The synergistic relationship between the ACL and hamstring muscles in preventing anterior translation of the tibia necessitates staged reconstruction in the setting of a simultaneous injury to protect the new ACL graft.
Dr. John H Wilckens, Department of Orthopaedic Surgery, Johns Hopkins Medicine, Baltimore. E-mail: jwilcke1@jhmi.edu
Introduction: Simultaneous anterior cruciate ligament (ACL) and ipsilateral hamstring ruptures have never been reported in the literature. The purpose of this article is to describe a treatment approach for such a case. The principles in this case can help guide treatment for any patient with concomitant ACL and hamstring pathology.
Case Report: We describe the case of a 53-year-old male who presented with left ipsilateral simultaneous complete proximal hamstring tendon (HT) and ACL tears after an acute tennis injury. He was successfully treated with a staged procedure, first with a proximal HT repair and later with a delayed ACL reconstruction using a bone-patellar tendon-bone autograft.
Conclusion: Ipsilateral simultaneous complete proximal HT and ACL tears can be successfully treated with acute proximal HT repair and delayed ACL reconstruction after rehabilitation from the HT repair. The synergistic relationship between the ACL and hamstring muscles in preventing anterior translation of the tibia necessitates staged reconstruction in the setting of a simultaneous injury.
Keywords: Anterior cruciate ligament, hamstring tendon, orthopedics.
Anterior cruciate ligament (ACL) ruptures are a common athletic injury, with an estimated annual incidence of 100,000–200,000 in the United States [1]. Surgical treatment options include reconstruction with bone-patellar tendon-bone (BTB), hamstring tendon (HT), or quadriceps tendon autograft or allograft. In 1985, Walla et al. reported that hamstring function is particularly important in the ACL-deficient knee because the hamstring muscles prevent anterior translation of the tibia and unload the ACL [2]. More recent studies have reported an increased incidence of ACL ruptures in patients with a history of hamstring injuries [3] and an increased incidence of hamstring injuries in patients with a history of ACL injury [4], highlighting the synergistic relationship between the structures [3]. While acute hamstring strains are a common injury in athletes, proximal hamstring tears or avulsion injuries are much less common and are treated as a separate injury [5,6]. A lack of prompt recognition and treatment of proximal HT ruptures can lead to a delay in return to sports and long-term functional impairments, persistent pain, and sciatic nerve symptoms [7-9]. To our knowledge, simultaneous ACL and ipsilateral hamstring ruptures have never been reported in the literature. Therefore, the purpose of this article is to describe a treatment approach for such a case. The principles in this case can help guide treatment for any patient with concomitant ACL and hamstring pathology. The patient was informed that his case would be submitted for publication, and he provided consent. Institutional Review Board approval was not required for the publication of this case report.
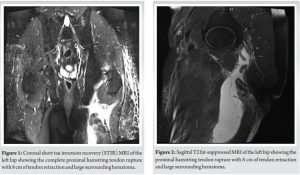
A 53-year-old previously healthy male presented after sustaining injuries to his left knee and posterior thigh while playing tennis. The patient stated that he was lunging to hit a ball when he felt a pop in his posterior thigh. Upon planting his foot, he also felt a pop in his knee. He experienced immediate pain and an inability to ambulate. X-rays in the emergency department were negative. Upon presentation to the clinic 7 days later, the patient had marked posterior left thigh ecchymosis that extended proximally to the gluteal crease. There was palpable fullness distal to the gluteal crease. Knee examination was significant for a 2+ Lachman test and mild effusion. Subsequent MRI of the pelvis revealed proximal common HT rupture with 8 cm of tendon retraction and a large surrounding hematoma (Fig. 1 and 2).
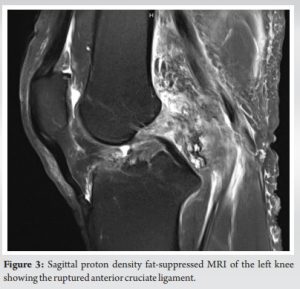
A knee MRI demonstrated a complete rupture of the ACL and a complex tear of the posterior horn of the medial meniscus (Fig. 3).
Treatment options included non-operative treatment and repair or reconstruction of one or both tears. Following shared decision-making, the patient elected to proceed with aspiration of the hematoma to improve knee range of motion (ROM) and ameliorate his symptoms, followed by operative repair of the left tendon rupture. The plan was to assess knee stability and function after the tendon repair and then consider reconstructing the ACL.
