Proximal Tibial sMCL detachment and Medial Meniscus extrusion can be used as prognostic factors for the progression of knee Osteoarthritis
Dr. Aniket Wagh, Department of Orthopedics, Murup Hospital, Changwon, South Korea. E-mail: muruphospital@gmail.com
Introduction: The aim of the study is to assess the correlation of detachment of proximal tibia superficial medial collateral ligament (sMCL) and medial meniscus (MM) extrusion with knee osteoarthritis (OA) and its progression.
Materials and Methods: This is a prospective study where 165 knees were evaluated using radiographs and magnetic resonance imaging for the severity of OA knee according to Kellgrence-Lawrence grading, MM extrusion, and status of proximal tibia attachment of sMCL. Chi-square test of Independence and Pearson’s correlation test were used to assess any correlation among the variables.
Results: The study population had a mean age of 52.93 19.46 years. 106 (64.24%) were males and 59 (35.75 were females. There were 83 (50.30%) left knees and 82 (49.70%) right knees in the study. The percentage of proximal tibia sMCL detachment was more in patients with knee OA than those without OA (85–88.89%). Similarly, the percentage of MM extrusion was maximum in advanced arthritis patients (95%). Both these variables were lowest in non-arthritic group (2.56% and 6.41%, respectively). Statistical analysis showed a significantly positive correlation of detachment of proximal tibial attachment of sMCL as well as MM extrusion with grades of OA of knee (P < 0.001 for both).
Conclusion: A detached proximal tibia sMCL and an extruded MM were individually found to have a strong association (Chi-square test) and a positive linear correlation (Pearson’s test) with the arthritic condition of the knee. This would suggest a role of both these variables in the progression of knee OA. They can thus be used as prognostic markers for knee OA as well as an important target in the management of knee OA.
Keywords: Meniscus extrusion, superficial medial collateral ligament, osteoarthritis knee, superficial medial collateral ligament, medial meniscus, prognostic factors, OA progression.
Knee osteoarthritis (OA) is the most common chronic joint disease in the world, affecting the articular cartilage and exposing the subchondral bone [1]. There is progressive pain, stiffness, and reduced mobility, eventually deteriorating the joint function [2]. Along with affecting the quality of life of the patients, OA also poses a burden on global public health [3]. Depending on the grade of OA, there is a battery of treatments available, namely conservative treatment with medications and physiotherapy; minor interventions such as intra-articular steroids, platelet-rich plasma, prolotherapy, and viscosupplementation; and surgical interventions such as chondroplasty, osteotomies, and lastly partial or total knee replacement. Most of the times, orthopedicians are required to make these judgments based on analysis of risk factors, symptoms, signs, and results of imaging and laboratory examinations [4]. However, there are instances where selection of adequate treatment becomes dilemmatic due to factors such as clinic-radiological mismatch, borderline age group, and obesity. [5]. Therefore, identifying specific diagnostic and prognostic parameters for knee OA has become the need of the hour. In literature, many parameters such as hyaluronic acid level, baseline radiographic reduction in joint space, quadriceps strength, gender, general activity level, and previous knee injury have been associated with OA prognosis [6]. It is often observed that magnetic resonance imaging (MRI) showing arthritic changes in the knee also shows concomitant morphological changes in the proximal tibial attachment of superficial medial collateral ligament (sMCL) and medial meniscus (MM) extrusion to some extent. However, there is no substantial research that links non-traumatic changes in proximal tibia sMCL with knee OA. Similarly, more studies are needed to establish a linear relationship between MM extrusion and generalized knee OA. Medial collateral ligament (MCL) is the most commonly injured knee ligament [7]. The superficial layer of the MCL (sMCL), being the prime medial stabilizer, comprises anterior fibers that are oriented vertically and attach to proximal tibia at 12 mm distal to articular surface (proximal attachment) and 6 cm distal to articular surface (distal attachment) [8,9]. MM is a crescent-shaped fibrocartilage in the knee functioning toward balanced force transmission, joint stability, joint congruity and lubrication [10,11]. The collagen fibers in the meniscus are specifically aligned in a circumferential manner (hoop structure), which creates a biomechanical resistant against hoop stresses during weight bearing [12,13]. Our study aims to comprehensively investigate and find a possible correlation between proximal tibia sMCL detachment and MM extrusion with knee OA.
Patients with chronic as well as recent onset knee pain were included in the study with valid consents and evaluated with routine knee radiographs and MRI. Those with a history of trauma or previous invasive interventions in the knee were excluded. We managed to enroll 165 patients in our study. Routine radiographs comprised of standing antero-posterior and lateral views. These were evaluated for OA, if any, according to Kellgrence-Lawrence (K-L) grading system. Knee MRI was evaluated for MM extrusion and status of proximal tibial attachment of sMCL (attached or detached).
