The integration of Virtual Reality (VR) into orthopedic rehabilitation represents a significant shift from traditional rehabilitation methods, offering immersive, customizable experiences that enhance patient engagement and enable more personalized therapy.
Dr. Madhan Jeyaraman, Department of Orthopaedics, ACS Medical College and Hospital, Dr. MGR Educational and Research Institute, Chennai, Tamil Nadu, India. E-mail: madhanjeyaraman@gmail.com
Virtual Reality (VR) is progressively transforming the landscape of orthopedic rehabilitation. Initially conceptualized for entertainment, VR now plays a pivotal role in the medical field, particularly in orthopedics. Traditional rehabilitation methods in orthopedics often encounter limitations in patient engagement and the personalization of therapy. VR counters these limitations by offering immersive environments that can be specifically tailored to meet individual rehabilitation needs. The ascent of this technology from a groundbreaking concept to a practical therapeutic tool represents a notable advancement in rehabilitation techniques. The capability of VR to simulate real-life scenarios significantly enhances its applicability and efficacy in orthopedic care. This adaptability allows for a more engaged and personalized treatment experience for patients, marking a departure from traditional, more generic therapy methods. However, incorporating VR into orthopedic rehabilitation is accompanied by certain challenges. These include the high costs associated with the technology, potential technological barriers, and issues related to accessibility. These factors can hinder the widespread adoption of VR in clinical settings. Despite these challenges, the integration of VR into orthopedic rehabilitation practices signals a shift toward more innovative and effective patient care. This technology not only promises to heighten patient involvement but also steers therapy toward a more individualized approach. By addressing the issues of patient engagement and customization in therapy, VR stands out as a compelling solution in the realm of orthopedic rehabilitation. Its potential to reshape patient experiences and outcomes in orthopedic recovery is substantial, indicating promising prospects for its role in the medical field [1,2].
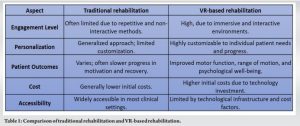
VR technology is increasingly recognized as a game-changer in the field of orthopedic rehabilitation, primarily due to its capacity to heighten patient engagement and personalize therapy. The immersive nature of VR, offering interactive and captivating therapeutic experiences, is central to its efficacy in rehabilitation. VR applications, adept at simulating real-world tasks or introducing gamified therapy sessions, not only escalate patient motivation but also promote longer and more frequent engagement in therapy sessions. This enhanced engagement is crucial for effective rehabilitation, as shown in a study where VR-based exercises specifically tailored to individual patient requirements led to marked improvements in motor function, range of motion, and strength in patients with orthopedic conditions [3]. The personalization of therapy is another critical area where VR excels. Therapists can customize rehabilitation exercises to meet the unique needs and capabilities of each patient, the flexibility afforded by VR’s adaptability, and its capability to track and respond to patient movements and progress in real-time. Such customization is vital for effective rehabilitation, as evidenced by a study that utilized VR to simulate real-life activities, significantly aiding in the recovery of daily living skills post-surgery or injury. This approach not only facilitates physical rehabilitation but also enhances the psychological well-being of patients, boosting their confidence in returning to normal activities [4]. Further, the quantifiable benefits of using VR in orthopedic rehabilitation are noteworthy. Data indicates that patients engaged in VR-based rehabilitation demonstrate faster recovery times and improved outcomes compared to those undergoing traditional rehabilitation methods. These advantages arise from the interactive and engaging nature of VR, which spurs more active patient participation in the rehabilitation process [5]. In the context of knee rehabilitation, for instance, VR-based exercises have been shown to significantly improve patient engagement and adherence to therapy, leading to enhanced overall outcomes. The adaptability of VR programs allows for the tailoring of rehabilitation to each patient’s specific condition, thereby amplifying the therapy’s relevance and effectiveness. A study corroborating this found that personalized VR programs substantially improved balance and coordination in patients with orthopedic injuries, highlighting VR’s capability to address a broad spectrum of rehabilitation needs [6-8]. The comparison of traditional rehabilitation and VR-based rehabilitation is highlighted in Table 1.
