younger than 16. Aggressive synovitis of the hip may cause joint destruction, hip protrusion, erosion, pseudosubluxation, dysplasia, and osteoarthritis. Subluxation of the hip had been reported previously. However, dislocation of the hip in JIA is an extremely rare situation, and only two cases have been reported up to date. Reduction of the dislocated hip has to be performed in any way. However, there is no algorithm to be followed for the treatment of hip dislocations caused by JIA.
Case Presentation: In this study, we presented two cases of hip dislocation caused by JIA. Case 1: An 11-year-old boy had JIA and chronic recurrent multifocal osteomyelitis (CRMO). X-rays and computed tomography (CT) revealed a posterior dislocation of the left hip. An urgent operation was planned for the reduction of the hip. Avascular necrosis, dysplasia, or erosions were not evident at the last follow-up. Case 2: An 11-year-old girl was referred to the hospital with excessive left hip pain starting 24 h ago. A limited synovectomy with joint irrigation was performed. However, pathological examination of the synovium showed chronic inflammation consistent with JIA. On the post-operative 10th day, the patient was consulted for an increase in hip pain and deformity of the left hip. X-rays and MRI revealed posterior dislocation of the left hip with synovial hypertrophy. An urgent operation was planned. The hip could be reduced under anesthesia with mild traction, and a pelvipedal cast was applied only for 3 weeks. Avascular necrosis, dysplasia, destruction, or erosions were not evident at the last follow-up.
Conclusion: For early diagnosed patient reduction under anesthesia and medial soft-tissue contracture release; for late diagnosed patient medial soft-tissue contracture release, capsulotomy and synovectomy were effective to prevent destruction and early degenerative changes of the hip joint for treatment of dislocation caused by JIA.
Keywords: Juvenile idiopathic arthritis, monoarthritis, hip, dislocation, surgery.
Juvenile idiopathic arthritis (JIA) is a persistent autoimmune-inflammatory disease that affects children younger than 16. This is the most common arthritic disease of childhood and may be manifest clinically in three ways: oligoarthritis, polyarthritis, and systemic arthritis [1]. The initial subtype of the manifestation may alter with the proceeding of the disease [2]. The mainstay of the treatment is non-steroidal anti-inflammatory drugs, systemic corticosteroids, disease-modifying medication (methotrexate, sulfasalazine, and/or biological), and physical therapy [3]. Although the disease is managed by pediatric rheumatology, orthopedic surgeons become involved either at the initial onset of the disease for differential diagnosis or after failed medical management to perform some varieties of salvage procedures. The frequency of joint involvement in the disease is as follows: knee, hand/wrist, ankle, hip, and spine. The hip joint is commonly affected in JIA (70%) and particularly in cases of systemic polyarticular disease (50%). However, isolated hip monoarthritis diagnosed with oligoartricular-JIA has been reported in only a few cases, and a positive HLA B27 test in these patients may be an indicator for aggressive synovitis and severe hip arthritis [4]. Joint destruction may occur in the hip because of synovitis; hip protrusion due to erosion; pseudosubluxation due to synovial hypertrophy and capsule laxity; dysplasia and osteoarthritis occurs because of growth disturbances if the disease occurs at younger ages [5]. Although subluxation of the hip is a known condition due to hip flexor contractures, dislocation of the hip in JIA is an extremely rare situation, and only two cases have been reported up to date [6,7]. All of these conditions are debilitating and need to be addressed. Synovectomy, soft-tissue release, limb length discrepancy correction, arthrodesis, and joint replacement are most performed surgeries for JIA patients by orthopedists [1]. In this study, we presented the treatment of hip dislocation for two children caused by JIA.
