Total hip replacement is an excellent option post acetabular fixation leading to hip arthritis, AVN or neglected dislocation as in our report.
Dr. Turki Alshehri, Department of Trauma and Orthopaedic Surgery, Armed Forces Hospital Southern Region, Khamis Mushait, Saudi Arabia. E-mail: express507@hotmail.com
Introduction: An acetabular fracture is a relatively uncommon injury. An acetabular fracture can occur in conjunction with a posterior hip dislocation. Oni defined neglected hip dislocation as dislocation lasting more than 1 week after injury.
Case Report: We present a 31-year-old male involved in a road traffic accident 6 months ago. He had 5 cm of shortening on examination, and the sciatic nerve was intact. The patient had post-traumatic arthritis and was counseled for total hip arthroplasty (THA) and its complications.
Conclusion: Neglected posterior dislocation of the hip after acetabular fracture fixation is rare these days. It is a time-sensitive medical emergency that must be reduced within 6 h to avoid its complications, especially avascular necrosis and post-traumatic arthritis.
Keywords: Neglected, hip dislocation, acetabulum fixation.
Posterior dislocation of the hip is a high-energy trauma mostly occurring after road traffic accidents or falls from heights. The dislocation can occur as an isolated injury or in association with an acetabular fracture. Acetabular fracture is a relatively uncommon fracture, challenging for surgeons as it is a more complex and challenging injury to treat [1]. Acetabular fractures have an incidence of approximately three patients/100,000/year [2] and mainly occur in two distinct age groups: Young patients develop acetabular fractures after high-energy trauma, whereas elderly patients develop acetabular fractures after low-energy trauma associated with osteoporotic bone status [3-6]. The standard procedure for displaced and unstable acetabular fractures consists of surgical anatomical reconstruction, followed by internal fixation and early mobilization, or total hip arthroplasty (THA) for post-traumatic arthritis or avascular necrosis (AVN) [3,4,7,8]. Hip dislocations are divided into anterior and posterior types. Posterior dislocations vastly outnumber anterior dislocations [9]. Posterior hip dislocation can be linked with an acetabular fracture, which increases the risk of complications [10]. Oni defined neglected hip dislocation as dislocation lasting more than 1 week after injury [9]. This definition is based on the fact that patients seen within 1 week of injury can be successfully treated by manipulative reduction, just as in fresh cases. Beyond this time, the acetabulum becomes filled with fibrous tissue, and capsular contractures occur across the base of the acetabulum. Loose intra-articular osteochondral fragments and labral tears become adherent to the acetabulum, making reduction difficult or impossible by closed maneuvers [9,11]. Herein, we presented a 31-year-old male diagnosed with neglected posterior dislocation hip post-acetabulum fixation.
We present a 31-year-old male involved in a road traffic accident 6 months ago in our institution’s outpatient department who had acetabular fracture fixation in another hospital with pain, shortening, and internal rotation. He had 5 cm of shortening on examination, and the sciatic nerve was intact.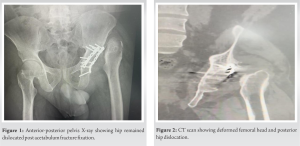 Anterior-posterior pelvis X-rays showed that the hip remained dislocated post-acetabulum fracture fixation (Fig. 1). In addition, a computed tomography (CT) scan shows a deformed femoral head, post-traumatic arthritis, and posterior hip dislocation (Fig. 2 & 3).
Anterior-posterior pelvis X-rays showed that the hip remained dislocated post-acetabulum fracture fixation (Fig. 1). In addition, a computed tomography (CT) scan shows a deformed femoral head, post-traumatic arthritis, and posterior hip dislocation (Fig. 2 & 3).
