This study highlights the importance of surgical intervention in appropriate candidates with medial meniscal root tear to prevent progression to osteoarthritis.
Dr. Krishnavel Thavasianantham, Chettinad Hospital and Research Education, Chettinad Academy of Research and Education, Kelambakkam, Tamil Nadu, India. E-mail: krishna08vel@gmail.com
Introduction: To sustain hoop stress, prevent extrusion, and maintaining the function of the meniscus, the posterior root attachment point of the medial meniscus is essential. The purpose of this study is to determine the functional and radiological outcome of conservative therapy and meniscal repair for medial meniscal root tears.
Materials and Methods: Prospective evaluations were performed on forty individuals who confirmed a diagnosis of Medial meniscus root tear (MMRT). Among the 40 patients, 20 underwent arthroscopic meniscal repair and 20 underwent conservative management and followed up a period of 2 years. Functional outcome between two groups was measured using Tegner Lysholm score and IKDC score. Radiological outcome was measured using X-rays (medial joint space width, joint space narrowing, K-L grade).
Results: Both group showed improvement in Lysholm score and IKDC. When comparing the clinical outcomes between both the groups, Group A showed significantly better outcome (P = 0.02). About 60% of patients in Group A and all patients in Group B showed K-L grade progression. Of the patients in Group A, 5% had significant K-L grade progression and 10% had severe joint space constriction. Of the patients in Group B, 80% had significant K-L grade progression and 25% had severe joint space constriction. Meniscal repair had considerably superior outcomes for radiologic parameters than conservative care (P < 0.01) when we examined the final results of Groups A and B.
Conclusion: The MMRT repair group had better functional and radiological outcome than the conservative treatment group. Although treatment did not entirely stop the advancement of arthrosis, meniscal repair decreased the rate of arthritic changes when compared to the conservative group.
Keywords: Knee, meniscal root tear, arthroscopic repair, meniscal root repair, pull-out repair, conservative management.
The fundamental functions of the meniscus include stabilization, proprioception, load distribution, stress absorption, and lubrication [1]. Load distribution is one of the important roles to prevent deterioration of articular cartilage. This occurs due to the collagen fibers that are arranged circumferentially; these fibers have a propensity to stretch centrifugally while under-weight, resulting in hoop tension [2]. The definition of a medial meniscal root tear (MMRT) is a radial tear that occurs within 5 mm of the posterior bony attachment of the medial meniscus. The posterior bony attachment of the medial meniscus is situated between the PCL’s insertion and the medial tibial spine as well as the articular border of the posteromedial tibial plateau [3,4]. Through the meniscal roots, the meniscus is securely fixed to the tibial plateau [5,6]. The containment of this hoop tension results in a balanced distribution of axial-loading forces within the knee joint, protecting the articular cartilage [1]. Asians are more prone to have radial tears at the posterior horn of the medial meniscus, which is the most common site of meniscal injury [7]. The hoop tension, which is essential for preventing meniscal extrusion, may change depending on the nature of the tear, which is frequently depicted as a full transection [5]. According to biomechanical research, MMRT has comparable effects to complete meniscectomy, which causes the medial compartment of the knee joint to develop degenerative arthritis [9-11]. As with other radial meniscal tears, MMRT has traditionally been treated with a straightforward meniscectomy; however, this did not stop the osteoarthritis from progressing [8]. Recent biomechanical studies indicate that corrected MMRT brought the peak contact pressure back to a level that was close to normal [9-12]. In biomechanical research, numerous techniques for repairing MMRT have been reported [13-16], and clinical trials are being carried out to determine the outcomes of MMRT repair [17,18]. These findings, however, are rather ambiguous, and several studies are being conducted to identify the MMRT repair prognostic variables [19]. In addition, conservative therapy might not be beneficial based on biomechanical outcomes [9,20]. Factors such as age, gender, body mass index, and cultural environment were associated with a high likelihood of negative outcome [21]. There are, however, a few publications on prognostic factors linked to subpar clinical outcomes following MMRT repair [19]. In this study, the functional and radiological outcomes of conservative therapy and pull-out repair of the MMRT are compared.
