The purpose of this case report is to emphasis that orthopedic surgeon should be aware of different options for the treatment of aneurysmal bone cyst (ABC) including the use of denosumab; in addition, it highlights the importance of a multidisciplinary approach in managing these cases.
Dr. Ramy Samargandi Department of Orthopedic Surgery, Centre Hospitalier Régional Universitaire de Tours, (hôpital Trousseau), avenue de la République, Chambray-lès-Tours, 37044 Tours cedex 9, France. Email: ramy.samargandi@hotmail.com
Introduction: Aneurysmal bone cysts (ABCs) are aggressive and benign tumors that primarily affect children and adolescents. The standard course of treatment for ABCs involves surgical excision or curettage with a bone transplant or cement to repair the deficiency. Denosumab, a monoclonal antibody that inhibits receptor activator of nuclear kappa B ligand, is used to treat osteoporosis, skeletal metastasis, and giant cell tumors of the bones.
Case Report: This case study details the therapeutic treatment of a female patient, age 22, who had a recurring aggressive ABC of the distal tibia. The patient was initially treated using curettage and lesion filling. However, recurrence of the osteolysis was observed 9 months later that led to subsequent interventions involving absolute alcohol sclerotherapy in multiple sessions. However, these interventions failed to achieve ossification. Following unsuccessful surgical and sclerotherapy treatments, the patient was administered denosumab, which led to a positive response. Regular radiographic and clinical follow-up demonstrated significant improvements in ossification and pain reduction. During the course of the 12-month treatment, the frequency of visits was gradually reduced. Further, follow-up and monitoring revealed the effectiveness of the local control and long-term treatment.
Conclusion: This case report highlights the ability of denosumab to manage recurrent aggressive ABCs after surgical or sclerotherapy failure.
Keywords: Aneurysmal bone cyst, curettage, distal tibia, denosumab, recurrence, sclerotherapy.
Aneurysmal bone cysts (ABCs) are aggressive and benign tumors that comprise 1% of bone tumor cases [1]. ABCs primarily affect children and adolescents, with the majority of cases being diagnosed before 30 years of age. ABCs are often seen in the vertebrae, the pelvis, and the metaphyseal region of the long bones [1]. Approximately 70% of cases are primary ABCs, while the rest are secondary ABCs, often linked to tumors such as osteoblastoma and giant cell tumors of the bones (GCTBs) [2]. Distinguishing between the primary and secondary forms of the disease is necessary. The constituents of ABCs are multinucleated large cells that mimic osteoclasts and express high numbers of receptor activator of nuclear kappa B (RANK) receptors, as well as neoplastic stromal cells that express high amounts of RANK ligand (RANKL). The RANK-RANKL interaction triggers a signaling cascade that leads to an abnormally high rate of bone resorption, osteolysis, and destruction in ABCs. Like GCTBs, ABCs have similar histological features [3]. The standard course of treatment for ABCs involves surgical excision or curettage with a bone transplant or cement to repair the deficiency. Percutaneous sclerotherapy has also shown efficacy [4]. Other treatment options include curopsy, selective arterial embolization [5,6], and radiotherapy [7]. However, each has its limitations, underscoring the need for innovative treatments [2,7]. Denosumab, a monoclonal antibody that inhibits RANKL, is used to treat osteoporosis, skeletal metastasis, and GCTBs [8]. RANKL inhibition limits osteoclast formation and function [8]. Neoplastic stromal cells that express large amounts of RANKL and multinucleated giant cells that resemble osteoclasts and exhibit high levels of RANK receptor are the components of ABCs. The RANK-RANKL connection starts a signaling cascade in ABC patients that causes abnormally high levels of osteolysis, disintegration, and resorption of bone. GCTBs and ABCs share comparable histological characteristics [3]. Theoretically, denosumab may benefit patients with ABCs as well. This theory is supported by the published results of denosumab in GCTB treatment [8], the immunohistochemically similarity between ABCs and GCTB [9,10], and positive action of denosumab in few reported ABC cases [9]. This case report describes the clinical course and treatment decisions in a case of aggressive recurrent ABC at the distal end of the left tibia that was unresponsive to surgical and sclerotherapy treatments and reviews the relevant literature.
