Regional anesthesia is better and safer than general anesthesia for shoulder surgeries in the beach chair position, especially for high-risk group patients.
Dr. Vinay Jaiswal, Department of Anaesthesiology, L N C T. Medical College and Sewakunj Hospital, Indore, Madhya Pradesh, India. E-mail: drvinay.136@gmail.com
Introduction: Shoulder surgeries (arthroscopic or open) are usually performed under general anesthesia or combined with regional anesthesia. Post-operative pain following shoulder surgery is usually very severe and hinders early mobility of joints and recovery; which is also a cause of mental stress for the patient. Regional anesthetic techniques are known to provide excellent pain control postoperatively, both at rest and on movement. It allows faster recovery with earlier mobilization of joints. Profound knowledge of neural innervation of the shoulder is very essential to provide successful regional anesthesia for shoulder surgeries.
Case Reports: We underwent a case series of 10 patients with multiple comorbidities and were categorized as high-risk patients, posted for shoulder surgeries under regional anesthesia (PNS-guided interscalene brachial plexus block combined with suprascapular nerve block). Five out of ten patients were of the ASA 3 category, with multiple comorbidities. Shoulder surgeries (arthroscopic/open) were planned under regional anesthesia with mild sedation and resulted in better surgeon and patient satisfaction perioperatively.
Conclusion: Interscalene nerve block combined with suprascapular nerve block should be considered an alternative approach to general anesthesia for shoulder surgeries. Thus sole regional anesthesia can be considered a novel approach for all types of shoulder surgeries and is significantly safer for ASA Grade III and IV patients.
Keywords: Shoulder arthroscopy, shoulder surgery, regional anesthesia, peripheral nerve stimulation, suprascapular nerve block, interscalene nerve block.
The anesthesia of choice for shoulder surgery (arthroscopy, arthroplasty, and complicated trauma) is general anesthesia in consideration either alone or combined with regional anesthesia. Both arthroscopic (particularly rotator cuff repair and Bankart repair) and open shoulder surgeries cause moderate-to-severe post-operative pain. During rehabilitation, post-operative pain in many patients is severe, which is exacerbated by movement [1] (Fig. 1) and requires opioids for pain relief sometimes this severe pain leads to jerky movements at the shoulder joint in the post-operative period which might lead to failure of surgery. Regional anesthesia is an excellent choice for both intra-operative anesthesia and post-operative analgesia which improves patient’s comfort and enhances the recovery from surgery with more patient and surgeon satisfaction. Other advantages of regional anesthesia are:
- Regional anesthesia improves post-operative recovery time, earlier discharge thus reducing the cost of hospital stay
- Reduces post-operative pain and dosage of opioids thus decreasing the opioid-related side effects such as sedation, nausea, and vomiting [2]
- Complications of general anesthesia such as compromisation of the airway, respiratory, and cardiovascular physiology are avoided (including hypotension in the “beach-chair” position)
- Less perioperative complications, nausea and vomiting, etc.
- Reduced NPO time
- Earlier mobilization and recovery of joint.
The Institutional Ethics Committee permission for the case series was obtained. The mode of anesthesia and procedure was explained to the patients and valid informed consent was taken from the patients as per institution protocol. The cases were planned under regional anesthesia and the operative shoulder was prepared. The peripheral nerve stimulation-guided interscalene brachial plexus block with suprascapular nerve block for the operative shoulder was selected as the mode of anesthesia, to avoid any complication of general anesthesia in the beach chair/lateral position. A prepared combination of local anesthetic (total volume based on lean body weight) (lignocaine 2% + adrenaline1:200000 [7 mg/kg] + bupivacaine 0.5% [3mg/kg]) was calculated. 10 mL of the total calculated volume of local anesthetic mixture was used for suprascapular nerve block and 20 mL was given for interscalene brachial plexus block. After securing the I/V line, the patients were administered 4 mg of ondansetron, 1 mg of midazolam, and 50 mcg of fentanyl intravenously to alleviate anxiety and provide mild sedation. Intravenous tranexamic acid 1 g was given in 100 mL NS to all the patients to reduce bleeding at the surgical site.