Case 1
An 11-year-old boy was consulted by the pediatric orthopedic team at the pediatric rheumatology clinic because of flexion and adduction contracture of the left hip. The medical history of the patient revealed that the patient had a JIA with polyarticular onset (bilateral knees, wrists, and hips; HLA B27 positive; ANA negative) from the age of 4 and was also diagnosed with CRMO 2 years ago. The patient had used corticosteroids and conventional and biological disease-modifying antirheumatic drugs (DMARDs) and had come to follow-ups in a regular fashion. The patient had developed polyarthralgia resistant to all available treatments involving both hips and knees in February 2020. Non-steroidal anti-inflammatory drugs (NSAIDs) had been prescribed, and a rehabilitation program at home had been initiated to restore range of motion (ROM) in both hips and knees. The patient had caught a COVİD-19 infection during rehabilitation at home but had been treated successfully without any complications. However, the patient had lost follow-ups during the initial lockdown because of the COVİD-19 pandemic between April and August 2020, could not get his biological DMARDs during this period, and showed up with severe pain in his left hip.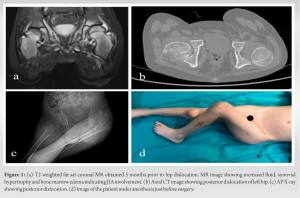
The physical examination revealed a fixed flexion-adduction contracture of the left hip, limb-length discrepancy, and flexion contracture of the left and right knees as well. The patient could not walk or sit, and the hip was very painful during the examination. X-rays and computed tomography (CT) revealed a posterior dislocation of the left hip. Also, an MRI was planned, but the patient could not tolerate being positioned in the MRI during scanning. Parents reported the patient to be in this posture for 3–4 weeks (Fig. 1). At the time of consultation, WBC counts were high (17.00/uL), Hgb levels were low (9,7/g/dl), CRP levels were just over normal ranges (8,6 mg/dl), sedimentation, levels were high (89 mm/h), and a fever was not detected. An urgent operation was planned for the reduction of the hip. The hip and knees were still contracted under anesthesia, and the hip could not be reduced with traction. An arthrography was performed prior to the incision, and the arthrography revealed excessive synovium filling the medial acetabulum (Fig. 1). Thus, a medial approach was used, as all medial muscles, including adductors and iliopsoas, were contracted, and all synovium was located medially. A transverse 5cm incision was performed 2 cm distal to the origin of the adductor magnus muscle. A tenotomy of the adductor muscles and medial pectineus muscle was performed. The whole synovium with the medial capsule was resected. After the removal of the synovium, the hip was reduced without any effort. Furthermore, a limited hamstring lengthening was performed for both left and right knee flexion contractures. Moreover, a pelvipedal cast was applied for 3 weeks. After 3 weeks, the cast was altered to a bilateral long-leg cast, and hip flexion and extension were allowed. The remaining casts were removed after another three weeks, and full weight bearing with physical therapy for muscle strengthening was allowed. This patient’s last follow-up was in the post-operative 16th month. Pain was mild and inconsistent; activated with activity, hip flexion was 100°, abduction was 35°, adduction was 15°, internal rotation was 10°, and external rotation was 15°. The patient could walk for a short time and limp existed without a cane, but could walk for a long time with a cane. Hip functions were revealed to be very good, and a very great improvement was achieved in hip functions after surgery, according to the Merle d’Aubigné classification system [8]. The arthritis was rated using the Larsen classification [9]. The patient had grade 1 destruction, including slight joint space narrowing (<25%) and periarticular osteopenia, both at pre-operative and last post-operative X-rays. Avascular necrosis, dysplasia, or erosions were not evident at the last follow-up (Fig. 2).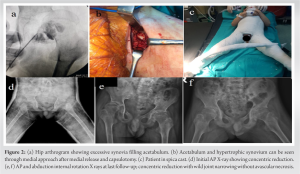
Case 2 (persistent oligoarticular JIA)
An 11-year-old girl consulted with the pediatric orthopedic team at the pediatric rheumatology clinic. The patient had been referred to the hospital with excessive left hip pain starting 24 h ago. The medical history of the patient was normal, but the patient reported the pain starting 4 months ago, particularly being disturbing in the mornings, but that does not limit her daily activities. The patient was living in an urban area and had contact with farm animals. The physical examination revealed irritated hip findings, including severe hip pain with the hip movements and pseudo-paralyses with the hip in mild flexion and adduction. At the time of consultation, WBC counts were high (14.900/uL), Hgb levels were within normal ranges (13,7/g/dl), CRP levels were within normal ranges (<0,2 mg/dl), sedimentation levels were within normal ranges (16mm/h), and a fever was not detected. X-rays were normal, and there was no evident pathology. MRI revealed increased fluid in the left hip joint space and thickened