Surgical technique: Proximal HT repair
The patient was placed in the prone position on the operating table. An incision was marked transversely along the gluteal fold. The stump of the avulsed hamstring was palpable just distal to the planned incision site, as was the planned repair location on the ischial tuberosity. Dissection was conducted to the gluteal fascia, and the thickened hamstring fascia and bursa were identified. The avulsed HTs were identified and mobilized so the repair could be completed under minimal tension. The sciatic nerve was identified just anterior to the HT muscles. Next, three sets of locking stitches were run along the tendon, and three G-4 suture anchors (Mitek, Chesterfield, MO) were placed in the ischial tuberosity. The residual tendon origin was used to help guide anchor placement. The sutures were tied down, and the tendon was oversewn with a suture from the central anchor. The patient was placed in a knee ROM brace (Bledsoe) locked at 60° of flexion to take tension off the repair. He was made non-weightbearing on his left lower extremity.
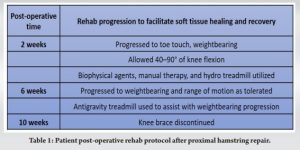
Rehabilitation after proximal HT repair
Table 1 outlines the patient’s post-operative protocol. He had 4/5 tibialis anterior and extensor hallucis longus weakness and paresthesia immediately post-operatively, attributed to a common peroneal nerve traction injury. These symptoms resolved within 2 months with the use of a home-based personal biofeedback unit. At 5 months, his rehabilitation progress slowed, and he complained of persistent instability in his left knee. On physical examination, he continued to have a 2+ Lachman test. An MRI again showed a ruptured ACL and medial meniscal tear. Because he had persistent physical limitations, the patient elected to proceed with ACL reconstruction with a BTB autograft.
Surgical technique: ACL reconstruction
The patient was placed supine on the operating table, and a tourniquet was placed around the left upper thigh. An incision was made at the anterior aspect of the knee from the inferior pole of the patella down the tibial tubercle, exposing a 30-mm-wide patellar tendon. The central 10 mm were taken with bone plugs. Diagnostic arthroscopy revealed a complete rupture of the ACL and a medial meniscus tear involving 30% of the middle and posterior third. The meniscal tear was debrided to a stable rim. The patient underwent a 2-incision ACL reconstruction with his patellar tendon autograft fixed with two 17-mm ligament buttons. The knee was taken through a full ROM and noted to be stable to Lachman and anterior drawer testing. The wounds were irrigated and closed in a layered fashion. The patient was then placed in a knee brace, locked in extension.
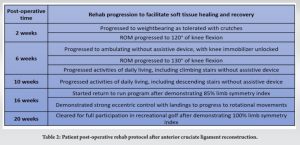
Rehabilitation after ACL reconstruction
Table 2 outlines the patient’s post-operative protocol. At his 2-year follow-up from the ACL reconstruction (approximately 2.5 years after the hamstring repair), he had no complaints and was jogging and playing golf. His left knee ROM was 8° of hyperextension and 135° of flexion; strength and endurance testing of the quadriceps and hamstrings were within 15% of the contralateral side; and he had a stable Lachman test.
We describe here a treatment approach for ipsilateral simultaneous complete proximal HT rupture and ACL tears. In any clinical encounter, it is important to maintain a high index of suspicion for concomitant pathologies; in this case, a thorough physical examination revealed posterior thigh ecchymosis, a knee effusion, and a positive Lachman test, which led to the diagnosis of two simultaneous injuries. The next step was to prioritize treatment options. Conservative treatment for proximal hamstring tears can result in poor outcomes, including persistent pain, decreased function, and an inability to participate in sports [7-9]. Therefore, surgical repair is typically recommended for partial-thickness tears that have not improved with non-surgical care, for 2-tendon injuries with retraction of ≥ 2 cm, and for complete 3-tendon injuries [8,10,11]. Early treatment is preferred because chronic injuries are more challenging to repair and have a higher risk of complications [7,8,10]. Because of the knee ROM restrictions placed to rehab from the hamstring repair, and because complications can arise if knee ROM cannot be regained after ACL reconstruction [12], we recommended that the patient proceed with proximal HT repair first, with consideration of ACL reconstruction only after recovery. After recovering from the tendon repair, the patient elected to proceed with ACL reconstruction. ACL reconstruction is usually recommended for active individuals who wish to return to high-level sports or activities that involve cutting or pivoting motions [13]. Non-operative treatment involves bracing and physical therapy and is often recommended for older individuals and those who might not require a high level of knee stability [13]. Recent studies have shown that delaying ACL reconstruction beyond 6 months is associated with an increased rate of revision surgery and worse patient outcomes [14]. In the case presented here, we needed to prioritize recovery from the proximal HT repair, and the delayed ACL reconstruction appears not to have negatively affected the patient’s 1-year outcome. There is a known relationship between hamstring and ACL injuries. Visser et al. reported an increased risk for hamstring injuries in patients with a history of ipsilateral ACL reconstruction [4]. Conversely, a history of hamstring injuries has been reported to be associated with an increased risk of ACL rupture [3]. The proposed mechanism for synergistic functions of the ACL and hamstring musculature is that hamstring muscle contraction unloads the ACL by resisting anterior translation of the tibia, therefore decreasing the risk of ACL rupture [3]. This synergistic relationship provides a challenge for treating both injuries simultaneously. In our review of the literature, which included a database search on PubMed and Embase with the terms ACL, hamstring, and simultaneous, we did not find any articles that mentioned cases of simultaneous ACL and hamstring ruptures. Furthermore, an ipsilateral hamstring injury alters graft selection options for ACL reconstruction. Two of the most commonly used graft options for ACL reconstruction are BTB and HT autografts [15]. A recent systematic review and meta-analysis of randomized controlled trials reported no significant differences between BTB and HT grafts with regard to returning to a pre-injury level of physical activity or sports participation [15]. In our case, an HT graft was not possible because of the proximal hamstring injury, so BTB was an appropriate graft choice.