PNS-guided interscalene brachial plexus block
The block is preferable for surgeries involving the shoulder, including the lateral two-thirds of the clavicle, proximal humerus, and shoulder joint [3]. The Winnie, classical anterior approach was used with nerve stimulation technique to give interscalene brachial plexus block [4]. The patient’s arm was placed in adduction. Under all aseptic precautions, a 50-mm 22 G peripheral nerve block needle was inserted in interscalene groove at the cricoid level using the initial current setting of 1.5 mA. Contraction of deltoid muscle elicited and current setting reduced to 0.5 mA. A total volume of 20 mL of the prepared combination of local anesthetic as described above was injected into the brachial plexus sheath. RAJ TEST POSITIVE [5] was confirmed.
PNS-guided suprascapular nerve block
For the suprascapular nerve block, the ideal approach ensures the blockade of the more proximal branches to the acromion and the subacromial region to maximize coverage. Meier technique [6] for the suprascapular nerve block was used. Needle insertion is 2 cm cephalad and 2 cm medial to the midpoint of a line connecting the lateral acromion and medial border of the spine of the scapula. The needle is angled 45° in the coronal plane, with 30° of ventral inclination. The target motor response of minor abduction (supraspinatus muscle contraction) and external rotation of the shoulder (infraspinatus muscle contraction at a low current of 0.5 mA achieved [7]). A total volume of 10 mL of the prepared combination of the local anesthetic was injected.
Case Summary
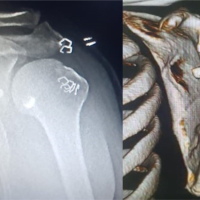
We are presenting a case series of a total 10 cases. Patients were aged between 50 and 75 years and weighed 40–70 kg. Out of eight; seven were male and three were female patients. ASA categorization of the patients was as follow: ASA I:-2, ASA II:-3, and ASA III:-5. Three patients were on antihypertensive and one was on oral hypoglycemics too. Indications for surgeries were tubercular synovitis of the shoulder joint, rotator cuff tear, and A-C joint dislocation. Seven patients were planned for arthroscopic repair and three for open shoulder surgeries under regional anesthesia (PNS-guided interscalene brachial plexus block combined with suprascapular nerve block). All patients were pre-medicated with intravenous ondansetron 4 mg + midazolam 1 mg + fentanyl 50 mcg. All cases were done in beach chair position, skin incision was given 15–20 min after giving regional anesthesia, and two to six ports (one anterior and one posterior port and others as required according to surgery planned) were inserted without any discomfort to the patient and arthroscopic surgery proceeded successfully. Intravenous paracetamol 1 g + tramadol 100 mg + loxicard 63 mg was added to relieve the complaint of positional discomfort whenever required. Only two out of ten patients needed nitroglycerine infusion intraoperatively to control blood pressure to get a clear bloodless field of vision during arthroscopy. (Fig. 2). Two of the patients, who were posted for open shoulder surgery for AC joint dislocation, had complaints of mild pain during manipulation of the coracoid process; this particular complaint was resolved with intravenous Ketofol and surgery proceeded comfortably. Rest surgeries were completed comfortably with the duration of surgery ranging from 1 to 1/2–3 h. All patients were shifted to the intensive care unit for observation and then to the orthopedic ward the next day. The intraoperative and 24-h Visual Analog Scale for pain scores did not exceed four in any of the patients.
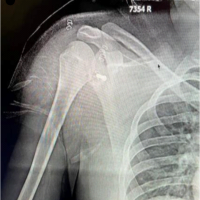
The position of two to six ports needed in shoulder arthroscopy depends on the surgery planned. A posterior port is the main viewing port which is inferiomedial to the posterolateral aspect of the acromion. The location of other ports varies depending on the plan of surgery for ease of joint instrumentation [8]. General anesthesia is always considered the most common technique of anesthesia for shoulder surgeries and results in the reversible state of unconsciousness [9]. General anesthesia requires monitoring at a more advanced level, vigilance for changes in the patient’s vital signs, and adequate ventilation with the correct position of an endotracheal device. Suppression of physiological autonomic functions, including cardiac and respiratory responses is another challenge during general anesthesia [10].(Fig.3). Older and sicker patients are at greater risk of associated complications of general anesthesia, such as cardiovascular and respiratory complications which include, myocardial infarction, pulmonary function interference, and pre-existing pathological state aggravation. Post-operative cognitive dysfunction and acute renal impairment are the long-term adverse effects encountered with general anesthesia [11]. Regional anesthesia provides benefits of better post-operative analgesia at rest and on mobility, respectively, reduced incidence of muscle spasms, help in earlier mobilization, and increased comfort level of the patient during physiotherapy. Therefore, regional anesthesia has excellent results in both improved patient recovery and outcome postoperatively in both open and arthroscopic surgeries. It decreases the complications of general anesthesia as well. The peripheral nerve stimulation technique for interscalene block can be considered to be safer over the blind technique in patients with compromised state of lungs. Suprascapular nerve block is considered to be a mode of analgesia and supplement for procedures where interscalene block is either not technically possible or contraindicated. It is believed that this modality only blocks a proportion of the afferent input from the shoulder joint and is therefore substantially inferior to the interscalene block. In addition, it is also believed that it is not sufficient to provide cutaneous analgesia; therefore, local anesthetic are infiltrated around the incision site when suprascapular nerve block is performed [12], but in our case series we found excellent cutaneous analgesia; and there was no need of local infiltration for the posterior port insertion during arthroscopy.