Prospective evaluations were performed on 40 individuals who confirmed a diagnosis of MMRT radiologically. Inclusion criteria were Age between 25 and 60 years, Kellgren-Lawrence Grade 1 and 2, onset of symptoms <6 months, and radiologically confirmed meniscal root tear. The patient who underwent arthroscopic meniscal root repair (Transosseous suture pull-out technique) was termed as Group A and the patient treated conservativity (pain control, strengthening exercise, and physical therapy) was termed as Group B. Functional and radiological outcome were recorded pre- and postoperatively for 2 years.
Treatment methods
Group-A
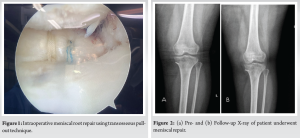
Under spinal anesthesia, the patient was placed in the supine position. Using standard anteromedial and anterolateral knee arthroscopic portal diagnostic arthroscopy was done. Medial meniscal root tear was confirmed. Two simple sutures were placed in the posterior horn with a gap of 5 mm. Footprint of meniscal root was prepared, and articular cartilage was removed from the footprint. Transosseous tibial tunnel was created using a PCL guide. Guide wire was retrieved from the footprint of meniscal root. Sutures were then passed through the tunnel and pulled through the tibia and fixed to the anterior tibia using an endobutton. Stability of the repair was checked using the probe, and the position of the fixation was confirmed (Fig. 1). Closure was done. Postoperatively, the patient was mobilized non-weight-bearing for period of 4 weeks. Gradual tolerated weight-bearing was started from 5 weeks post-operative.
Group B
The patient was managed conservatively with analgesics, quadriceps strengthening exercise, wax bath/IFT to knee, and lifestyle modifications such as avoiding stair climbing, cross-leg sitting, and squatting.
Statistical analysis
The demographic data within the groups were compared using the Chi-square test and expressed as mean (±standard deviation). The Mann–Whitney test was used to compare the groups, while the Wilcoxon rank-sum test was used to compare within the groups. This statistical test was two-tailed, with a significance threshold of P < 0.05. Statistical Package for the Social Science (SPSS) Version 26 was used for all statistical analyses (IBM, SPSS Statistics, Armonk NY, USA)
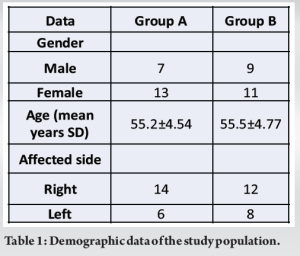
In Group A, the mean age was 55.2 ± 4.54 with 7 males and 13 females. In Group B, the mean age was 55.5 ± 4.77 with 9 males and 11 females (Table 1). The pre-operative clinical and demographic features of Groups A and B did not have statistically significant difference.
Functional outcome
Both the groups showed improvement in Lysholm score and IKDC score during follow-up.
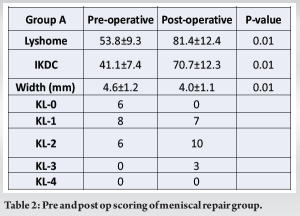
In Group A, Lysholm score improved from 53.8 ± 9.3 (pre-operative) to 81.4 ± 12.4 (post-operative) (P < 0.01) and IKDC score improved from 41.1 ± 7.4 (pre-operative) to 70.7 ± 12.3 (post-operative) (P < 0.01) (Table 2).
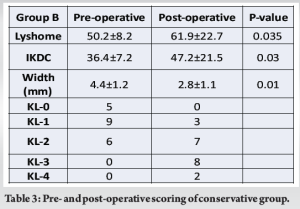
In Group B, Lysholm score improved from 50.2 ± 8.2 (pre-op) to 61.9 ± 22.7 (post-operative) (P = 0.035) and IKDC score improved from 36.4 ± 7.2 (pre-operative) to 47.2 ± 21.5 (post-operative) (P = 0.030) (Table 3).
