A combined approach using ALT flap and multiple tendon grafts, along with interposed vein grafts, can effectively salvage a severely injured lower limb following a road accident. How to salvage a severely injured lower limb following a road accident.
Dr. Gloria Fanton, Department of Neurosciences, Clinic of Plastic Surgery, University of Padua, Padua, Italy. E-mail: gloria.fanton@aopd.veneto.it
Introduction: The free anterolateral thigh (ALT) flap is commonly used to repair a large loss of soft tissue following a lower-limb injury. An issue to be managed is the choice of adequate recipient vessels when the tibial arteries result damaged. In this scenario, vein grafts can be interposed to connect a healthy recipient vessel to the ALT flap pedicle.
Case Report: We present a report of a 19-year-old male who suffered a Gustilo fracture type IIIc after a road injury involving the right lower limb. After a failed first attempt of limb salvage with reconstruction of extensor tendons and a free ALT flap, a second procedure was performed using another ALT flap with interposed vein grafts to reach very proximal recipient vessels.
Results: The patient demonstrated excellent recovery and restored ambulation. The effectiveness of the most complex reconstructive options for a high-demanding patient with no comorbidities is demonstrated in this case.
Conclusion: The key to success in even the most complex injury cases is early intervention, meticulous surgical planning, and a multidisciplinary approach.
Keywords: Anterolateral thigh flap, vein graft, gustilo fracture, ankle, tendon graft, limb salvage.
Severe lower limb injuries resulting from road injury can frequently pose a significant challenge for both orthopedics and plastic surgeons. Beyond the necessity to warrant a prompt and stable wound healing, often a reconstruction of the tendinous extensor compartment of the foot is also required to give the patient the chance to walk again. The microsurgical anterolateral thigh (ALT) flap has proven to be an effective reconstructive tool in replacing large soft-tissue losses [1]. Significant advantages characterize the ALT flap as versatility, easy dissection, adequate size to cover large wounds, and an excellent perfusion. However, when the vessels in close proximity to the wound are compromised, a long pedicle can be required to reach a distant blood source. ALT pedicle ranges from 5 up to 7 cm in length and thus may not be long enough to anastomose with healthy recipient vessels. To obviate to this inconvenient, a complementary microsurgical technique, the vein grafting, can be used to elongate the flap pedicle and so permitting a successful outcome [2].
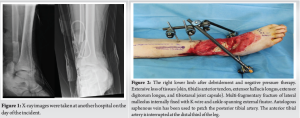
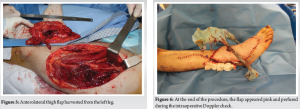
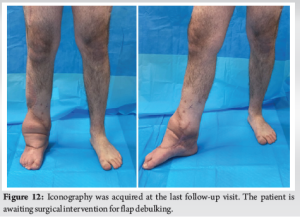
A 19-year-old male was referred to our tertiary hospital following a motorcycle accident that caused significant damage to his right lower limb (Fig. 1). He suffered a near-complete amputation of the ankle joint with interruption of the anterior and posterior tibial arteries (Fig. 2). In urgency, he underwent a limb-salvaging procedure with an open angioplasty of the anterior tibial artery and a patching of the severed posterior tibial artery. The procedure was successful but the soft tissues of the distal third of the lower limb started to suffer, and after 3 days the dorsal aspect of the right ankle and foot presented a full-thickness skin necrosis. Given the patient’s young age and absence of comorbidities, a conservative approach was chosen. The patient was assessed as suitable for the reconstruction procedure after undergoing multiple debridement sessions and negative pressure therapy application. The first surgery involved reconstruction of the tibialis anterior tendon and extensor longus hallucis using a contralateral plantar tendon graft, along with reconstruction of the extensor retinaculum using an autologous fascia lata graft (Fig. 3 and 4). A fasciocutaneous ALT flap was harvested from the contralateral thigh and used as a free flap to cover the exposed bone and joint area (Fig. 5). Finally, skin grafts were utilized to cover the remaining non-critical defects. There was no perfusion impairment of the free flap at the time of microsurgical anastomose to the mid-leg anterior tibial vessels (artery and concomitant vein), and the procedure was considered successful (Fig. 6). The flap conditions begin to deteriorate the 2nd day after surgery. Venous congestion was suspected and resulted in the patient returning to the OR (Fig. 7). The most likely cause of this venous congestion was the excessive tension placed on the venous anastomosis during microsurgery, in conjunction