In this case series, though the number of cases are less, it was demonstrated that the PNS-guided interscalene block with suprascapular nerve block can safely be applied for both anesthesia and analgesia in arthroscopic shoulder surgeries, it can be a part of routine surgical anesthesia for ASA1-2 and very much beneficial in ASA III/IV patients. In our case series, we found it to be completely beneficial to patients, intraoperatively and postoperatively, and a high grade of satisfaction to both surgeon and patient with a comparatively clear field of arthroscopic view. We did not encounter any side effects of these techniques. Further prospective randomized control will ensure the safety of this block and need a larger number of case series documentation for the same.
- Regional anesthesia is a better alternative to general anesthesia in patients with compromised cardiopulmonary reserve and high-risk patients
- Regional anesthesia is cost-effective due to enhanced recovery, lesser hospital stay, and excellent post-operative analgesia.
References
- 1.Bowens C Jr., Sripada R. Regional blockade of the shoulder: Approaches and outcomes Department of Anesthesiology, Vanderbilt University School of Medicine. Anesthesiol Res Pract 2012;2012:971963. [Google Scholar | PubMed]
- 2.Lee BH, Qiao WP, McCracken S, Singleton MN, Goman M. Regional anesthesia techniques for shoulder surgery in high-risk pulmonary patients. J Clin Med 2023;12:3483. [Google Scholar | PubMed]
- 3.Borgeat A, Ekatodramis G. Anaesthesia for shoulder surgery. Best Pract Res 2002;16:211-25. [Google Scholar | PubMed]
- 4.Winnie AP. Interscalene brachial plexus block. Anesth Analg 1970;49:455-66. [Google Scholar | PubMed]
- 5.Montgomery SJ, Raj PP, Nettles D, Jenkins MT. The use of the nerve stimulator with standard unsheathed needles in nerve blockade. Anesth Analg 1973;52:827-31. [Google Scholar | PubMed]
- 6.Meier G, Bauereis C, Maurer H. The modified technique of continuous suprascapular nerve block. A safe technique in the treatment of shoulder pain. Anaesthesist 2002;51:747-53. [Google Scholar | PubMed]
- 7.Gray H. Anatomy of the Human Body. 20th ed. Philadelphia, PA: Lea and Febiger; 1918. [Google Scholar | PubMed]
- 8.Hewson DW, Oldman M, Bedforth NM. Regional anaesthesia for shoulder surgery. BJA Educ 2019;19:98-104. [Google Scholar | PubMed]
- 9.Gargano F, Migliorelli S, Strumia A, Carassiti M, Agrò FE. Evolution of anesthetic techniques for shoulder surgery: A narrative review. Osteology 2022;2:52-61. [Google Scholar | PubMed]
- 10.Brown AR, Weiss R, Greenberg C, Flatow EL, Bigliani LU. Interscalene block for shoulder arthroscopy: Comparison with general anesthesia. Arthroscopy 1993;9:295-300. [Google Scholar | PubMed]
- 11.Mason SE, Noel-Storr A, Ritchie CW. The impact of general and regional anesthesia on the incidence of post operative cognitive dysfunction and post-operative delirium: A systematic review with meta-analysis. J Alzheimers Dis 2010;22:101086. [Google Scholar | PubMed]
- 12.Singelyn F, Lhotel L, Fabre B. Pain relief after arthroscopic shoulder surgery: Comparison of intra-articular analgesia, suprascapular nerve block and inter scalene brachial plexus block. Anesth Analg 2004;99:589-92. [Google Scholar | PubMed]