MRI assessment
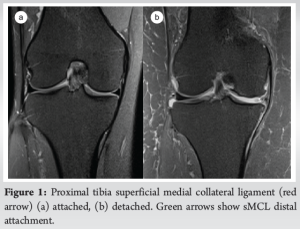
sMCL was assessed in coronal plane, and the proximal attachment (approximately 12 mm from joint line) was observed whether attached or detached (Fig. 1).
MM was assessed in a coronal plane on a slice with the widest tibial plateau. It was considered extruded if it was displaced beyond the outermost border of the tibial plateau in mid-coronal plane [14]. The authors have devised a novel classification for easier understanding of the severity of meniscus injuries (Fig. 2).

Grading of meniscal injury
Grade 0: No injury (intact meniscus)
Grade 1: Meniscus tear present without extrusion
Grade 2: Limited meniscal extrusion with or without tear
Grade 3: Definite meniscal extrusion (defined as complete extrusion of meniscus beyond the line joining ends of articular surface of femoral and tibial condyles).
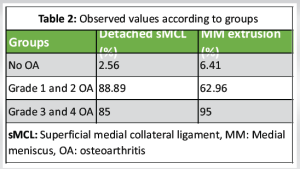
Grades 2 and 3 were considered in the MM extrusion group during the statistical analysis. Subjects were divided into 3 groups – No OA (K-L grade 0), mild-to-moderate OA (K-L grade 1, 2), and advanced OA (K-L grade 3, 4). Each group was studied for MM extrusion and proximal tibia sMCL status. Chi-square test of independence and Pearson’s correlation test were used to establish possible association of these 2 variables with OA knee.
A total of 165 patients were studied. The mean age of the study population was 52.93 ± 19.46 years. 106 (64.24%) were males and 59 (35.75%) were females. There were 83 (50.30%) left knees and 82 (49.69%) right knees. 78 (47.27%) patients had no OA (K-L grade 0). 27 (16.36%) had mild-to-moderate OA (grade 1 or 2). 60 (36.36%) patients had advanced OA (Grade 3 or 4) (Table 1). It was observed that the incidence of proximal tibia sMCL detachment was significantly higher in arthritic knees (85–88.89%) than in non-arthritic ones (2.56%). Similarly, MM extrusion was seen to be more in higher grades of OA (62.96–95%) as compared to no OA group (6.41%) (Table 2).

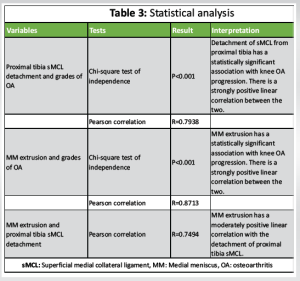
Statistical analysis (Table 3)
- According to Chi-square test of Independence and Pearson’s correlation test, detachment of proximal tibia sMCL had a high statistically significant association and a strong positive correlation with the severity of OA knee (P < 0.001 and r = 0.7938). In other words, knees with detached proximal tibia sMCL had more severe OA progression.
The Chi-square statistic was 115.7194 with degree of freedom 2
χ² (2, n = 165) = 115.72, P < 0.001
The coefficient of determination (r2) was 0.6301
r (163) = 0.79, P < 0.00001
- MM extrusion showed similar correlation with OA which was strongly positive and highly significant (P < 0.001 and r = 0.8713). This signifies that more the extrusion of MM, higher would be the OA grades.
The Chi-square statistic was 109.5972 with degree of freedom 2
χ² (2, n = 165) = 109.5972, P <0.001
The coefficient of determination (r2) was 0.7592
r (163) = 0.87, P < 0.00001
- In addition, Pearson’s correlation test also showed a moderately positive correlation of MM extrusion with proximal tibial sMCL detachment (r = 0.7494). In other words, proximal tibia sMCL detachment increases the chances of MM extrusion.
The coefficient of determination (r2) was 0.5616
r (163) = 0.74, P < 0.00001.