The patient was counseled for THA and complications. The patient underwent an uncemented total hip replacement (j&j) pinnacle cup and corail stem with a 32 mm ceramic head through an anterolateral approach in the lateral decubitus position. Extensive adhesions were released along the femoral neck and head, and fibro-fatty tissue was removed from the floor of the acetabulum. Intra-operative fluoroscopy was used to identify the true floor of the acetabulum for placement of the acetabular cup in the optimum position to achieve the ideal center of rotation and offset. The reconstruction plated used for fracture fixation was not in the way of the acetabulum cup positioning, so it was left in situ. The post-operative patient had equal limb lengths with intact sciatic nerve and mobilized full-weight bear as tolerant and discharged home. At 6 months and 1 year, an X-ray showing the implant was stable with no radiolucent lines (Fig. 4 & 5 ).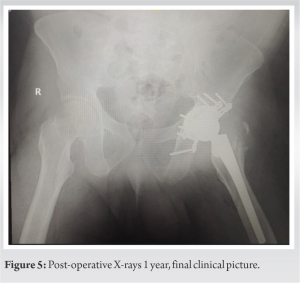
Posterior dislocation of the hip is a high-energy trauma, usually when the position of hip is in adduction and flexion. It can be isolated or associated with complex acetabulum fractures. Fixation of acetabulum fractures is a complex and demanding surgery, even for the most experienced surgeon. Pre-requisites for any acetabular fracture with dislocated hips are anatomical reduction, rigid fixation, and congruent joint post-fixation to delay post-traumatic arthritis and AVN hips, which will eventually need THA pain relief. Hip dislocation can be linked with an acetabular fracture, which increases the risk of complications [9]. Posterior dislocations greatly outnumber anterior dislocations [12]. Pubic-type dislocations result from abduction, extension, and external rotation of the hip. Obturator-type dislocations result from abduction, flexion, and external rotation of the hip [13]. Patients with anterior dislocations may have a palpable femoral head in the femoral triangle in contrast to a palpable femoral head in the gluteal area with posterior dislocations [2]. Neglected hip dislocations occur when a patient does not or cannot obtain appropriate medical care [14]. Herein, we present a case of a 31-year-old male diagnosed with neglected posterior dislocation of the hip post-acetabulum fixation. Neglected posterior hip dislocation is common in developing countries for various causes. Sometimes, the patient does not arrive at the medical facility on time or when the dislocation is well advanced due to insufficient treatment by local bone setters [15]. Hip dislocation can also be overlooked in polytrauma patients when the more visible or life-threatening injuries take precedence and the patient’s consciousness is muted [15]. Hip dislocations are time-sensitive medical emergencies that must be reduced within the first 6 h to avoid the chances of the femoral head’s devascularization, increasing by 20 fold the critical time, leading to AVN [16]. Our case was discovered after 6 months of acetabulum fixation, and immediately, he was counseled for THA, where he underwent an uncemented total hip replacement. A routine anteroposterior (AP) radiograph of the pelvis is mandatory for all patients sustaining multiple traumas. In posterior fracture-dislocations of the hip, the AP radiograph of the pelvis usually displays a small femoral head above the acetabular dome and different patterns of acetabular fractures. Posterior wall fractures are the most common pattern, accounting for 18–33% of all acetabular fractures. CT scans obtained before reduction help evaluate and decision-making about the injured hip. Magnetic resonance imaging has been proven to have a limited role in diagnosing and assessing posterior fracture-dislocations of the hip. However, MRI can effectively identify non-displaced fractures that are not apparent on axial CT scans [13,17]. Regarding our case, an AP X-ray of the pelvis was first done, and it showed the hip remained dislocated post-acetabulum fracture fixation. The CT scan showed a deformed femoral head and posterior hip dislocation. Most authors recommend initial traction followed by open reduction by either a lateral or posterolateral approach [18-20]. Concentric reduction is essential in children because the femoral head needs to stay in the acetabulum for appropriate growth and remodeling. Adult research on neglected cases of pure posterior dislocation (Type I) must be improved. Few studies on ignored dislocations with accompanying acetabulum fractures (Type II or above) have discovered that primary THA produces the best results [21-23]. THA was a practical choice to control our case, where he underwent an uncemented total hip replacement. Fluoroscopic guidance is frequently used to evaluate bone preparation, check component positioning, and measure leg length and offset during the surgery [24]. Accurate acetabular cup placement is critical for the long-term success of hip replacements [25]. Traditional landmarks for establishing acetabular component position can be variable, leading to placement outside Lewinnek’s safe zone [26]. Fluoroscopic imaging has increased accuracy in the acetabular cup position and is an advantage of the anterior hip approach [27]. Herein, we used intra-operative fluoroscopy to identify the acetabulum’s true floor to place the acetabulum cup in the optimum position. The Harris hip score (HHS) is a joint-specific score completed by the clinician and the patient. It consists of 10 items covering pain, function, functional activities, deformity, and hip range of motion. The HHS was initially described for the assessment of functional outcomes after mold arthroplasty for posttraumatic arthritis [28]. The HHS has been used to evaluate functional outcomes after the pertrochanteric hip fracture and the intracapsular fracture of the neck of the femur [29-31]. Regarding our case, pre- and post-operative Harris hip scores at 6 months showed implant stability with no radiolucent lines.