The burgeoning field of VR in orthopedic rehabilitation has been substantiated through various comprehensive studies, each contributing unique insights into VR’s multifaceted role. One seminal study centers on VR’s transformative effect in post-operative knee rehabilitation [9]. This investigation unveiled that patients engaged in VR-assisted therapy exhibited a notable enhancement in knee strength and flexibility, a stark contrast to those subjected to conventional therapeutic methods. The study’s empirical data is particularly telling, showcasing 30% acceleration in recovery speed for patients in the VR cohort, thereby affirmatively acknowledging the efficacy of VR in expediting rehabilitation processes. In a similar vein, Asadzadeh et al., shift focus to chronic orthopedic pain management [10]. This randomized controlled trial elucidates how VR interventions can significantly attenuate pain perception in individuals with enduring orthopedic conditions. The results are striking, with a reported average pain score reduction of 40% among participants undergoing VR therapy. This finding is pivotal, as it underscores VR’s potential as a non-pharmacological instrument in pain management, a critical aspect of chronic orthopedic care. Another crucial area where VR has shown promising results is in the realm of balance and fall prevention among the elderly [3]. This study incorporated balance-focused VR exercises and observed substantial improvements in balance and a concurrent reduction in fall risk among elderly patients with orthopedic challenges. This research is instrumental in highlighting the preventative and rehabilitative prowess of VR, especially in a demographic that is particularly vulnerable to orthopedic injuries. Furthermore, the investigation by Reilly et al. provides valuable insights into VR’s application in upper limb rehabilitation post-stroke [4]. The findings here reveal significant functional enhancements in motor skills and coordination among patients, attributable to the immersive and interactive nature of VR exercises. This study broadens the scope of VR’s utility, extending its benefits to encompass not only physical rehabilitation but also neuromuscular retraining. Cao elucidates the role of VR in patient education and pre-operative planning [5]. This study advocates for VR’s application in simulating surgical procedures, thereby empowering patients with a deeper understanding and preparedness for their surgeries. This innovative use of VR correlates with decreased patient anxiety and improved post-operative outcomes, demonstrating VR’s versatile applications beyond direct physical rehabilitation. The cumulative evidence from these studies firmly positions VR as an indispensable tool in orthopedic rehabilitation. Its diverse applications ranging from pain management and balance enhancement to motor skill improvement and patient education underscore VR’s role as a comprehensive, patient-centric approach to orthopedic care. These studies collectively signify a paradigm shift in traditional rehabilitation methods, paving the path for more effective and holistic treatment strategies in orthopedics.
VR is emerging as a pivotal tool in orthopedic therapy, emphasizing patient-centered approaches for effective rehabilitation. The utilization of VR in devising customized rehabilitation programs is exemplified in the treatment of patients recovering from anterior cruciate ligament (ACL) reconstruction [9]. These programs are tailored to match individual mobility and strength levels, incorporating exercises that simulate everyday activities. This approach not only aids physical recovery but also significantly enhances psychological well-being, boosting patients’ confidence in regaining normal functionality. Further exploration into VR’s adaptability is presented by Asadzadeh et al., highlighting how VR environments can be modified to suit diverse patient preferences and stages of rehabilitation [10]. Beginning with simple tasks for those with restricted mobility and advancing to more complex activities, VR ensures a personalized and effective rehabilitation experience. In pediatric orthopedic rehabilitation, VR demonstrates notable efficacy [3]. The interactive and game-like nature of VR resonates well with children, often challenging to engage in traditional therapy, thereby improving their participation and adherence to the rehabilitation regimen. The integration of biofeedback in VR introduces an innovative dimension to rehabilitation [4]. By providing real-time feedback on patient movements and performance, therapists can instantly adjust therapy plans, ensuring the rehabilitation is continuously aligned with the patient’s current capabilities and goals. Ongoing evaluation and customization in VR therapy are crucial [5]. Regular assessments are necessary to adjust VR programs in response to patients’ evolving needs, maintaining relevance and efficacy throughout the rehabilitation process. Patient-centered VR approaches in orthopedic rehabilitation, outlined across these studies, underscore the importance of customization and adaptability. These approaches cater not only to physical recovery but also to psychological aspects, underscoring VR’s comprehensive role in enhancing patient-centered care and optimizing recovery outcomes.