The objective of this study is to establish proximal tibia sMCL detachment and MM extrusion as possible risk factors and prognostic variables for the progression of OA. The statistical analysis showed a significant and valid correlation supporting the above hypothesis. It is clear in the findings that higher grades of OA have higher chances of proximal tibia sMCL detachment and more MM extrusion. There are no previous studies linking detachment of proximal tibial sMCL directly to OA grades with such a remarkably positive correlation. In 2015, Bastick et al. summarized numerous patient-related and disease-related prognostic factors such as bone marrow lesions, flexion contractures, subchondral cysts, and synovitis toward OA progression. However, proximal tibia sMCL detachment was not among them. Moreover, meniscal damage and extrusion could not be significantly associated with the disease [15]. Bierma-Zeinstra and Koes in their study found that there was a moderate to strong association of serum levels of hyaluronic acid with knee OA progression [16]. However, no other factors were found to have stronger evidence of being OA prognostic markers. Heidari in his article in 2011 stated that joint laxity along with other factors could be considered for the prognosis of knee OA [17]. Similarly, another article by Sharma et al. found increased laxity as a strong prognostic factor for OA knee progression [18]. Lewek et al. stated that patients with significant medial knee laxity had high prevalence of OA than those with no laxity [19]. On the same lines, Conaghan et al. postulated that weak or damaged ligaments would lead to untoward laxity, causing abnormal weight distribution. This would ultimately damage the articular cartilage and cause OA [20]. The above examples make it clear that in the past, no research has been done to specifically study the status of proximal tibia sMCL attachment along with MM extrusion and correlate them both to the progression of knee OA. The author has previously researched and published a study concluding that a detached sMCL proximal tibial attachment can be a strong predictor of OA knee progression [21]. This article studies a wider aspect and includes MM extrusion along with proximal tibia sMCL detachment to correlate with knee OA. This makes the study unique and gives researchers a vital thought to do further research upon. Swamy et al. in 2018 stated that an extruded meniscus is not just a meniscal injury but can be an expression of other pathologies such as cartilage loss, ligament injuries, or OA [14]. Crema et al., in their article, concluded that meniscal extrusion could probably result from complex interactions between joint tissues and mechanical stresses in the OA process [22]. A recent prospective cohort study by Zeng et al. suggests that MM extrusion can be considered as a predictor of structural progression of knee OA [23]. In 2005, Kamekura et al., in their brilliant experiment, studied the direct effects of transection of various ligaments of the knee on knee cartilage in mice [24]. They found that the combination of MCL transection and medial meniscectomy caused cartilage destruction and osteophyte formation in the medial tibial plateau. Histological examination showed proliferation and shape change of chondrocytes at 2–4 weeks, cartilage destruction into the middle zone at 8 weeks, and osteophyte formation at 12 weeks. This article substantially supports our study and its results align with our finding that detachment of proximal tibial attachment of sMCL and MM extrusion contributes to progression of knee OA.
Meniscus extrusion was studied in supine MRI which might be more on a weight-bearing study. Mechanical axis malalignment, which could be associated with OA knee progression, was not studied. Furthermore, MRI being an expensive modality, this evaluation would be costly and cumbersome.
Proximal tibial sMCL detachment and MM extrusion were statistically found to be significantly associated with knee OA and thus can be used as prognostic predictors for the progression of OA. Since these two variables are statistically interdependent, they can also be considered as medial menisco-ligamentous complex failure, which can prognosticate about knee OA. A keen identification of the status of proximal tibia sMCL attachment might help us judge the laxity of the knee and aid in decision-making while treating that knee conservatively as well as surgically. Similarly, correct diagnosis of MM extrusion and early repair of the associated lesion can slowdown OA progression and increase success rates of conservative treatments. As a future prospect, these measures in turn can lead to less number of prosthetic replacements and significantly benefit the quality of life of the patient and economy of the health system.
A detached proximal tibia sMCL with extruded meniscus suggests an accelerated OA progression. Identifying these variables can help surgeons to decide about early interventions for preserving the knee, thus reducing the chances of future prosthetic replacements.