In June 2019, a 22-year-old lady complained of a limp, edema, and localized pain in her left ankle. She had no history of illness or injury. The swelling and pain progressively increased. The patient had not previously received any therapy. A clinical examination revealed distal ankle swelling with tenderness and pain during mobility. There were no signs of proximal lymphadenopathy, neurovascular impairment, or sinuses over the swelling. Laboratory test results were normal.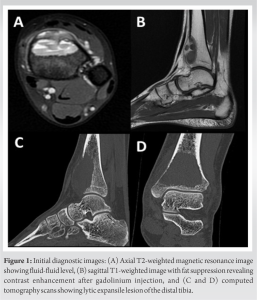
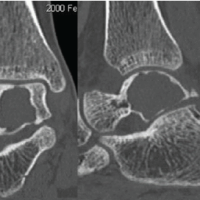
A 6- by 4-cm lytic expansile lesion was visible on the left ankle’s anteroposterior and lateral radiographs near the metaphysis of distal tibia (Fig. 1). Medial tibial cortical erosion was observed in the distal half of the lesion, and the lesion exhibited septations. Magnetic resonance imaging (MRI) revealed a heterogeneously expanding anterior lesion with intralesional septations and a fluid-fluid level but no epiphyseal plate ruptures (Fig. 1). Post-contrast images showed enhancement of the septa and surrounding areas.

An open incisional biopsy was performed to confirm the diagnosis of primary ABC and exclude other adjacent tumors that presented with secondary ABC or telangiectatic osteosarcoma. A histopathological analysis confirmed the diagnosis of primary ABC (Fig. 2). The surgical approach involved extensive curettage and bone filling using a combination of allografts and autografts. An anterior skin incision was used to expose the ankle joint. A large bone window was established and meticulous intralesional curettage of the cyst was performed using adjuvants such as a high-speed burr, argon, and hydrogen peroxide. The resulting bone defect was filled with a mixture of allografts and autografts (Fig. 3a and b). Postoperatively, the ankle was immobilized with a cam walking boot for 3 months. The patient was advised against weight-bearing for the first 2 months, while partial weight-bearing was recommended in the 3rd post-operative month. At the 3-month follow-up, she displayed full painless dorsiflexion and plantar flexion compared with the unaffected side. Radiography confirmed bone graft union (Fig. 3c and d), and full weight-bearing was initiated.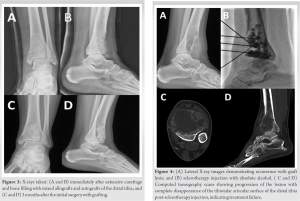
The patient’s post-operative recovery was promising. However, at 9 months post-operative, the pain recurred and osteolytic recurrence was observed on radiography. Subsequent investigations, including computed tomography (CT) and MRI, verified the ABC recurrence. Another surgical biopsy was conducted, and a histological analysis confirmed recurrent ABC. Given the aggressive behavior of the cyst, the patient underwent five sclerotherapy sessions with absolute alcohol (Fig. 4). However, due to its limited efficacy and due to progression of the lesion (Fig 5a and b), the patient’s case was discussed multiple times by our institution’s tumor board. The initial decision was to perform a distal tibial resection and reconstruction through ankle arthrodesis using a vascularized fibular graft. However, considering the patient’s young age and the potential adverse outcomes, the case was revisited by the French national tumor board. A final decision to administer denosumab was made. The treatment was initiated in April 2022. Dental check-ups preceded the denosumab therapy to assess the patient’s oral health. Denosumab 120 mg was subcutaneously injected as a loading dose on days 1, 8, 15, and 29, with monthly dosing thereafter. The patient was prescribed daily supplements of calcium 500 mg and Vitamin D 400 IU and her calcium levels monitored regularly. The patient reported no denosumab-related side effects during treatment. Partial ossification of the lesion was noted at 1 month after the start of the denosumab treatment, and complete ossification was achieved at 3 months (Fig. 5c and d). The patient managed to bear weight without crutches and was pain free. The treatment continued monthly for 1 year before being adjusted to once every 3 months. Twenty-2 months after the denosumab treatment and 34 months post-surgery until March 2024, regular imaging examinations showed no signs of recurrence (Fig. 5 e and f) [3].