and inflamed synovium (Fig. 3). At this stage, a puncture was performed to rule out septic arthritis. However, neither an increase in synovial fluid cell counts (WBC=18000, PMN%63) nor a bacteria in gram staining were detected (bacteria cultures were also revealed to be negative after three days). However, surgery was planned to rule out mycobacterium, brucella, and fungal infections and perform a debridement to alleviate the pain of the patient, as irritated hip findings were still evident despite the initiation of NSAIDs during 24 h. An anterior approach was performed. A mild synovial hypertrophy was detected during surgery, and a limited synovectomy with joint irrigation was performed. A survey for viral pathologies and JIA was initiated after surgery, and the patient was followed by a pediatric infectious disease clinic. During the 1st week, the hip pain of the patient was consistent, but the acute phase reactants were within normal ranges. Laboratory surveys for mycobacterium (ppd), brucella (IgG and IgM), viral panel surveys, and antinuclear anticore (ANA), HLA-B27, anti-ds DNA, and rheumatoid factor (RF) were revealed to be negative. However, pathological examination of the synovium showed chronic inflammation consistent with JIA (synovial tissue in a villoidal configuration containing lymphocytes). On the post-operative 10th day, the patient was consulted for an increase in hip pain and deformity of the left hip. A physical examination of the patient revealed fixed flexion and adduction of the left hip. Hip was reported to be in this position for 14 h. Also, the first toe was numb, and the patient was unable to extend the first toe. X-rays and MRI revealed posterior dislocation of the left hip with synovial hypertrophy. An urgent operation was planned. Hips could be reduced under anesthesia with mild traction. However, the adductor muscles were contracted. Therefore, a percutaneous adductor tenotomy was performed, and a pelvipedal cast was applied only for 3 weeks. A conventional DMARD treatment with corticosteroids was initiated initially after surgery with the diagnosis of oligoartihritic JIA. After the initiation of treatment for JIA, the pain was alleviated dramatically, and the patient was pain-free in the cast. Full weight bearing with physical therapy was started after the removal of the cast, and pain did not recur after the removal of the cast. The partial sciatic nerve (peroneal branch) palsy healed at post-operative 3 months.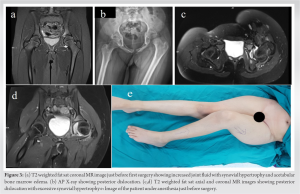
The last follow-up was at the post-operative 21st month. There was no pain, neither with activity nor in rest; hip range of motion (ROM) was within normal ranges; the patient could walk without cane, limping, and pain for a long time. Hip functions were revealed to be very good, and a very great improvement was achieved in hip functions after surgery, according to the Merle d’Aubigné classification system [8]. Radiographically, the left hip was totally normal (Larsen stage 0); avascular necrosis, dysplasia, destruction, or erosion were not evident at the last follow-up. However, mild synovial hypertrophy was still evident on MRI sections obtained at the post-operative 14th month (Fig. 4).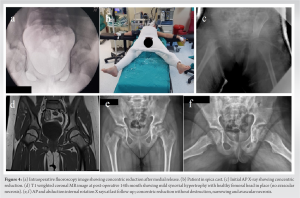
Hip involvement in JIA is not a frequent manifestation, and synovial hypertrophy of the hip can result in several debilitating pathologies, including destruction of the chondral surface, osteoarthritis, dysplasia, and limb length discrepancies. Medical treatment of the hip involves NSAIDs, paracetamol, resting, and conventional or biological DMARD treatments as for other joints. Synoviectomy and/or medial soft-tissue release is indicated as a salvage procedure for cases that have resistant synovial hypertrophy. Persistent synovial hypertrophy and capsule laxity in JIA push the patient to take the hip in flexion, inter-rotation, and adduction positions, which later cause contracture of the adductor muscles and iliopsoas muscles and subluxation of the femoral head. Although subluxation of the hip has been reported in hip involvement, dislocation is very rare, and only two case reports are available up to now. Reduction of the dislocated hip has to be performed in any way. However, there is no algorithm to be followed for the treatment of hip dislocations caused by JIA. The first case was reported in 1975 [7]. The authors had used skin traction for reduction and put the patient in a spica cast. The second case was reported in 2004 [6]. Authors had used skin traction but could not obtain a reduction. Thus, they used an anterolateral approach for soft-tissue release and synovectomy and followed the patient in a spica cast for 3 weeks. However, both studies reported early destruction, deformation, and degeneration of the joint despite successful reduction of the hips. In both of our cases, we did not use traction for reduction of the hip as a first-step attempt because dislocation was very new in the second case, and we presumed that the hip could be reduced under anesthesia. In the second case, the dislocation had been evident for at least 3 weeks and even more because the