References
- 1.Al-Mhanna SB, Mohamed M, Mohd Noor N, Aldhahi MI, Afolabi HA, Mutalub YB, et al. Effects of circuit training on patients with knee osteoarthritis: A systematic review and meta-analysis. Healthcare (Basel) 2022;10:2041. [Google Scholar | PubMed]
- 2.He Y, Li Z, Alexander PG, Ocasio-Nieves BD, Yocum L, Lin H, et al. Pathogenesis of osteoarthritis: Risk factors, regulatory pathways in chondrocytes, and experimental models. Biology (Basel) 2020;9:194. [Google Scholar | PubMed]
- 3.Dawson J, Linsell L, Zondervan K, Rose P, Carr A, Randall T, et al. Impact of persistent hip or knee pain on overall health status in elderly people: A longitudinal population study. Arthritis Rheum 2005;53:368-74. [Google Scholar | PubMed]
- 4.Geng R, Li J, Yu C, Zhang C, Chen F, Chen J, et al. Knee osteoarthritis: Current status and research progress in treatment (Review). Exp Ther Med 2023;26:481. [Google Scholar | PubMed]
- 5.Gossec L, Paternotte S, Maillefert JF, Combescure C, Conaghan PG, Davis AM, et al. The role of pain and functional impairment in the decision to recommend total joint replacement in hip and knee osteoarthritis: An international cross-sectional study of 1909 patients. Report of the OARSI-OMERACT Task Force on total joint replacement. Osteoarthritis Cartilage 2011;19:147-54. [Google Scholar | PubMed]
- 6.Belo JN, Berger MY, Reijman M, Koes BW, Bierma-Zeinstra SM. Prognostic factors of progression of osteoarthritis of the knee: A systematic review of observational studies. Arthritis Rheum 2007;57:13-26. [Google Scholar | PubMed]
- 7.Lind M, Jakobsen BW, Lund B, Hansen MS, Abdallah O, Christiansen SE. Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. Am J Sports Med 2009;37:1116-22. [Google Scholar | PubMed]
- 8.Standring S, editor. Gray’s Anatomy. 41st ed. Philadelphia, PA: Elsevier; 2016. [Google Scholar | PubMed]
- 9.LaPrade MD, Kennedy MI, Wijdicks CA, LaPrade RF. Anatomy and biomechanics of the medial side of the knee and their surgical implications. Sports Med Arthrosc Rev 2015;23:63-70. [Google Scholar | PubMed]
- 10.Makris EA, Hadidi P, Athanasiou KA. The knee meniscus: Structure-function, pathophysiology, current repair techniques, and prospects for regeneration. Biomaterials 2011;32:7411-31. [Google Scholar | PubMed]
- 11.Andrews S, Shrive N, Ronsky J. The shocking truth about meniscus. J Biomech 2011;44:2737-40. [Google Scholar | PubMed]
- 12.Fox AJ, Bedi A, Rodeo SA. The basic science of human knee menisci: Structure, composition, and function. Sports Health 2012;4:340-51. [Google Scholar | PubMed]
- 13.Bullough PG, Munuera L, Murphy J, Weinstein AM. The strength of the menisci of the knee as it relates to their fine structure. J Bone Joint Surg Br 1970;52:564-7. [Google Scholar | PubMed]
- 14.Swamy N, Wadhwa V, Bajaj G, Chhabra A, Pandey T. Medial meniscal extrusion: Detection, evaluation and clinical implications. Eur J Radiol 2018;102:115-24. [Google Scholar | PubMed]
- 15.Bastick AN, Runhaar J, Belo JN, Bierma-Zeinstra SM. Prognostic factors for progression of clinical osteoarthritis of the knee: A systematic review of observational studies. Arthritis Res Ther 2015;17:152. [Google Scholar | PubMed]
- 16.Bierma-Zeinstra SM, Koes BW. Risk factors and prognostic factors of hip and knee osteoarthritis. Nat Clin Pract Rheumatol 2007;3:78-85. [Google Scholar | PubMed]
- 17.Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian J Intern Med 2011;2:205-12. [Google Scholar | PubMed]
- 18.Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: Role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum 2003;48:3359-70. [Google Scholar | PubMed]
- 19.Lewek MD, Rudolph KS, Snyder-Mackler L. Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthritis Cartilage 2004;12:745-51. [Google Scholar | PubMed]
- 20.Conaghan PG, D’Agostino MA, Le Bars M, Baron G, Schmidely N, Wakefield R, et al. Clinical and ultrasonographic predictors of joint replacement for knee osteoarthritis: Results from a large, 3-year, prospective EULAR study. Ann Rheum Dis 2010;69:644-7. [Google Scholar | PubMed]
- 21.Jung Wh, Roy S, Takeuchi R. Can status of superficial medial collateral ligament proximal tibial attachment predict progression of OA knee? J Orthop 2024;51:137-41. [Google Scholar | PubMed]
- 22.Crema MD, Roemer FW, Felson DT, Englund M, Wang K, Jarraya M, et al. Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: The multicenter osteoarthritis study. Radiology 2012;264:494-503. [Google Scholar | PubMed]
- 23.Zeng M, Cicuttini FM, Wluka AE, Jones G, Hill CL, Ding C, et al. Association between medial meniscal extrusion and knee structural progression in adults with symptomatic knee osteoarthritis - a prospective cohort study. Skeletal Radiol 2024;4;Jun 15, https://doi.org/10.1007/s00256-024-04731-2. [Google Scholar | PubMed | CrossRef]
- 24.Kamekura S, Hoshi K, Shimoaka T, Chung U, Chikuda H, Yamada T, et al. Osteoarthritis development in novel experimental mouse models induced by knee joint instability. Osteoarthritis Cartilage 2005;13:632-41. [Google Scholar | PubMed]