with an inadequately sized recipient vein. This could have been prevented by selecting a larger recipient vein or using a vein graft to create an adequate conduit and reduce the tension on the vascular anastomosis. Despite all efforts, the flap had to be removed and negative pressure therapy was applied to prevent infection and necrosis of the underlying tendons. A second reconstructive surgery was carried out using another microsurgical ALT flap that was harvested from the ipsilateral thigh. To ensure proper vascular supply to the flap, two 10-cm vein grafts from the left forearm were interposed between the recipient limb vessels (proximal posterior tibial artery and comitant vein) and the ALT flap pedicle (Figs. 8 and 9). Targeted antibiotic therapy was used for postoperative management due to multi-microbial contamination. After the second procedure, the patient’s condition improved rapidly, and after 6 days, he was able to start the rehabilitation program. After 2 months, ambulation with crutches was achieved (Fig. 10) and after 5 months, full ambulation capability was achieved (Fig. 11). The reconstructive effort focused on two key tendons in the ankle and foot which are the tibialis anterior tendon and the extensor hallucis longus. The tibialis anterior is responsible for dorsiflexion of the ankle joint and plays a role in inversion, which is the movement of turning the foot inward. The extensor hallucis longus is responsible for extending the great toe, which is crucial for grip and balance. The dorsiflexion movement, crucial for walking, running, and jumping, has been partially achieved. The patient walks smoothly and is deemed satisfied with the achieved outcome (Fig. 12). He is currently awaiting flap debulking surgery.





Free ALT flaps have emerged as a versatile option for lower limb reconstruction due to its abundant blood supply, the ease of harvesting, and reliable outcomes [3,4]. The ALT flap provides ample soft-tissue coverage, making it ideal for large tissue defects, as proven in our clinical case [1]. The ability to transfer vascularized tissue as a fasciocutaneous flap-sparing muscle also reduces the risk of donor site morbidity [5]. Several studies have reported favorable outcomes of ALT flaps in lower limb reconstruction [6,7]. However, even when soft-tissue coverage is achieved, the functional recovery depends mainly on the recovery of the range of motion of the ankle joint though a tendon reconstruction. In this case, extensor tendon reconstruction was achieved using a contralateral plantar tendon graft for the tibialis anterior and extensor longus hallucis muscles. The use of plantar tendon grafts has been shown to provide a durable and effective solution for tendon defects, allowing for the restoration of function and joint stability [8,9]. The choice of a plantar tendon graft in our patient was justified by its availability, proximity, and similarity to the damaged tendons. A fascia lata graft was utilized to reconstruct the extensor retinaculum. The use of fascia lata to reconstruct tendons is well known in the literature due to its higher resistance to infection, faster healing, fewer adhesions, and better gliding capability [10]. However, the simultaneous reconstruction of ankle tendons, retinaculum, and a free flap covering has not yet been described before. The major complication that occurred after the first procedure demonstrates the significance of thorough preoperative planning and precise localization of healthy recipient vessels. Despite the initial failure, the decision to attempt a second reconstructive surgery with a new ALT flap and the use of subcutaneous vein grafts proved to be successful in restoring adequate blood supply and tissue coverage. This case report emphasizes the importance of appropriate patient selection, in fact, the effects of the injury can be detrimental for blood vessels, which may be altered after direct trauma and prolongate exposition to inflammatory agents. Nowadays, the use of a free flap is the first choice in many cases of lower limb expose fracture, but the microsurgical technique necessitates accurate planning and patent recipient vessels. When a composite reconstruction is required, both of skin envelope and tendon apparatus, patient’s comorbidities such as altered glycemia, atherosclerosis, and venous hypertension should be taken in great consideration due to the higher risk of flap failure. On the other hand, when the patient does not present any comorbidity, is young in age, and shows high compliance to medical advices, orthopedic and plastic surgeons should consider the opportunity to perform a complex procedure to reach the best functional outcome.