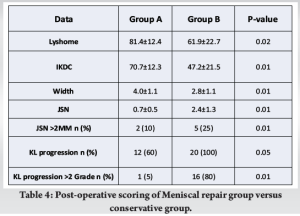
When comparing the clinical outcomes between both the groups, Group A showed significantly better outcome (P = 0.02) (Table 4).
Radiological outcome
K-L grade progression was seen in 60% of individuals in group A (12/20) and in 100% of patients in Group B (20/20). At the end follow-up, both groups’ medial joint space width and K-L grade were significantly lower (Group A P < 0.01, Group B < 0.01) (Table 2).
About 10% of the patients (2 out of 20) in Group A exhibited significant joint space narrowing (>2 mm), and 5% (1 out of 20) had severe K-L grade progression (>2 grades). 25 percent of the patients in Group B (5 out of 20) had significant joint space narrowing (>2 mm), and 80 percent (16 out of 20) had severe K-L grade progression (>2 grades) (Table 3).
Meniscal repair had substantially superior outcomes for radiologic measures than conservative therapy when we examined the end results of Groups A and B (P < 0.01) (Table 4).
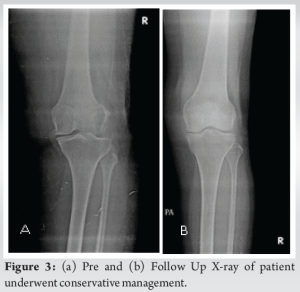
In addition, osteoarthritis development was markedly slowed in the meniscal repair group (Fig. 2 and 3).
When there is a loss of integrity in one of the root ligaments, the meniscus circumferential collagen fibers lose their continuity, which finally results in a loss of hoop tension [5,10,11]. This meniscus issue contributes to meniscal extrusion, which causes gradual cartilage degradation [22]. As opposed to the other meniscal roots, the posterior root of the medial meniscus is very brittle and more prone to injury [6,23]. The one probable factor contributing to the high frequency of MMRT in Asian cultures is the cultural mandate to sit with hyper flexed knees. Far Eastern people than the rest of the globe have posterior root tear of the medial meniscus significantly more frequently [8,23]. The ability of magnetic resonance imaging (MRI) to identifying a tear of the posterior horn of the medial meniscus has been shown to be highly sensitive in earlier investigations [24,25]. On MRI, et al [7]. found only 68% sensitivity for radial tears, while Bin et al. [8] found that the sensitivity for posterior root tears of the medial meniscus was 66.3%. According to reports from Lee et al. [18] and Moon et al. [19], the average Lysholm knee score saw an improvement from 57.0 to 93.1 and 48.3 ± 13.7 to 83.2 ± 16.1 (P < 0.001), respectively [3,18,19]. In addition, Moon et al. observed that a worse clinical result of MMRT repair was shown to be independently associated with extensive cartilage deterioration (Outerbridge Grade III or IV). The primary source of mechanical discomfort in patients with a posterior root tears of the medial meniscus, including those who were old, was successfully treated with a partial meniscectomy by Bin et al. [8]. They came to the conclusion that due to the age-related degeneration of meniscal tissue and the poor healing capacity of a posterior root tear of the medial meniscus, restoration is nearly impossible. Arthroscopy-guided MMRT repair is a commonly utilized procedure for re-establishing hoop tension and preventing osteoarthritis. Nowadays, there are several surgical techniques available for repairing a posterior root tear of the medial meniscus [13-15]. Considering two factors, the first being the posterior root of the meniscus is an enthesis with strong healing potential and that the posterior horn of the medial meniscus has an adequate vascular supply, Double bundle transosseous pull-out suture techniques were previously reported by Ahn et al. [14] as a means of anchoring the posterior horn. Kim et al. have also talked about the transosseous technique, which uses a Caspari suture hook and shuttle through the meniscus’s anteromedial portal [16]. This method helps to enhance healing by preventing red-red zone tissues from easily rupturing. A method of all-inside repair using metal suture anchors was described by Choi et al. in their study [27]. A pull-out repair procedure employing a transosseous tunnel and fastening with a button at the anterior tibial cortex was proposed by Petersen and Zantop [28]. Much like in previous research [8,18], the majority of patients in our group developed mechanical pain around the posteromedial side of the knee fairly rapidly,probably squatting or kneeling was the specific motion that caused this pain. The biomechanical effects of the medial meniscus’ posterior root tear were assessed by Allaire et al. [9]. They showed that a posterior root tear of the medial meniscus causes considerable alterations in the contact pressure and the kinematics of the knee joint. Exercise is one of the most effective treatments for osteoarthritis and is crucial for reducing knee pain, improving muscular strength and endurance, increasing activity level, and improving quality of life in osteoarthritis patients [28,29]. According to one study, performing physical activity 3 times per week for 4 months can enhance knee function by more than 35% [28]. We think that our patients’ functional abilities improved as a result of physical activity. However, it is not apparent if there were any pain alleviation results from using non-steroidal anti-inflammatory drugs, physical exercise, or both.