Total hip replacement is an excellent option for post-acetabular fixation, leading to HIP arthritis, AVN, and pain relief, as in our report. Neglected posterior dislocation of the hip after acetabulum fracture fixation is rare. THA is a practical and standard choice for post-traumatic hip arthritis, as in our case.
Posterior dislocation of hip is a high energy trauma usually when the position of hip is in adduction and flexion. It can be isolated or associated with complex acetabulum fractures. Fixation of acetabulum fractures is a complex and demanding surgery even for the most experienced surgeon. Pre requiste for any acetabular fracture with dislocated hip is anatomical reduction rigid fixation and congruent joint post fixation to delay the post traumatic arthritis and AVN hip which will need total hip arthroplasty eventually for pain relief.
References
- 1.Iqbal F, Taufiq I, Najjad MK, Khan N, Zia OB. Functional and radiological outcome of surgical management of acetabular fractures in tertiary care hospital. Hip Pelvis 2016;28:217-24. [Google Scholar | PubMed]
- 2.Laird A, Keating JF. Acetabular fractures: A 16-year prospective epidemiological study. J Bone Joint Surg Br 2005;87:969-73. [Google Scholar | PubMed]
- 3.Hanschen M, Pesch S, Huber-Wagner S, Biberthaler P. Management of acetabular fractures in the geriatric patient. SICOT J 2017;3:37. [Google Scholar | PubMed]
- 4.Mears DC. Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg 1999;7:128-41. [Google Scholar | PubMed]
- 5.Rinne PP, Laitinen MK, Huttunen T, Kannus P, Mattila VM. The incidence and trauma mechanisms of acetabular fractures: A nationwide study in Finland between 1997 and 2014. Injury 2017;48:2157-61. [Google Scholar | PubMed]
- 6.Boudissa M, Francony F, Kerschbaumer G, Ruatti S, Milaire M, Merloz P, Tonetti J. Epidemiology and treatment of acetabular fractures in a level-1 trauma center: Retrospective study of 414 patients over 10 years. Orthop Traumatol Surg Res 2017;103:335-9. [Google Scholar | PubMed]
- 7.Vipulendran K, Kelly J, Rickman M, Chesser T. Current concepts: Managing acetabular fractures in the elderly population. Eur J Orthop Surg Traumatol 2021;31:807-16. [Google Scholar | PubMed]
- 8.Kelly J, Ladurner A, Rickman M. Surgical management of acetabular fractures-a contemporary literature review. Injury 2020;51:2267-77. [Google Scholar | PubMed]
- 9.Oni OO, Orhewere FA, Keswani H. The treatment of old unreduced traumatic dislocations of the hip. Injury 1984;15:219-23. [Google Scholar | PubMed]
- 10.Dilogo IH, Erwin US, Hendriarto A. Posterior dislocation of left hip joint with closed fracture of left acetabulum Judet-Letournel type posterior wall, femoral head fracture, management and follow up: A case report. Int J Surg Case Rep 2020;71:85-90. [Google Scholar | PubMed]
- 11.Buckwalter J, Westerlind B, Karam M. Asymmetric bilateral hip dislocations: A case report and historical review of the literature. Iowa Orthop J 2015;35:70-91. [Google Scholar | PubMed]
- 12.Waddell BS, Mohamed S, Glomset JT, Meyer MS. A detailed review of hip reduction maneuvers: A focus on physician safety and introduction of the Waddell technique. Orthop Rev (Pavia) 2016;8:6253. [Google Scholar | PubMed]
- 13.Alonso JE, Volgas DA, Giordano V, Stannard JP. A review of the treatment of hip dislocations associated with acetabular fractures. Clin Orthop Relat Res 2000;377:32-43. [Google Scholar | PubMed]