ABC is a benign yet locally aggressive tumor with a frequent recurrence risk. Presentation at recurrence makes surgical options with bone/joint conservation difficult due to the absence of the cortex. In this case, the initial treatment decision was distal tibial resection with reconstruction using a vascularized fibular autograft and joint arthrodesis. Denosumab is an alternative treatment that demonstrates high efficacy. With its use, our patient was able to bear weight painlessly, the joint was conserved, and major surgical procedures were avoided. The initial treatment in this case involved curettage and lesion filling. However, with the recurrence of osteolysis, further interventions such as sclerotherapy and denosumab treatment became necessary. Multiple sclerotherapy sessions with absolute ethanol were conducted to induce fibrosis and promote bone healing. Although the patient’s initial response was unsatisfactory, denosumab was ultimately effective. Denosumab has shown promising results in the treatment of ABCs by inhibiting osteoclast activity and promoting bone healing. In the present case, the patient showed a favorable response to denosumab with improved ossification and decreased pain. ABCs can be treated locally with a variety of techniques, such as radiation, sclerotherapy, embolization, and surgery. Intralesional curettage is commonly considered the gold standard for ABC treatment. However, the recurrence rate after surgical treatment is reportedly 18–59% [11]. Surgical complications are notable owing to high morbidity rates, and the vascularity of ABCs can cause considerable intraoperative bleeding [5]. Percutaneous sclerotherapy is a favored alternative for the treatment of primary or recurrent ABCs after surgery, offering comparable success rates with less morbidity [6]. Several authors have used sclerotherapy as first-line treatment for ABCs. A recent review found similar success rates for sclerotherapy and surgery; however, surgery was associated with more complications and worse functional outcomes [4]. Novel therapeutics is required for ABCs, given the high risk of problems connected to conventional treatment choices. The US Food and Drug Administration (FDA) has authorized denosumab as a treatment for osteoporosis and skeleton-related symptoms in patients with bone metastases. Our findings are consistent with the theory that patients treated with RANKL-inhibiting denosumab may benefit significantly from having GCTBs as well as ABCs. Overall, clinical (symptom reduction) and radiological (tumor calcification) responses to denosumab treatment are beneficial for individuals with ABCs. Furthermore, denosumab has a safe pharmacological profile despite rare occurrences of hypocalcemia. However, denosumab use in ABCs is an off-label therapy that the FDA has not yet approved. The histological similarities of GCTBs and ABCs serve as a major justification for the use of denosumab therapy for the latter [3]. Although the number of treated patients to date is limited, recent reports support this concept. Pelle et al. documented the 12-month treatment with denosumab of a 5-year-old child with sacral ABC. The youngster experienced pain relief and improved neurological symptoms after a few weeks, and after 3 months, the tumor volume on an MRI was dramatically reduced [3]. After 19 months, a 21-year-old woman had a localized recurrence of a proximal forearm ABC, as reported by Pauli et al. Denosumab therapy helped to better outline the tumor with a bony rim, which also made surgery easier [10]. In two instances of children with spinal ABCs, Lange et al. reported that embolization failed, but that lesion healing, regression of neurologic impairments, pain relief, and tumor regression were all accomplished after four months of denosumab treatment [12]. Palmerini et al. observed clinical and radiological improvements, including pain reduction, bone formation on CT, and decreased gadolinium contrast uptake on MRI [13]. Overall, denosumab helps control tumor volume, making surgical procedures easier when used in a neoadjuvant setting. However, denosumab use carries a dose-dependent risk of osteonecrosis of the jaw in a small percentage of patients [14].
The management of recurrent ABCs can be challenging and requires a multidisciplinary approach that considers various treatment options. In the present case, curettage and filling, sclerotherapy, and denosumab treatment were sequentially administered to address the recurrent cyst in the left distal tibia. The use of denosumab yielded positive results, including enhanced ossification and pain reduction. The long-term safety and effectiveness of denosumab in the treatment of recurrent ABC need to be further investigated.
Denosumab is an option for treatment of recurrent ABC after in case of failure of surgical treatment and sclerotherapy. It shows promise in managing such cases effectively.