The study Group A which has MMRT pull-out repair had better functional and radiological outcome than the conservative treatment group. Meniscal repair aided the slowing of arthritic changes compared with conservative group; however, it did not prevent the progression of arthrosis completely.
For patients with medial meniscal root tears, surgical repair should be considered the preferred treatment option, especially in those who are younger and active, as it provides superior functional recovery and helps preserve joint health. Conservative management may be appropriate for select patients with lower activity levels or significant surgical risks, but it often results in poorer long-term outcomes, including increased risk of osteoarthritis.
References
- 1.Bessette GC (1992) The meniscus. Orthopedics 15:35–42 [Google Scholar | PubMed]
- 2.Petersen W, Tillmann B (1998) Collagenous fibril texture of the human knee joint menisci. Anat Embryol (Berl) 197:317–324 [Google Scholar | PubMed]
- 3.Johnson DL, Swenson TM, Livesay GA, Aizawa H, Fu FH, Harner CD (1995) Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy 11:386–394 [Google Scholar | PubMed]
- 4.Shino K, Hamada M, Mitsuoka T, Kinoshita H, Toritsuka Y(1995) Arthroscopic repair for a flap tear of the posterior horn of the lateral meniscus adjacent to its tibial insertion. Arthroscopy 11:495–498 [Google Scholar | PubMed]
- 5.Petersen W, Forkel P, Feucht MJ, Zantop T, Imhoff AB, Brucker PU (2014) Posterior root tear of the medial and lateral meniscus. Arch Orthop Trauma Surg 134:237–255 [Google Scholar | PubMed]
- 6.Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM (1999) Meniscal movement. An in vivo study using dynamic MRI. J Bone Joint Surg Br 81:37–41 [Google Scholar | PubMed]
- 7.Magee T, Shapiro M, Williams D. MR accuracyand arthroscopic incidence of meniscal radialtears. Skeletal Radiol 2002; 31:686–689 [Google Scholar | PubMed]
- 8.Bin SI, Kim JM, Shin SJ (2004) Radial tears of the posterior horn of the medial meniscus. Arthroscopy 20:373–378 [Google Scholar | PubMed]
- 9.Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am 90:1922–1931 [Google Scholar | PubMed]
- 10.Forkel P, Herbort M, Schulze M, Rosenbaum D, Kirstein L, Raschke M, Petersen W (2013) Biomechanical consequences of a posterior root tear of the lateral meniscus: stabilizing effect of the meniscofemoral ligament. Arch Orthop Trauma Surg 133:621–626 [Google Scholar | PubMed]
- 11.Forkel P, Herbort M, Sprenker F, Metzlaff S, Raschke M, Petersen W (2014) The biomechanical effect of a lateral meniscus posterior root tear with and without damage to the meniscofemoral ligament: efficacy of different repair techniques. Arthrosc J Arthros Relat Surg 30:833–840 [Google Scholar | PubMed]
- 12.Kim JG, Lee YS, Bae TS, Ha JK, Lee DH, Kim YJ, Ra HJ (2012) Tibiofemoral contact mechanics following posterior root of medial meniscus tear, repair, meniscectomy, and allograft transplantation. Knee Surg Sports Traumatol Arthrosc 21:2121–2125 [Google Scholar | PubMed]
- 13.Ahn JH, Kim SH, Yoo JC, Wang JH (2004) All-inside suture technique using two posteromedial portals in a medial meniscus posterior horn tear. Arthroscopy 20:101–108 [Google Scholar | PubMed]