hamstrings were contracted, so it was clear that reduction could not be obtained just with traction. Hip-joint synovectomy has not yet been proven to have a real joint-preserving effect in patients with rheumatic diseases [10]. However, Carl et al. [3] claimed this procedure to be effective and safe, even in patients with late-stage articular damage, through an anterior approach in terms of pain and mobility. The authors had used an anterolateral approach for synovectomy and soft-tissue release, as this approach could be considered safer to avoid injury to the medial femoral circumflex artery. However, the authors had dislocated the hip in some cases with severe hypertrophy that could not be reached through an anterior incision. In our first case, we performed the synovectomy through a medial incision as a pre-operative arthrogram revealed excessive synovial hypertrophy pooled medially. Therefore, we presume that a cautious medial approach could be safe and effective to release all medial contractures and perform a radical synovectomy. Moreover, fixed deformation of the hip makes it very difficult to perform an anterolateral approach without compressing the femoral head against the posterior acetabular wall, which can cause avascular necrosis of the femoral head. In the second case, only medial soft-tissue release was effective, as a concentric reduction was verified with fluoroscopy after release. To us, preservation of the hip in a spica cast for 2–3 weeks is mandatory, as these patients tend to keep the hip in flexion and adduction despite the muscle release. Actually, in the second case, persistent pain could have warned us to apply a spica cast for 2 weeks after the first intervention. This could have alleviated the pain and synovial hypertrophy, which eventually resulted in hip dislocation. Sure, it is impossible to draw exact conclusions from two cases. However, our cases revealed that cessation of treatment in active aggressive JIA cases and persistent pain resistant to NSAID treatment may be indicative of dislocation. Thus, the application of a spica cast or close follow-up may prevent debilitating complications. Treatment must be based on the individual. Concentric reduction must be the ultimate goal, with or without radical synovectomy. In the second case, synovectomy was not performed, and mild medial synovial hypertrophy was still evident at the post-operative 14th month. But there was no pain or degenerative change after 21 months of follow-up. Also, the first case was doing well clinically after synovectomy, and the progression of destruction was prevented after 16 months of follow-up.
For early-diagnosed patients, reduction under anesthesia and medial soft-tissue contracture release; for late-diagnosed patients, medial soft-tissue contracture release and synovectomy could be effective to prevent destruction and early degenerative changes of the hip joint for the treatment of dislocation caused by JIA.
Restricted hip movement in children diagnosed with JIA could signal a serious issue. Active and aggressive cases of JIA, as well as persistent pain resistant to NSAID treatment, may suggest the possibility of hip dislocation. Patients with JIA, especially those who take breaks from treatment, should undergo a careful evaluation.
References
- 1.Iesaka K, Kubiak EN, Bong MR, Su ET, Di Cesare PE. Orthopedic surgical management of hip and knee involvement in patients with juvenile rheumatoid arthritis. Am J Orthop (Belle Mead NJ) 2006;35:67-73. [Google Scholar]
- 2.Strickler AL, Cifuentes D, Mihovilovic K, Vergara F, Grez M, Rivera V. Change of diagnosis and diagnostic category in patients with juvenile idiopathic arthritis within 7 years of follow-up. Rev Chil Pediatr 2020;91:521-8. [Google Scholar]
- 3.Carl HD, Schraml A, Swoboda B, Hohenberger G. Synovectomy of the hip in patients with juvenile rheumatoid arthritis. J Bone Joint Surg Am 2007;89:1986-92. [Google Scholar]
- 4.Lepore N, Cashin M, Bartley D, Ardelean DS. Atypical monoarthritis presentation in children with oligoarticular juvenile idiopathic arthritis: A case series. Pediatr Rheumatol Online J 2017;15:2. [Google Scholar]
- 5.Rydholm U. Growth affection. In: Surgery tor Juvenile Chronic Arthritis. Lund, Sweden: Ortholani; 1990. [Google Scholar]
- 6.Inui K, Maeno T, Tada M, Takaoka K, Koike T. Open reduction of the dislocated hip in juvenile idiopathic arthritis: A case report. Mod Rheumatol 2004;14:399-401. [Google Scholar]
- 7.Ahmad I. Juvenile rheumatoid arthritis causing hip dislocation. Case report. Bull Hosp Joint Dis 1975;36:159-62. [Google Scholar]
- 8.Merle d’Aubigné R, Cauchoix J, Ramadier JV. Quantitative assessment of hip function. Application to the study of the results of hip mobilization operations. Rev Chir Orthop 1949;35:541-8. [Google Scholar]
- 9.Larsen A, Dale K, Eek M. Radiographic evaluation of rheumatoid arthritis and related conditions by standard reference films. Acta Radiol Diagn (Stockh) 1977;18:481-91. [Google Scholar]
- 10.Jacobsen ST, Levinson JE, Crawford AH. Late results of synovectomy in juvenile rheumatoid arthritis. J Bone Joint Surg Am 1985;67:8-15. [Google Scholar]