References
- 1.Restrepo R, Zahrah D, Pelaez L, Temple HT, Murakami JW. Update on aneurysmal bone cyst: Pathophysiology, histology, imaging and treatment. Pediatr Radiol 2022;52:1601-14. [Google Scholar | PubMed]
- 2.Tsagozis P, Brosjö O. Current strategies for the treatment of aneurysmal bone cysts. Orthop Rev (Pavia) 2015;7:6182. [Google Scholar | PubMed]
- 3.Pelle DW, Ringler JW, Peacock JD, Kampfschulte K, Scholten DJ 2nd, Davis MM, et al. Targeting receptor-activator of nuclear kappaB ligand in aneurysmal bone cysts: Verification of target and therapeutic response. Transl Res 2014;164:139-48. [Google Scholar | PubMed]
- 4.Bavan L, Wijendra A, Kothari A. Efficacy of treatment interventions for primary aneurysmal bone cysts: A systematic review. Bone Joint Open 2021;2:125-33. [Google Scholar | PubMed]
- 5.Rossi G, Mavrogenis AF, Papagelopoulos PJ, Rimondi E, Ruggieri P. Successful treatment of aggressive aneurysmal bone cyst of the pelvis with serial embolization. Orthopedics 2012;35:e963-8. [Google Scholar | PubMed]
- 6.Masthoff M, Gerwing M, Schneider KN, Köhler M, Deventer N, Schindler P, et al. Combined transarterial embolization and percutaneous sclerotherapy as treatment for refractory and nonresectable aneurysmal bone cysts. J Vasc Interv Radiol 2021;32:1425-34.e2. [Google Scholar | PubMed]
- 7.Strohm JA, Strohm PC, Kühle J, Schmal H, Zwingmann J. Management of juvenile and aneurysmal bone cysts: A systematic literature review with meta-analysis. Eur J Trauma Emerg Surg 2023;49:361-72. [Google Scholar | PubMed]
- 8.Li J, Liang J, Wu L, Xu Y, Xiao C, Yang X, et al. CYT387, a JAK-specific inhibitor impedes osteoclast activity and oophorectomy-induced osteoporosis via modulating RANKL and ROS signaling pathways. Front Pharmacol 2022;13:829862. [Google Scholar | PubMed]
- 9.Branstetter DG, Nelson SD, Manivel JC, Blay JY, Chawla S, Thomas DM, et al. Denosumab induces tumor reduction and bone formation in patients with giant-cell tumor of bone. Clin Cancer Res 2012;18:4415-24. [Google Scholar | PubMed]
- 10.Pauli C, Fuchs B, Pfirrmann C, Bridge JA, Hofer S, Bode B. Response of an aggressive periosteal aneurysmal bone cyst (ABC) of the radius to denosumab therapy. World J Surg Oncol 2014;12:17. [Google Scholar | PubMed]
- 11.Park HY, Yang SK, Sheppard WL, Hegde V, Zoller SD, Nelson SD, et al. Current management of aneurysmal bone cysts. Curr Rev Musculoskelet Med 2016;9:435-44. [Google Scholar | PubMed]
- 12.Lange T, Schulte TL. Answer to the Letter to the Editor of H. Namazi concerning “Denosumab: A potential new and innovative treatment option for aneurysmal bone cysts” by Lange T, Stehling C, Fröhlich B, Klingenhöfer M, Kunkel P, Schneppenheim R, Escherich G, Gosheger G, Hardes J, Jürgens H, Schulte TL (2013), Eur Spine J;22(6):1417-1422. Eur Spine J 2013;22:2343. [Google Scholar | PubMed]
- 13.Palmerini E, Ruggieri P, Angelini A, Boriani S, Campanacci D, Milano GM, et al. Denosumab in patients with aneurysmal bone cysts: A case series with preliminary results. Tumori 2018;104:344-51. [Google Scholar | PubMed]
- 14.Raje N, Terpos E, Willenbacher W, Shimizu K, García-Sanz R, Durie B, et al. Denosumab versus zoledronic acid in bone disease treatment of newly diagnosed multiple myeloma: An international, double-blind, double-dummy, randomised, controlled, phase 3 study. Lancet Oncol 2018;19:370-81. [Google Scholar | PubMed]
- 15.Maximen J, Robin F, Tronchot A, Rossetti A, Ropars M, Guggenbuhl P. Denosumab in the management of Aneurysmal bone cyst. Joint Bone Spine 2022;89:105260. [Google Scholar | PubMed]