- 14.Ahn JH, Wang JH, Lim HC, Bae JH, Park JS, Yoo JC, Shyam AK (2009) Double transosseous pull out suture technique for transection of posterior horn of medial meniscus. Arch Orthop Trauma Surg 129:387–392 [Google Scholar | PubMed]
- 15.Ahn JH, Wang JH, Yoo JC, Noh HK, Park JH (2007) A pull out suture for transection of the posterior horn of the medial meniscus: using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc 15:1510–1513 [Google Scholar | PubMed]
- 16.Kim YM, Rhee KJ, Lee JK, Hwang DS, Yang JY, Kim SJ (2006) Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy 22(795):e791–e794 [Google Scholar | PubMed]
- 17.Kim SB, Ha JK, Lee SW, Kim DW, Shim JC, Kim JG, Lee MY (2011) Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy 27:346–354 [Google Scholar | PubMed]
- 18.Lee JH, Lim YJ, Kim KB, Kim KH, Song JH (2009) Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year followup. Arthroscopy 25:951–958 [Google Scholar | PubMed]
- 19.Moon HK, Koh YG, Kim YC, Park YS, Jo SB, Kwon SK (2012) Prognostic factors of arthroscopic pull-out repair for a posterior root tear of the medial meniscus. Am J Sports Med 40:1138–1143 [Google Scholar | PubMed]
- 20.Lerer DB, Umans HR, Hu MX, Jones MH (2004) The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol 33:569–574 [Google Scholar | PubMed]
- 21.Hunter DJ (2011) Osteoarthritis. Best Pract Res Clin Rheumatol 25:801–814 [Google Scholar | PubMed]
- 22.Jones AO, Houang MT, Low RS, Wood DG (2006) Medial meniscus posterior root attachment injury and degeneration: MRI findings. Australas Radiol 50:306–313 [Google Scholar | PubMed]
- 23.Shepard MF, Hunter DM, Davies MR, Shapiro MS, Seeger LL (2002) The clinical significance of anterior horn meniscal tears diagnosed on magnetic resonance images. Am J Sports Med 30:189–192 [Google Scholar | PubMed]
- 24.Rennie WJ, Finlay DB (2006) Meniscal extrusion in young athletes: associated knee joint abnormalities. AJR Am J Roentgenol 186:791–794 [Google Scholar | PubMed]
- 25.Lee SY, Jee WH, Kim JM (2008) Radial tear of the medial meniscal root: reliability and accuracy of MRI for diagnosis. AJR Am J Roentgenol 191:81–85 [Google Scholar | PubMed]
- 26.Van Dyck P, Gielen J, D’Anvers J, Vanhoenacker F, Dossche L, Van Gestel J, Parizel PM (2007) MR diagnosis of meniscal tears of the knee: analysis of error patterns. Arch Orthop Trauma Surg 127:849–854 [Google Scholar | PubMed]
- 27.Choi NH, Son KM, Victoroff BN (2008) Arthroscopic all-inside repair for a tear of posterior root of the medial meniscus: a technical note. Knee Surg Sports Traumatol Arthrosc 16:891–893 [Google Scholar | PubMed]
- 28.Petersen W, Zantop T (2006) Avulsion injury to the posterior horn of the lateral meniscus. Technique for arthroscopic refixation. Unfallchirurg 109:984-987 [Google Scholar | PubMed]
- 29.Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am 90:1922–1931 [Google Scholar | PubMed]
- 30.Herrlin S, Hallander M, Wange P, Weidenhielm L, Werner S (2007) Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc 15:393–401 [Google Scholar | PubMed]
- 31.Mangione KK, McCully K, Gloviak A, Lefebvre I, Hofmann M, Craik R (1999) The effects of high-intensity and low-intensity cycle ergometry in older adults with knee osteoarthritis. J Gerontol A Biol Sci Med Sci 54:M184–190. [Google Scholar | PubMed]