Ipsilateral simultaneous complete proximal HT and ACL tears can be successfully treated with acute proximal HT repair and delayed ACL reconstruction after rehabilitation from the HT repair.
This case report presents the first simultaneous ACL and ipsilateral hamstring ruptures reported in the literature. Although this case was rare, the important principles in the case can be applied to more common clinical scenarios. The synergistic relationship of the ACL and hamstring muscles in preventing anterior translation of the tibia necessitated healing of the HTs before ACL reconstruction to protect the BTB autograft.
References
- 1.Evans J, Nielson J. Anterior cruciate ligament knee injuries. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. [Google Scholar | PubMed]
- 2.Walla DJ, Albright JP, McAuley E, Martin RK, Eldridge V, El-Khoury G. Hamstring control and the unstable anterior cruciate ligament-deficient knee. Am J Sports Med 1985;13:34-9. [Google Scholar | PubMed]
- 3.Opar DA, Serpell BG. Is there a potential relationship between prior hamstring strain injury and increased risk for future anterior cruciate ligament injury? Arch Phys Med Rehabil 2014;95:401-5. [Google Scholar | PubMed]
- 4.De Visser HM, Reijman M, Heijboer MP, Bos PK. Risk factors of recurrent hamstring injuries: A systematic review. Br J Sports Med 2012;46:124-30. [Google Scholar | PubMed]
- 5.Pombo M, Bradley JP. Proximal hamstring avulsion injuries: A technique note on surgical repairs. Sports Health 2009;1:261-4. [Google Scholar | PubMed]
- 6.Agre JC. Hamstring injuries. Proposed aetiological factors, prevention, and treatment. Sports Med 1985;2:21-33. [Google Scholar | PubMed]
- 7.Irger M, Willinger L, Lacheta L, Pogorzelski J, Imhoff AB, Feucht MJ. Proximal hamstring tendon avulsion injuries occur predominately in middle-aged patients with distinct gender differences: Epidemiologic analysis of 263 surgically treated cases. Knee Surg Sports Traumatol Arthrosc 2020;28:1221-9. [Google Scholar | PubMed]
- 8.Bodendorfer BM, Curley AJ, Kotler JA, Ryan JM, Jejurikar NS, Kumar A, et al. Outcomes after operative and nonoperative treatment of proximal hamstring avulsions: A systematic review and meta-analysis. Am J Sports Med 2018;46:2798-808. [Google Scholar | PubMed]
- 9.Hofmann KJ, Paggi A, Connors D, Miller SL. Complete avulsion of the proximal hamstring insertion: Functional outcomes after nonsurgical treatment. J Bone Joint Surg Am 2014;96:1022-5. [Google Scholar | PubMed]
- 10.Lempainen L, Banke IJ, Johansson K, Brucker PU, Sarimo J, Orava S, et al. Clinical principles in the management of hamstring injuries. Knee Surg Sports Traumatol Arthrosc 2015;23:2449-56. [Google Scholar | PubMed]
- 11.Degen RM. Proximal hamstring injuries: Management of tendinopathy and avulsion injuries. Curr Rev Musculoskelet Med 2019;12:138-46. [Google Scholar | PubMed]
- 12.Shelbourne KD, Freeman H, Gray T. Osteoarthritis after anterior cruciate ligament reconstruction: The importance of regaining and maintaining full range of motion. Sports Health 2012;4:79-85. [Google Scholar | PubMed]
- 13.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: A systematic review and meta-analysis of the state of play. Br J Sports Med 2011;45:596-606. [Google Scholar | PubMed]
- 14.Forsythe B, Lu Y, Agarwalla A, Ezuma CO, Patel BH, Nwachukwu BU, et al. Delaying ACL reconstruction beyond 6 months from injury impacts likelihood for clinically significant outcome improvement. Knee 2021;33:290-7. andomized controlled trials. Am J Sports Med 2022;50:2292-303. [Google Scholar | PubMed]
- 15.Bergeron JJ, Sercia QP, Drager J, Pelet S, Belzile EL. Return to baseline physical activity after bone-patellar tendon-bone versus hamstring tendon autografts for anterior cruciate ligament reconstruction: A systematic review and meta-analysis of r [Google Scholar | PubMed]