- 14.Clegg TE, Roberts CS, Greene JW, Prather BA. Hip dislocations--epidemiology, treatment, and outcomes. Injury 2010;41:329-34. [Google Scholar | PubMed]
- 15.Jain M, Swaroop S, Kumar DS. Neglected posterior hip dislocation in adults presenting after one year managed successfully with single stage Total hip arthroplasty: A case series. J Orthop Case Rep 2021;11:84. [Google Scholar | PubMed]
- 16.Mehlman CT, Hubbard GW, Crawford AH, Roy DR, Wall EJ. Traumatic hip dislocation in children. Long-term follow-up of 42 patients. Clin Orthop Relat Res 2000;376:68-79. [Google Scholar | PubMed]
- 17.Bhandari M, Matta J, Ferguson T, Matthys G. Predictors of clinical and radiological outcome in patients with fractures of the acetabulum and concomitant posterior dislocation of the hip. J Bone Joint Surg Br 2006;88:1618-24. [Google Scholar | PubMed]
- 18.Aguilar JA. Treatment of neglected traumatic posterior hip dislocation in children. Tech Orthop 2006;21:143-9. [Google Scholar | PubMed]
- 19.Gardner RO, Worku N, Nunn TR, Zerfu TT, Kassahun ME. Management of neglected traumatic hip dislocation in children. J Pediatr Orthop 2020;40:e554-9. [Google Scholar | PubMed]
- 20.Kumar S, Jain AK. Neglected traumatic hip dislocation in children. Clin Orthop Relat Res 2005;431:9-13. [Google Scholar | PubMed]
- 21.Ilyas I, Rabbani SA. Total hip arthroplasty in chronic unreduced hip fracture-dislocation. J Arthroplasty 2009;24:903-8. [Google Scholar | PubMed]
- 22.Epstein HC. Traumatic dislocations of the hip. Clin Orthop Relat Res 1973;92:116-42. [Google Scholar | PubMed]
- 23.McArthur BA, Schueler BA, Howe BM, Trousdale RT, Taunton MJ. Radiation exposure during fluoroscopic guided direct anterior approach for total hip arthroplasty. J Arthroplasty 2015;30:1565-8. [Google Scholar | PubMed]
- 24.Daines BK, Dennis DA. The importance of acetabular component position in total hip arthroplasty. Orthop Clin North Am 2012;43:e23-34. [Google Scholar | PubMed]
- 25.Barrack RL, Krempec JA, Clohisy JC, McDonald DJ, Ricci WM, Ruh EL, et al. Accuracy of acetabular component position in hip arthroplasty. J Bone Joint Surg Am 2013;95:1760-8. [Google Scholar | PubMed]
- 26.Slotkin EM, Patel PD, Suarez JC. Accuracy of fluoroscopic guided acetabular component positioning during direct anterior total hip arthroplasty. J Arthroplasty 2015;30:102-6. [Google Scholar | PubMed]
- 27.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969;51:737-55. [Google Scholar | PubMed]
- 28.Babhulkar S. Unstable trochanteric fractures: Issues and avoiding pitfalls. Injury 2017;48:803-18. [Google Scholar | PubMed]
- 29.Hopp S, Wirbel R, Ojodu I, Pizanis A, Pohlemann T, Fleischer J. Does the implant make the difference?-Prospective comparison of two different proximal femur nails. Acta Orthop Belg 2016;82:319-31. [Google Scholar | PubMed]
- 30.Zhang H, Zeng X, Zhang N, Zeng D, Xu P, Zhang L. Intertan nail versus proximal femoral nail antirotation-Asia for intertrochanteric femur fractures in elderly patients with primary osteoporosis. J Int Med Res 2017;45:1297-309. [Google Scholar | PubMed]
- 31.Frihagen F, Grotle M, Madsen JE, Wyller TB, Mowinckel P, Nordsletten L. Outcome after femoral neck fractures: A comparison of Harris Hip Score, Eq-5d and barthel index. Injury 2008;39:1147-56. [Google Scholar | PubMed]