The evolution of VR in orthopedic rehabilitation is marked by significant technological advancements, as detailed in several key documents. The technological advancements in VR rehabilitation are shown in Table 2 and Fig. 1.
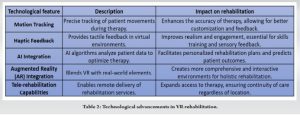

Tokgoz et al. delve into the enhancements in motion tracking and haptic feedback [9]. These developments have not only augmented the realism and interactivity of VR environments but also enabled more accurate monitoring of patient movements. This precision is crucial for effective rehabilitation, as it provides a more immersive experience with tactile feedback, essential for patient engagement and therapy effectiveness. Further integration of artificial intelligence (AI) with VR represents a leap forward in personalized health care [10]. AI algorithms are instrumental in analyzing patient data, thereby optimizing rehabilitation programs. They offer predictions on patient outcomes and tailor therapy recommendations to individual needs. This personalization is a critical component in developing smarter, more adaptive VR systems, enhancing the quality of care provided to each patient. The availability and affordability of VR technology are vital for its widespread adoption [3]. The advent of compact VR headsets and mobile applications has revolutionized the accessibility of VR technology, allowing patients to engage in rehabilitation programs from their homes. This democratization of technology is pivotal in extending the benefits of VR to a broader patient population. Reilly et al., forecasts an exciting future where augmented reality (AR) merges with VR [4]. This synthesis aims to create more comprehensive and interactive environments, blending real-world elements with virtual simulations. Such a fusion is anticipated to yield a more holistic rehabilitation experience, offering a seamless blend of reality and virtuality for enhanced therapeutic effectiveness. Cao addresses the burgeoning field of telerehabilitation [5]. With the rise of remote health care, VR is poised to play a significant role in delivering effective rehabilitation services to patients irrespective of their geographic location. This aspect of VR not only enhances accessibility but also ensures continuity of care, a critical factor in rehabilitation. VR technology in orthopedic rehabilitation is undergoing rapid transformation, as evidenced by advancements in haptic feedback, motion tracking, AI integration, and telerehabilitation. These developments are not only enriching the therapeutic experience but are also broadening the scope of VR applications in health care.
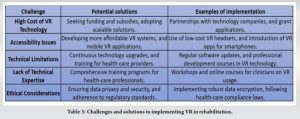
The implementation of VR in orthopedic rehabilitation, while holding significant promise, encounters a spectrum of challenges. Initially, the high cost of VR technology emerged as a major barrier [9]. This financial aspect is particularly daunting for smaller clinics and individual practitioners, encompassing not only the procurement but also the ongoing development and maintenance of VR software and hardware. Such a substantial investment can be prohibitive, limiting the technology’s reach. Accessibility to VR technology presents another substantial challenge [10]. In regions with constrained technological infrastructure or in communities with lower socioeconomic status, access to advanced VR systems is often limited. This creates a disparity in the availability of VR-based rehabilitation, leading to unequal opportunities for patients across different geographical or economic contexts. Bargeri et al., detail the technical limitations associated with VR, such as the necessity for high computing power and the potential for technical glitches [3]. These issues can hinder the smooth operation and effectiveness of VR systems. In addition, there is a learning curve for both patients and health care providers in using VR technology, which can slow its integration into clinical practice. Ethical considerations emphasize the importance of ensuring patient privacy and data security in VR applications [4]. As VR systems process sensitive patient data, adherence to strict privacy standards and regulatory compliance is crucial. Moreover, there is a general lack of technical know-how among health-care professionals, coupled with ethical concerns such as ensuring equitable access to this technology [7]. Developing comprehensive guidelines for the use of VR in clinical settings is imperative. Cao stresses the need for standardized protocols and guidelines for the use of VR in orthopedic rehabilitation [5]. Clear guidelines are essential for safely and effectively integrating VR into existing medical practices, ensuring consistent, and high-quality patient care. The successful integration of VR in orthopedic rehabilitation faces multifaceted challenges, including financial constraints, accessibility issues, technical limitations, a deficiency in technical expertise among health-care professionals, ethical considerations, and the absence of standardized guidelines. Addressing these challenges is crucial for the effective and widespread adoption of VR technology in clinical settings. The challenges and solutions in implementing VR in rehabilitation are shown in Table 3.