The use of a free ALT flap combined with vein, tendon, and fascia lata grafts proved to be effective to meet the needs of our young patient. Early intervention, meticulous surgical planning, and a multi-disciplinary approach are essential in managing such complex injury cases. The successful outcome in this case underlines the importance of further research and studies to explore the potential of combining different reconstructive methods to improve limb salvage rates in severe trauma cases. In addition, long-term follow-up studies are essential to assess the functional and esthetic outcomes of these procedures.
Complex reconstructive procedures represent a valuable alternative to limb amputation in selected cases, offering the potential for functional limb preservation and improved quality of life. Successful outcomes depend on comprehensive anatomical reconstruction, addressing vascular, bone, tendon, and soft-tissue deficits. Multistage procedures are often required, necessitating patient counseling and strict adherence to post-operative rehabilitation protocols. Surgical expertise plays a pivotal role in ensuring the success of these complex reconstructions.
References
- 1.Kim JH, Yoo H, Eun S. Reconstruction of extensive soft tissue defects of lower extremity with the extended anterolateral thigh flap. Int J Low Extrem Wounds 2022;21:601-8. [Google Scholar | PubMed]
- 2.Langdell HC, Shammas RL, Atia A, Chang EI, Matros E, Phillips BT. Vein grafts in free flap reconstruction: Review of indications and institutional pearls. Plast Reconstr Surg 2022;149:742-9. [Google Scholar | PubMed]
- 3.Luo S, Raffoul W, Luo J, Luo L, Gao J, Chen L, et al. Anterolateral thigh flap: A review of 168 cases. Microsurgery 1999;19:232-8. [Google Scholar | PubMed]
- 4.Nosrati N, Chao AH, Chang DW, Yu P. Lower extremity reconstruction with the anterolateral thigh flap. J Reconstr Microsurg. 2012 May;28(4):227-34. [Google Scholar | PubMed]
- 5.Ali RS, Bluebond-Langner R, Rodriguez ED, Cheng MH. The versatility of the anterolateral thigh flap. Plast Reconstr Surg 2009;124:e395-407. [Google Scholar | PubMed]
- 6.Dayan JH, Lin CH, Wei FC. The versatility of the anterolateral thigh flap in lower extremity reconstruction. Handchir Mikrochir Plast Chir 2009;41:193-202. [Google Scholar | PubMed]
- 7.Lin CH, Wei FC, Lin YT, Yeh JT, Rodriguez Ede J, Chen CT. Lateral circumflex femoral artery system: Warehouse for functional composite free-tissue reconstruction of the lower leg. J Trauma 2006;60:1032-6. [Google Scholar | PubMed]
- 8.Ruchelsman DE, Christoforou D, Wasserman B, Lee SK, Rettig ME. Avulsion injuries of the flexor digitorum profundus tendon. J Am Acad Orthop Surg 2011;19:152-62. [Google Scholar | PubMed]
- 9.Fletcher DR, McClinton MA. Single-stage flexor tendon grafting: Refining the steps. J Hand Surg Am 2015;40:1452-60. [Google Scholar | PubMed]
- 10.Lucattelli E, Delcroix L, Baldrighi C, Tanini S, Innocenti M. Quadriceps tendon reconstruction using a fascia lata included in a reverse-flow anterolateral thigh flap. Microsurgery 2019;39:642-6. [Google Scholar | PubMed]