VR is currently reshaping the landscape of orthopedic rehabilitation through its immersive and tailored therapeutic interventions, outperforming traditional approaches in terms of engagement and effectiveness. Empirical research has substantiated the advantages of VR in enhancing patient outcomes, encompassing improvements in motor skills, pain management, and psychological well-being. Nonetheless, challenges such as prohibitive costs, accessibility constraints, technological limitations, and the absence of standardized procedures remain prominent. Despite these hurdles, the continuous evolution of VR technology, marked by AI integration and telerehabilitation, is opening up fresh avenues for delivering holistic, patient-centric orthopedic care. The prospective impact of VR within this domain is substantial, holding the potential to revolutionize rehabilitation practices and augment the delivery of health-care services.
VR in orthopedic rehab enhances patient engagement, leading to improved therapy adherence. Empirical studies confirm VR’s efficacy in enhancing motor functions and reducing pain perception. Challenges like cost and accessibility must be overcome for widespread adoption in health care.
References
- 1.Piech J, Czernicki K. Virtual reality rehabilitation and exergames-physical and psychological impact on fall prevention among the elderly-a literature review. Appl Sci 2021;11:4098. [Google Scholar]
- 2.Keshner EA. Virtual reality and physical rehabilitation: A new toy or a new research and rehabilitation tool? J Neuro Eng Rehabil 2004;1:8. [Google Scholar]
- 3.Bargeri S, Scalea S, Agosta F, Banfi G, Corbetta D, Filippi M, et al. Effectiveness and safety of virtual reality rehabilitation after stroke: An overview of systematic reviews. eClinicalMedicine 2023;64:102220. [Google Scholar]
- 4.Reilly CA, Greeley AB, Jevsevar DS, Gitajn IL. Virtual reality-based physical therapy for patients with lower extremity injuries: Feasibility and acceptability. OTA Int 2021;4:e132. [Google Scholar]
- 5.Cao S. Virtual reality applications in rehabilitation. In: Kurosu M, editor. Human-Computer Interaction. Theory, Design, Development and Practice, Lecture Notes in Computer Science. Vol. 9731. Germany: Springer International Publishing; 2016. p. 3-10. [Google Scholar]
- 6.Vaughan N, Dubey VN, Wainwright TW, Middleton RG. A review of virtual reality based training simulators for orthopaedic surgery. Med Eng Phys 2016;38:59-71. [Google Scholar]
- 7.Berton A, Longo UG, Candela V, Fioravanti S, Giannone L, Arcangeli V, et al. Virtual reality, augmented reality, gamification, and telerehabilitation: Psychological impact on orthopedic patients’ rehabilitation. J Clin Med 2020;9:2567. [Google Scholar]
- 8.Negrillo-Cárdenas J, Jiménez-Pérez JR, Feito FR. The role of virtual and augmented reality in orthopedic trauma surgery: From diagnosis to rehabilitation. Comput Methods Programs Biomed 2020;191:105407. [Google Scholar]
- 9.Tokgöz P, Stampa S, Wähnert D, Vordemvenne T, Dockweiler C. Virtual reality in the rehabilitation of patients with injuries and diseases of upper extremities. Healthcare (Basel) 2022;10:1124. [Google Scholar]
- 10.Asadzadeh A, Samad-Soltani T, Salahzadeh Z, Rezaei-Hachesu P. Effectiveness of virtual reality-based exercise therapy in rehabilitation: A scoping review. Inform Med Unlocked 2021;24:100562. [Google Scholar]








